1 - Mediastinum and Embryology Flashcards
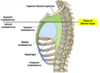
Superior Border of the Mediastinum
(Post) T1 - 1st Rib - Sup Manubrium (Ant)
Thoracic Inlet
Inferior Border of Mediastinum
Thoracic Outlet
(post) T12 - Diaphragm - Sternum (Xiphoid) (Ant)
Lateral Borders of Mediastinum
Formed by Mediastinal Parietal Pleura
Superior vs Inferior Mediastinum
Division Landmark?
Sub-Divisions?
Landmark: Plane of Sternal Angle (Between T4-T5 Vertebrae)
Within Inferior Mediastinum, you have the Anterior, Middle, and Posterior Mediastinum
Contents of the Divisions of Mediastinum:
Anterior
Area between pericardium and sternum
Contents: Thymus Gland, Lymph Nodes (tumor metastasis), Sternopericardial Ligaments
Contents of the Divisions of Mediastinum:
Middle
Contents:
- Heart w/in Pericardial Sac (part of coelomic cavity)
- Ascending Aorta
- Pulmonary Trunk + branches
- Seven Veins; Superior Vena Cava, termination of Azygous Vein, termination of Inferior Vena Cava, Four pulmonary veins (L Atrium)
- Phrenic Nerve
- Pericardiacophrenic Artery/Vein
- Mediastinal Lymph Nodes
Contents of the Divisions of Mediastinum:
Posterior
Contents: Located between heart and lower 8 thoracic vertebrae
Contains tubular structures (esophagus, aorta)
Thymus Gland
Mainly superior mediastinum, but can extend into Anterior during fetal/childhood
After puberty, begins to degrade
Clinical: Lymph nodes of Anterior Mediastinum
Potential site for tumor metastases
Seven Veins
Located in Middle Mediastinum
- Superior Vena Cava
- Azygous Vein
- Inferior Vena Cave
4-7: Pulmonary Veins
Phrenic Nerve:
Location
Type of Innervation
C3/4/5
Anterior to Root of Lung
- Motor: Diaphragm
- Sensory: Mediastinal Pleura, Pericardium, Pleura, Peritoneum
Pericardiacophrenic A. / V.
Branch of Internal thoracic artery and vein
Courses with Phrenic N. to supply pericardium/diaphragm
Contents of the Divisions of Mediastinum:
Middle
- Pericardium
- Pericardial Cavity
Fibrous Pericardium
Apex
Base
Posteriorly
Conical shaped sac, limits movement of heart
Apex: Pieced by asecning aorta, superior vena cava, pulmonary trunk
Base: Fused with central tendom of diaphragm, pierced by inferior vena cava
Posteriorly: Pierced by four pulmonary veins
Fibrous Pericardium: Anchor Points
Superior/Posterior
Inferior
Anterior
Superior / Posterior: Blends with tunica adventitia of great vessels
Inferior: Central tendon of diaphragm
Anterior: Sternopericardial Ligaments
Fibrous Pericardium:
Structure
Borders
Embryology
Structure: Inelastic–will NOT expand; blood can build up in the sac due to tear in heart/vessel
Borders: Follows heart, except on RIGHT side, extends up to Second Costal Cartilage (heart ends at third)
Embryology: Drived from Body Wall (Somatic) Mesoderm of Lateral Plane
Clinical: Pericardial Effusion and Cardiac Tamponade
Treatment?
Locations?
Pericardial Effusion: Excess fluid in the pericardial sac
Cardiac Tamponade: Compression of heart due to rapid accumulation of excess fluid
Treatment = Pericadiocentesis
- Parasternal Approach - Left 4th or 5th Intercostal Space
- Subxiphoid Approach - Left Xiphoid, angled posterior, superior at 45o angle
Serous Pericardium: Two Layers?
Parietal Layer - Inner surface of fibrous pericardium, inseparable from fibrous layer
Visceral Layer - Outer surface of heart, forms epicardium of the heart; continuous w/parietal layers by reflecting onto great vessels
Pericardial Cavity
Definition?
