Week 5: Anatomy and Histology of the Kidney Flashcards
Where are the kidneys located?
retroperitoneally
What are the 6 functions of the kidneys?
The main function of the kidneys is the production of urine
It also excretes metabolic wastes
It is in charge of regulation of water and acid-base balance of the blood
It regulates body fluid osmolarity and electrolyte concentration
Regulates arterial pressure
Secretes hormones
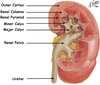
what are the 3 regions of the kidney
The cortex- contains nephrons, medulla- and pelvis

describe the blood supply of the kidneys

what are the two main components of the nephron and what do they contain?
Corpuscle
This is comprised of a glomerular tuft (which are spherical structures that get bigger the closer they get to the medulla)
This glomerular is encapsulated by bowman’s space, which is held together by bowman’s capsule
Tubule
Contains PCT, Descending limb, DCT

what are the two different types of nephrons and where are they located in the kidneys?
Juxtamedullary
Because they exist closer to the medulla (closer to the centre)
These have a long thin loop of Henle
The blood vessels that supply the loop of Henle are known as the Vasa Recta
Cortical
Have shorter loops of Henle
Exist in the outer cortex

Describe the structure of the renal corpuscle
Is comprised of a glomerulus that is surrounded by bowman’s capsule

In relation to the glomerulus, this structure is made up by a penetrating afferent arteriole (the bigger of the two) which forms the capillary network (the glomerulus), and then leaves as the efferent arteriole
Where these structures enter the renal corpuscle is known as the vascular pole
Opposite this is the urinary pole which drains the filtrate from the podocytes into the proximal convoluted tubule
What are the 3 types of cells in the glomeruli and their function
Podocytes
These are parietal cells that line the outside of capillaries
These are quite large cells with foot processes that reach out and interlock with each other
The little gaps between each of these interlocking foot processes is where the fluid will pass through (whilst stopping large structures like proteins)
Mesangial cells
Are the cell that structural supports the glomerular tuft
These are the cells that bind two capillaries together, providing structural support to the capillaries
These are less important in terms of filtration
Endothelial cells
Is the lining of the capillaries that forms part of the filtration barrier
It has a very spotty appearance, which actually are tiny holes known as fenestrations

Describe the histology of the PCT
Is made up of simple cuboidal epithelium
These have a special apical cell surface specialisation of microvilli, or finger like projections that reach into the tubule (which stain a very light pink)
These are usually referred to as a brush border (makes the lumen very messy)
This plays a major role in reabsorption
Have a ‘brush border’ which is the bright pink border which are thousands of micro villi à trying to increase surface area

describe the histology of the loop of henle
Simple squamous epithelium
There are thick and thin descending limbs, a hairpin turn, then a thin ascending limb before it expands to a thick ascending limb
Those nephrons that are close to the medulla (or juxtamedullary nephrons) have particularly long loops of Henle (as opposed to those in the cortex that are little)
Is heavily involved in water retention
different regions have different permeabilities to water
Describe the histology of the DCT
Cuboidal
Is the last segment of the nephron
It has no brush border, it is important in acid-base balance
It is the site of ion exchange
Site of salt and water regulation
This then connects to the collecting duct (which is not part of the nephron)
Has macula densa (or juxtamedullary) cells
In a nephron, which 3 structures are in the cortex and which 3 are in the medulla
The structures that are contained within the cortex are (left side of image);
Renal Corpuscle (glomerular tuft, bowmen’s space and bowman’s capsule)
Post convoluted Tubules
Distal convoluted Tubule
The structures that are contained within the medulla are (right side of image);
Loop of Henle
Collecting ducts
Vasa Recta
what are the 3 types of kidney variations
Fused ectopia (when kidneys fuse into one)
Horseshoe kidneys (when they are joined inferiorly by either kidney tissue or fibrous tissue). These result in higher rates of;
Obstructions and infections
Trauma (road accidents from seat belt)
Recurrent calculus
Pancake tissue is when both are joined inferiorly and superiorly creating one large shape. These result in higher rates of;
Uteropelvic junction obstruction
Recurrent infection
Recurrent calculus
Increased malignancy incidence

What are the macula densa cells, where are they located and what is their function?
These are special cells which line the distal convoluted tubule as it comes into close proximity to the afferent arteriole
These cells detect salt levels within the distal convoluted tubule, an elevated amount of sodium within the filtrate will then tell the afferent arterioles to constrict (reducing the amount of blood going through the capillaries, reducing the filtration rate of salt)
At the same time these cells tell the juxtaglomerular cells to produce renin, which will increase blood pressure through the renin-angiotensin aldosterone system
Describe the 3 sets of nephric structures to develop of kidneys
Pronephroi: transient, no excretory capacity, continuous with Wolffian duct, degenerates
Mesonephroi: excretory organs, open into Wolffian ducts and cloaca, function briefly, have glomeruli and tubules, degenerate end of 1st trimester (in males become efferent ductules of testes)
Metanephroi: produces urine week 10, excreted into amniotic cavity, permanent kidneys from uretic bud and metanephric mesenchyme

what does the uretic bud give rise to?
CD, calcyes, renal pelvis and ureter
what does the metanephric mesenchyme give rise to?
nephron and interstitium
Describe nephrogenesis
Induced by signals form ureteric epithelium
Renal vesicle forms à into nephron
Capillary becomes associated with nephron
What positional change do the kidneys undergo?
rotate 90 degrees.
What is characteristic about the ureter as they enter the bladder and what is the clinical significance of this?
The ureters descend to the base of the bladder where it turns medially and obliquely through the posterior bladder wall (an important structural mechanism which prevents backflow)
This backflow is prevented by the contraction of the smooth muscle of the bladder
As the urinary bladder fills, it compresses the ureter. (See diagram)
This function protects the kidney from spread of infections

Where are the 3 locations that renal calculi (kidney stones) may lodge?
Where the renal pelvis narrows is the region that the ureter begins, and is one potential zone where a renal calculi or kidney stone may lodge
Further down, the region where the ureter passes over the pelvic brim, and passes over the external iliac artery and vein, there is opportunity for kidney stones to lodge due to a slight kink
Where it passes through the bladder wall itself

What type of epithelium line the major calyces, renal pelvism ureters, bladder and urethra?
Transitional epithelium


Why do males have increase accuracy of urination?
These two sphincters (internal and external) open in opposite directions, this creates a spiralling effect of urine which increases accuracy of urination (like a bullet out of a gun)
Describe the histology of the male urethra
Starts out as transitional epithelium and then becomes stratified columnar and then towards the distal end it becomes stratified squamous
how long is the male urethra and female urethra?
What is the clinical significance of the length of the female urethra
20 cm and 4 cm
due to short length -much more prone to infection (e.g. e-coli during poor wiping.)

describe the histology of the female urethra
stratified colomnar epithelium
which kidney sits more cranially and why?
left sits higher than right as the right needs to make room for the liver
what are two functions of the type of epithelium that lines the ureter and what epithelium is it?
transitional epithelium, allows for stretch and prevents against toxicity of urine
why are women more susceptible to bladder infections
urethra only 4cm long
what components of the kidney are derived from the metanephric mesenchyme?
nephron and intersitium
what is the part of the medulla which is made up of a collection of tubules which drain into the minor calyx?
Renal pyramid


