2. Functional Histology of the Gut Flashcards
What are the 3 functional compartments of the alimentary tract?
1) Oral cavity: ingestion and fragmentation. Stratified squamous epithelium. Salivary glands (amylase)
2) Simple passages: oesophagus and anus - transport. Stratifed squamous epithelium.
3) Digestive tract: stomach and intestines. Digestion and absorption. Enterocytes. Mucosal and accessory glands incl. pancreas and liver.
Epithelium structure changes along alimentary tract.
Briefly describe the process of nutrient absorption/excretion from ingested food, from top to bottom.
Fragmentation (oral cavity + stomach, aided by saliva) -> Digestion (stomach (acid environment, mechanical breakdown) + duodenum (pancreatic and brush border enzymes, bile salts)) -> Absorption (most jejunim + ileum, enterocytes absorb to capillaries and lacteals) -> Elimination (colon + anal canal, lq residue, H2O absorbed, solid faeces expelled)
Absorbed lipids to lymphatic capillaries don’t go through liver processing unlike the nutrients absorbed into blood capillaries.
What are the 4 main layers of the gut wall (and their divisions, if any)?
Is the mucosa the same throughout the alimentaery tract?
1) Mucosa: epithelium, lamina propria, muscularis mucosae
2) Submucosa
3) Muscularis propria/externa: circular, longitudinal
4) Adventitia/serosa: CT, mesothelium
No - varies with region/function e.g. at the oesophageal - gastric junction, simple columnar epithelium of stomach -> stratified squamous epithelium of oesophagus.

Describe the submucosa.
Describe the muscularis propria/externa.
When is it called the adventitia or serosa?
Thick layer of fibrocollagenous, loose CT. Shock absorbing. Contains BV, lacteals, submucosal neural plexus = parasympathetic innervation. Nerves project up to lamina propria and regulate secretion etc.
SM layers, inner circular and outer longitudinal (work together to produce unidirectional peristalsis). Contains myenteric plexus.
Adventitia is where the gut is retroperitoneal - most of oesophagus, duodenum, ascending and descending colon and rectum.
Describe the 2 consistant portions throughout the gut wall.
1) Enteric NS: autonomous functioning ganglia, inputs from parasympathetic and sympathetic NS, spinal sensory afferents: submucosal plexus innervates muscularis mucosae and mucosal glands, myenteric plexus innervates muscularis propria.
2) MALT/GALT: intraepithelial lymphocytes (detect antigens in lumen), lymphocytes and plasma cells of lamina propria - IgA production and lymphoid follicles. Peyer’s patches = collections of lymphoid tissue found in ileum, helps regulate gut flora.

Where along the alimentary tract are A-D found? List some properties of each.

A: oesophagus: protective, thick, multiple layeres (stratified squamous)
B: stomach: secretory, long glands
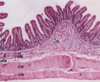
C: Small intestine: secretory/absorptive, protrusions into lumen + lamina propria, crypts at base of vili
D: Large intestine: absorptive/protective, no villi, no protrusions = flat surface
List the locations food passes through as it goes down the alimentary tract.
What does swallowing involve?
What kind of mucosa is found in the oesophagus?
What does the oesophageal submucosa contain?
What is the oesophageal muscularis propria like?
Does the oesophagus have adventitia or serosa?
Mouth -> oropharynx -> oesophagus -> stomach (cardia, fundus, body, pylorus) -> small intestine (duodenum, jejunum, ilium) -> large intestine (ascending, transverse, descending, sigmoid) -> anus
Relaxation of cricopharyngeal part of cricopharyngeus.
Non-keratinised stratified squamous epithelium
Mucous glands (=lubrication), BVs, nerves and ganglion cells (submucosa enteric plexus), lymphoid tissue
Top 1/3 skeletal muscle (swallowing), bottom 1/3 SM (peristalsis)
Adventita
What happens at the oesophagogastric junction?
What does the stomach do?
Abrupt change in mucosa (stratified squamous -> simple columnar/glandular mucosa), site of physiological sphincter preventing reflux: oesophagus joins at acute angle, diaphragm contraction, intra-abdominal pressure on oesophagus > intragastric pressure, unidirectional peristalsis
Aids in mechanical and chemical digestion: glandular mucosa produces gastric juice which helps reduce contents to chyme (also enzymes inc. pepsin). Mucosa is covered by a thick protective layer of mucous.

