Week 2: Haemostasis Flashcards
Define hemostasis in your own words
The process of blood clotting and desolution after tissue repair
Fill the blanks
- artery 2. vein 3. valve 4. endothelium of tunica intima 5. connective tissue (collagen + elastin) 6. tunica media 7. tunica adventitia

Which are the plasma componenets of hemostasis?
-coagulation and fibrinolytic proteins - inhibitors of coagulation and fibrinolytic proteins
Which are the main elements that act in primary hemostasis?
Blood vessels and platelets
Briefly describe primary hemostasis
Minor injury to blood vessels exposes collagen -> platelets bind to collagen via vWF and release platelet factors -> platelet factors trigger vasoconstriction -> platelets aggregate and attract further platelets to agglutinate and form a plug
Briefly describe secondary hemostasis
Platelet factors start the coagulation cascade and fibrinogen is converted to fibrin to form a stabilising ‘bandage’ over the plug
What are the three main stages of hemostasis?
1) Vasoconstriction 2) Platelet plug formation 3) Coagulation
Describe some of the elements involved in the vasoconstriction phase
Only in small vessels: - reflex reaction from smooth muscle - thromboaxane A2 (TXA2) + serotonin contribute - endothelin (strongest constrictor) released from endothelial cells
What kind of granules contain: fibrinogen, vWF, fibronectin, factors V and VIII, and PDGF?
alpha granules
What kind of granules contain: ADP, ATP, Ca2+, histamine, serotonin, epinephrine?
delta (dense) granules
Name some platelet factors outside of alpha and delta granules
glycoproteins, phospholipids, actin, myosin, thrombasthenin, TXA2
Which platelet factors allow platelet adhesion?
vWF
Which platelet factors allow platelet aggregation?
ADP, TXA2
Run through the steps of platelet plug formation including some of the platelet factors and how they affect the process
- free vWF from plasma leaks into damaged blood vessel tissue - vWF attaches to collagen and allows binding of platelets - platelets stick to vWF via surface receptor GpIb - adhesion causes conformational change from smooth discs to spike spheres, exposing glycoprotein receptors on platelet surface (GpIIb and GpIIIa) - conformational change causes the release of ADP, TXA2, and serotonin - ADP and TXA2 stimulate aggregation of platelets - platelets adhere to each other via fibrinogen, which is bound to surface receptor complex GpIIb-IIIa on each platelet - platelet plug is formed
How does the endothelial cell stop adhesion of platelets in a healthy blood vessel?
Endothelial cells release prostacyclin -> prostacyclin enters thrombocytes and upregulates adenylate cyclase to produce more cAMP from ATP. cAMP lowers intracellular Ca2+ concentration. Ca2+ is important for adhesion and aggregation processes. Therefore: prostacyclin -> ↑cAMP ->↓ Ca2+ -> ↓ adhesion and aggegation
How does the effect of prostacyclin on platelets compare with the effect of thromboaxane A2?
They are antagonistic. TXA2 increases cytosolic Ca2+ and promotes adhesion, whereas prostacyclin acts the opposite way
What is the trigger for the intrinsic pathway of blood clotting?
Blood coming in contact with a negatively charged surface (collagen, phospholipids from damaged platelets)
What is the trigger for the extrinsic pathway of blood clotting?
Tissue factor released from damaged cells
Are these factors intrinsic, extrinsic or both?

PK - Int HMWK - Int I - Both II - Both III - Ext IV - Both V - Both VII - Ext VIII - Int IX - Int X - Both XI - Int XII - Int XIII - Both
What are the clotting factors’ non-numerical names?

Prekallikrein - Fletcher factor High molecular weight kininogen - contact activation factor I - Fibrinogen II - Prothrombin III - Tissue Factor IV - Calcium V - Proaccelerin, laile factor VII - Proconvertin, serum prothrombin conversion accelerator (SPCA) VIII - Antihemophiliac factor A IX - Christmas factor, antihemophilic factor X - Stuart-Prower factor XI - Plasma thromboplastin antecendent (PTA) XII - Hageman factor XIII - Protransglutaminase, fibrin stabilising factor (FSF), fibrinoligase
Match the regulatory proteins

