26. Liver Anatomy Flashcards
Label A-D
What does the highest part of the diaphragm go up to?
4th intercostal space
A: hepatic flexure
B: fundus
C: lesser omentum
D: falciform ligament
Are all the parts of the duodenum retroperitoneal or intraperitoneal?
What is the liver divided into anatomically and surgically?
D1: starts intraperitoneal and becomes retroperitoneal
D2 and D3: retroperitoneal
D4: starts retroperitoneal and becomes intraperitoneal
Anatomically = lobes: L (larger) and R (smaller) divided by falciform ligament, caudate and quadrate. Surgically = Couinards classification of 8 diff lobes each with own vascular inflow and outflow and biliary drainage (can resect area without damaging remaining)
Label A-E on the visceral surface of the liver
What structres does D contain?

A: quadrate lobe (square shape)
B: caudate lobe (has tail)
C: ligamentum venosum
D: porta hepatis <em>(deep fissure in the inferior surface of the liver through which all the neurovascular structures (except hepatic veins) and hepatic ducts enter or leave the liver)</em>
E: IVC
Portal triad: bile duct + hepatic artery proper + portal vein, and lymph nodes and autonomic fibres

What is the ligamentum venosum?
What is the ligamentum teres/round ligament?
Remnant of the ductus venosus in the foetus: shunts L umbilical vein blood flow directly to IVC (b/c placenta does most of the liver’s function). Becomes fibrous remnant in adult.
Remnant of umbilical vein
Does peritoneum cover the liver?
Where does the lesser omentum arise from?
What are the 4 ligaments (peritoneal reflections) that hold the liver to other structures?
When the liver develops, what 2 ligaments are found either side of it?
Not all of it - small bare posterior area
Porta hepatis and ligamentum venosum (to lesser curvature of stomach)
Coronary (ant and post), R and L triangular, falciform
Falciform at front and lesser omentum between liver and stomach

What are A-C, and what are they seen here through?

A: portal vein
B: hepatic artery
C: bile duct
Free border of lesser omentum (anterior to epiploic foramen). NB. lesser omentum = hepatoduodenal and hepatogastric ligaments
What is the Pringle manoeuvre?
Describe the blood supply to the liver, and give the percent of delivery from the 2 main arteries.
Clamping of hepatoduodenal ligament (free border of lesser omentum) - clamps off hepatic artery and portal vein if want to repair liver.
Blood supply: pic
Coeliac trunk = 25%, hepatic portal system of veins = 75%

Describe the hepatic portal system of veins.
What are the 4 important sites of porto-systemic anastomoses?
Splenic and superior mesenteric veins meet posterior to head of pancreas to form portal vein.
Lower oesophagus, umbilical, retroperitoneal, ano-rectal junction

What is liver cirrhosis?
What is portal hypertension (give normal and PH value)?
What might happen to the spleen if a pt has portal hypertension?
Consequence of chronic liver disease characterised by replacement of liver tissue by fibrosis, scar tissue and regenerative nodules, leading to loss of liver function. 10 cause of portal hypertension b/c blood can’t perfuse through liver properly so BP in portal vein affected.
Normal portal pressure = 9mmHg. IVC = 2-6mmHg. PH usually when portal pressure gradient is >10 (i.e. diff between IVC and hepatic portal system >10). If liver fibrous, blood can’t go through it properly and builds up pressure in portal syste, first in hepatic portal vein and then in superior and inferior mesenteric veins.
Splenomegaly - higher portal pressure = spleen engorged with blood - not draining through liver as easy as it should.
Porto-systemic anastamoses come into play…
Describe how oesophageal varices form.
What may pts with this condition present with, and how may they be treated?
Where, specifically, do oesophageal varices form?
Normal = lower oesophagus drainage towards L and R gastric veins -> portal vein. If PH = pressure increase in these vains so blood won’t go in portal system as easily, so follows path of least resistance = through oesophageal venous plexus to caval system. Used as shunt after a while so superficial veins become distended and engorged = oesophageal varices at distal oesophagus.
Haematemesis, treat with gastric banding
Anastamoses of L gastric vein with oesophageal veins at gastro-esophageal junction.
What can you see here?

L: oesophageal varices v. obvious
R: splenomegaly
What is ascites?
List 3 main causes.
What is caput medusae?
Excess fluid in peritoneal cavity.
1) portal hypertension, 2) hypoalbuminemia (albumin helps regulate oncotic balance), 3) aldosterone related renal Na+ retention, with consequent blood volume expansion
Recanalised umbillical vein within the falciform ligament. Paraumbilical veins radiate superiorly to intercostal veins and inferiorly to the inferior epigastric vein.
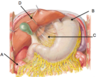
What can you see here?

Red arrow and A: ascites
B: gallbladder
What is retroperitoneal hemorrhage?
How are hemorrhoids different from anal-rectal varices?
Retroperitoneal organs (DR PAD: duodenum, rectum, pancreas, ascending and descending colon) have veins behind which either drain backwards to lumbar veins or forwards to portal system. If portal hypertension -> path of least resistance so drain through lumbar veins = RH = veins in retroperitoneal space -> rupture = blood accumulation
Hemorrhoids: vascular area around anal canal where venous sinusoids expand. 3 anal cushions help keep anus closed and maintain continence. Small veins become engorged and damaged.
Ano-rectal varices: occur higher up at ano-rectal junction. Form due to portal hypertension and portosystemic shunts. Bleed massively.
Describe the blood supply and venous drainage of the recto-anal junction:
a) above pectinate line
b) below pectinate line
- (Pectinate line (dentate line) divides upper two thirds and lower third of anal canal)*
a) superior rectal artery (branch of superior mesenteric), superior rectal vein (drains to inferior mesenteric vein (hepatic portal system)). Columnar epith
b) inferior rectal artery and vein (branch of/drains to internal iliac artery/vein (systemic)). Stratified squamous epith