Distinguish between the oesophagus and stomach on
a) an autopsy
b) an endoscopic view towards the stomach
a) Oesophagus = thick stratified epithelium (white)
b) Stomach = columnar epithelium, BV go right up to it so can see stomach darker b/c of BVs

What are the parts of the stomach?
What is a rugae?
What two things are found in the mucosa?
How is the stomach lining protected?
How is the stomach muscularis propria different?
Cardia, fundus, body, pylorus
Fold - when stomach is empty it folds up on itself (not permanent)
Gastric glands, open up into gastric pits.
Mucus secreting cells (columnar surface and mucous neck cells - not goblet cells) secrete protective alkaline mucus.
3 layers instead of 2: inner oblique, middle circular, outer longitudinal

What kind of gastric glands are found in:
a) the cardia
b) the fundus/body
c) the pylorus
State what they secrete.
a) mucous neck cells (mucus - diff to gastric pit mucus)
b) mucous neck cells (mucus), parietal cells (HCl, IF. Activate pepsinogen to pepsin), chief cells (make pepsinogen), endocrine cells (secretes hormones e.g. gastrin -> modulates molitlity of gut)
c) mucous neck cells (mucus), endocrine cells (gut hormones incl. gastrin).
STEM CELLS regenerate epithelium.
NB: mucus secreting cells = clear staining. Parietal cells look like fried eggs due to HCl prod. (pic).

What is the pyloric sphincter?
Describe the 3 areas of the small intestine.
At the gastroduodenal junction there is marked thickening of circular layer of muscularis propria.
Duodenum: digestion. Brunner’s glands: in submucosa, secrete thin alkaline mucous in response to luminal chyme. Receives bile and pancreatic juice via Ampulla of Vater, controlled by Sphincter of Oddi. Mainly retroperitoneal (2nd and 3rd parts)
Jejunum: most absorption occurs here. Most specialisation to increase SA.
Ileum: absorption. Greatest development of MALT = Peyer’s patches
What 3 things does the small intestine have to increase the SA for absorption?
List the contents of lamina propria of villi.
1) Plicae circulares: circular folds increasing submucosa in jejunum and ileum
2) Villi: mucosa extensions, central core of lamina propria, Crypts of Lieberkuhn at bases)
3) Microvilli: apical processes on cells = ‘brush border’, aids terminal digestion of proteins and carbs - peptidases and disaccharidases.
Areolar CT, strands of SM from muscularis mucosae, MALT, Capillaries, Central lacteal, Nerve fibres

What are the epithelial cells of the small intestine? (location + function).
1) Enterocyte: lining villus (digestion, absorption) and in crypt (secretion of watery interstitial juice)
2) Goblet cell: scattered along villus between enterocytes - increased numbers distally (mucus)
3) Endocrine cell: crypt (regulation of gut function)
4) Stem cell: crypt (regeneration of epithelium)
5) Paneth cell: crypt (antimicrobial agents - lysozyme etc.) - ensure gut flora maintained
What is G in the duodenum?
Brunner’s Glands, produce mucus-rich alkaline secretion
What is the yellow arrow pointing to in the small intestine?

Peyer’s patches (GALT) - lymphoid follicles for protection, lymphocytes make it blue.
Note the submucosa going outwards, plicae circulares
What happens in the large intestine?
How is it specialised?
Specialised for salt and water absorption (enterocytes) and mucus secretion (abundant goblet cells).
No villi (only tubular glands composed of enterocytes). Incresed proportion of goblet cells relative to absorptive enterocytes. Outer longitudinal muscularis propria organised to 3 bundles = taenia coli - sacculate colon forming haustra. Poterior aspects of ascending and descending segments are retroperitoneal therefore covered by adventitia (rest is serosa).
Label A and B in the large intestine.

A: tubular glands in mucosa (don’t stain well b/c lots of goblet cells there).
B: MALT/GALT
Note thin line of muscularis mucosae.
Where are the following mucosa found?

A: small intestine - villi in crypts
B: oesophagus - stratifed squamous epithelium
C: stomach - thick mucosa and glandular portion at top, see gastric pits and extended glandular portions
D: large intestine - colon, simple tubular glands with lots of goblet cells