- von Willebrand factor (vWF) 2. Protein C 3. Protein S 4. Thrombomodulin 5. Antithrombin III
Which are the contact factors and what defines them?
XII, XI, Pre-Kallikrein, HMWK. These are stable in blood and don’t require Ca2+
Which are the VitK dependent factors and what defines them?
II, VII, IX, X. These require vitamin K for synthesis, require Ca2+ for activation and are NOT consumed during coagulation
Which are the Fibrinogen group factors and what defines them?
I (Fibrinogen), V, VIII, XIII. These react with thrombin, are consumed during coagulation and increase during pregnancy
Describe the intrinsic pathway of coagulation
-Contact with collagen or phospholipids from damaged blood cells activates XII -> XIIa -XIIa acts on XI in the presence of HMWK to get XIa - XIa acts on IX in the presence of Ca2+ to get IXa - IXa and VIIIa combine with Ca2+ and phospholipids to form tenase - tenase activates X to get Xa - From here the pathways merge
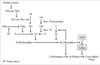
Describe the extrinsic pathway of coagulation
-tissue trauma causes the release of tissue factor aka tissue thromboplastin aka III - III activates VII to get VIIa - III and VIIa combine with CA2+ to form a trimolecular complex which activates X to get Xa -from here the pathways merge

Describe the common coagulation cascade from Xa
- Xa and Va, in the presence of Ca2+, form the prothrombin activator - Prothrombin activator converts prothrombin to thrombin - thrombin converts fibrinogen to fibrin monomers - thrombin together with VIII also activates XIII which stabilises fibrin, in the presence of Ca2+ and aids spontaneous polymerisation of fibrin monomers - fibrin polymers form a mesh and stabilise the clot
Aside from converting fibrinogen to fibrin, how else does thrombin feed into the cascade?
- Thrombin increases activation of V to Va - Thrombin increases activation of VIII to VIIIa - Thrombin increases activation of XI to XIa - Thrombin cleaves VIII from vWF (vWF binds VIII in plasma) - Thrombin catalyses formation of further thrombin from prothrombin - Thrombin causes release of nitric oxide, PGI2, ADP, vWF and tissue plasminogen activator from enothelial cells - Thrombin can act as an anticoagulant with protein C and S
Which pathway is more essential for coagulation?
Extrinsic
Aside from fibrin and platelets, what else is in a clot?
erythrocytes and leukocytes
Describe clot retraction
- 20-60 minutes after formation - squeezing serum from clot - actin and myosin released from platelets pulls edges together
How does tissue factor pathway inhibitor (TFPI) work?
-TFPI combines with the trimolecular complex of III, VII and Ca2+ and inactivates it - This stops extrinsic activation of X
How does thrombomodulin work?
Thrombomodulin is a glycosaminoglycan released by endothelial cells. It binds and inactivates thrombin. It can also combine with protein C
How does protein C work?
- Protein C is activated by thrombin - protein C combines with thrombomodulin-thrombin complex to inactivate thrombin - Protein C together with cofactor protein S binds Va and VIIIa to inhibit the coagulation cascade
Where are protein C and S produced?
In the liver and in endothelial cells
Which nutritional factor is necessary for Protein C and S formation?
VitK
How does antithrombin III work?
- ATIII is present in plasma and the endothelium - ATIII inactivates IXa, Xa, XIa, and thrombin - ATIII can bind with heparin which enhances and accelerates its activity -
What is the role of plasmin?
Plasmin causes degradation of fibrinogen and fibrin
Which are the intrinsic plasminogen activators?
Kallikrein and XIIa
What is the role of plasminogen activators?
They convert plasminogen into plasmin
Which enzyme catalyses the activity of extrinsic plasminogen activators?
streptokinase
Which are the sources of extrinsic plasminogen activators?
Liver, plasma, endothelium
What is a common source of heparin?
Mast cells (basophils also contain heparin)
What is warfarin and how does it work?
It is an anti-oral coagulant which decreases prothrombin and procoagulation facctors - inhibits production of VitK dependent factors
How does aspirin work? How long does it work for?
-It irreversibly inhibits cyclooxygenase which is necessary to produce downstream aggregation factors such as TXA2 - lasts about a week
How are the platelets activated?
Once they are bound to the vWF, actin protein activates them by causing a conformational change. This exposes their surface receptors and number of factors are released such as ADP, TXA2, vWF.
How would you test a patients intrinsic and common pathway and what is the normal range for this test?
Through aPPT (activated partial thromboplastin time), 30-45 seconds
How would you test a patients extrinsic pathway and what would the normal time range of this test be?
Prothrombin time (PT) - Time taken by plasma to clot after tissue factor and calcium are added - Normally this is 10 - 14 seconds
Which pathways would clotting time measure and what the normal time range for clotting?
All pathways, 3-10 minutes.
How would you test primary haemostasis in a patient and what is the normal time range for this test?
- Tests the primary phase of haemostasis (vasoconstriction and platelet plug) - Normally occurs between 3 - 6 minutes
How would you assess a patients secondary haemostasis and what is the normal time range for this test?
Clotting time, 3-10 minutes