Sub-regions?
Potential space between serous parietal and serous visceral pericardia; contains thin film on serous fluid
- Transverse Pericardial Sinus
- Oblique Pericardia Sinus
Transverse Pericardial Sinus
Clinical?
Between the Superior Vena Cava (posterior) and the ascending aorta/pulmonary trunk (anterior)
Serves as surgical landmark between these vessels.
Clinical: Method of separation of arteries from veins for ligation during surgery, bypass, etc.
Oblique Pericardial Sinus
Blind space bwteen the left atrium and the posterior wall of the pericardial sac
Formed by reflections of serous pericardium from pulmonary veins of the heart
Embryology: What creates the single, continous Coelomic Space?
What septae are formed by this?
Lateral folding of embryo
Pleuropericardial Membranes
Diaphragm
Embryology: How does separation of the Pleural and Pericardial Cavities occur?
What is formed by fusion of the right and left pleuropericardial membranes?
Rapid development of the lung buds drives splitting of inner somatic mesoderm layer, foming layer to separate pleural and pericardial cavities
Pleuropericardial membranes are somatic mesoderm layers (paired) that split from wall to envelop heart and form fibrous pericardium
Embryology: What occurs as the pleuropericardial membranes grow toward eachother?
What is the divisional result?
Fuse to form fibrous pericardium
Divides thoracic cavity into three spaces, each with visceral and parietal layers
- Ventral Pericardial Cavity (Heart)
2/3. Two Pleural Cavities (Lungs)
Embryology: What are the four sources of the Diaphragm?
- Septum Transversum
- Paired Pleuroperitoneal Membranes
- Dorsal Mesentery of the esophagus
- Myoblasts from somatic mesoderm of body wall
Embryology: What structure contains the phrenic nerve?
Pleuropericardial membranes (2x) as the develop from the body wall; which eventually fuse to form Fibrous Pericardium
Embryology: Septum transversum
Plate of mesoderm that incompletely separates the thoracic cavity from abdominal cavitity; forms central tendon of diaphragm
Embryology: Right and Left Pericardioperitoneal Canals
Coelomic spaces that link the thoracic and abdominal coelomic cavities–located alongside the foregut
Embryology: Pleuroperitoneal Membranes
Paired layers of somatic mesoderm, at the caudal border of the pleural cavities (lungs)
Will fuse with Septum Tranversum and the dorsal mesentery of the esophagus thus closing the pericardioperitoneal canals (sealing pleural/peritoneal cavities)
Embryology: What forms the crura (legs) of the diaphragm?
Dorsal mesentery of the esophagus
Embryology: What type of cells contribute to the muscles of the diaphragm?
Myoblasts from somatic mesoderm of body wall
Embryology: How does positional change affect the innervation of the diaphragm?
Septum Transversum begins at level of cervical somites and nerve fibers of C3/4/5 (phrenic nerve), grow into septum
Due to rapid growth of CNS, Phrenic Nerve is dragged inferiorly
Embryology: What coveres periphery innervation of the diaphragm?
Lower Intercostal Nerves (Parietal Pleura/Parietal Peritoneum) as it comes from the thoracic body wall
Clinical: Congenital Defects of Diaphragm
Congenital Diaphragmatic Hernia (Foramen of Bochdalek)
Failure of pleuroperitoneal membrane (90% on left side) to form/fuse with other contributions of diaphragm
Abdominal contents can enter thoracic cavity, compressing lungs
1:2000 births, high mortality rate
Clinical: Congenital Defects of Diaphragm
Esophageal Hiatal Hernia
Herniation of stomach through enlarged esophageal hiatus of the diaphragm
Stomach contents reflux into the esophagus since sphincter is nonfunctional
Infant will vomit when laid on back after feeding
Clinical: Congenital Defects of Diaphragm
Foramen of Morgagni or Parasternal Hernia
Herniation of abdominal visceral (sternocostal hiatus) space which surround the Superior Epigastric Artery, as the artery pierces the sternocostal portion of diaphragm
Normally small hole, defect makes it larger


