Week 2-Neck anatomy 2 Flashcards
What are some causes of lumps in the neck?
- Cervical (branchial) cyst (embryological)
- Thyroglossal duct (embryological)
- Thyroid gland (elnargement or tumour)
- Lymphadenopathy (tumour or infection)
- Salivary gland (tumour or infection)
- Epidermoid cysts
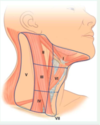
What can lymph nodes be grouped into?
Lymph nodes can be grouped into levels I-VI
This guides prognosis and tx in head and neck cancer –> determine lymph node spread of primary head and neck tumours
Number of levels of nodes determined and size of lymph nodes, best mode of tx can be instituted (surgery/ radiotherapy/ chemotherapy). Node level enables prognosis to be made.

What are the levels lymph nodes can be grouped into?
- Level 1 –> from midline submental triangle to level of submandibular gland
- Level 2 –> from skull base to level of hyoid bone anteriorly, and posteriorly to the level of the sternocleidomastoid.
- Level 3 –> inferior to hyoid bone, up to cricooid arch, posterior follows the sternocleidomastoid
- level 4 –> inferior to cricoid to top of manubrium of sternum, anterior to posterior border of sternocleidomastoid
- Level 5 –> posterior to sternocleidomastoid from skull base to clavicle, anterior to trapezius
- Level 6–> below hyoid and above jugular notch of sternum in the midline
- Level 7 –> below level of jugular notch
What do many of the head/ neck structures develop from?
Many develop from series of loops of tissue called the pharyngeal arches.
What is a pharyngeal arch?
Pharyngeal arches = Interconnecting loops of ectoderm, mesoderm and endoderm (lower face and neck)
Outside covered in ectoderm, inside covered in endoderm and inbetween those layers packed with mesoderm –> core of mesenchyme

Where does the mesoderm within a pharyngeal arch come from?
What type of cells are required within a pharyngeal arch?
Mesoderm has to migrate into the pharyngeal arch, if this doesnt occur –> pharyngeal arch defect.
Cranial neural crest-derived mesenchymal cells (ectomesenchyme) migrate into pharyngeal arches, from midbrain and hindbrain region forming:
neurons
Schwann cells
smooth muscle cells
osteoblasts
chondrocytes

how many pharyngeal arches are there in humans?
There are 6, however arch 5 is only transient, in the adult you’re left with only 5 arches: 1, 2,3,4,6
What is a pharyngeal pouch?
What is a pharyngeal cleft/ groove?
Pharyngeal pouch = internal indentation within a pharyngeal arch. Tissue that develops into specific organs may sit here.
Pharyngeal cleft/ groove = external indentation separating the pharyngeal arches

Why are there only 4 pharyngeal arches shown?

Only 4 Pharyngeal arches shown as only arches 1,2,3,4 and 6 develop.
Arch 5 disapppears, arch 6 is small and will appear tucked under arch 4.
What does each arch have?
- Each arch has an aortic arch arterial vessel supplying it (from the heart tube in red within thorax region)
- Mesoderm develops –> muscle, cartilage, cartilage can form bone
- Each is innervated by a cranial nerve

Which cranial nerve supplies pharyngeal arch 1?
Which muscles develop from arch 1?
What bones/ ligaments develop from arch 1?
1st arch –> cranial nerve V supplies it
Muscles of mastication, mylohyoid, anterior belly of digastric, tensor tympani, tensor veli palatini
Bones/ ligaments: Malleus, incus, spine of sphenoid, sphenomandibular ligament, maxilla, zygona and mandible
What signs and sx might be associated with a pharyngeal arch 1 defect?
What cells have failed to migrate?
Small mandible, zygoma and maxilla may not develop properly, leading to eyes being in incorrect position.
Plus conductive deafness –> incus and malleus do not develop properly
Defects in the development of pharyngeal cleft 1 can result in preauricular (i.e. in front of the pinna of the ear) cysts and/or fistulas.
Neural crest cells have failed to migrate.
What aortic arch is associated with arch 2?
What innervates arch 2?
What are the derivatives of arch 2?
- Associated with 2nd aortic arch, develops into stapedial artery
- Innervated by facial nerve CN VII
- Derivatives: Muscle
- muscles of facial expression
- posterior belly of digastric
- stylohyoid muscle
- stapedius
- Derivatives: Bone/ cartilage:
- lesser horn of hyoid
- upper half of body of hyoid
- stapes
- styloid process
What innervates pharyngeal arch 3?
Which aortic arch is it associated with?
- Innervated by CNIX (Glossopharyngeal)
- Associated with aortic arch 3 –> contributes to common carotid and proximal part of internal carotid artery
- Derivatives: Muscle
- stylopharyngeus
- Derivatives: Bone/ cartilage
- greater horn of hyoid
- lower half of body of hyoid
What aortic arch is assocaited with pharyngeal arch 4?
What CN innervates it?
What are the derivatives of arch 4?
- Associated with aortic arch 4 –> contributes to proximal right subclavian and arch of aorta
- innervated by CNX
- derivatives: muscular:
- muscles of soft palate (except tensor veli palatini)
- muscles of pharynx (except stylopharyngeus)
- cricothyroid
- cricopharyngeus
- Derivatives: bone/ cartilage:
- thyroid cartilage
- cricoid cartilage
- arytenoid cartilage
- corniculate cartilage
- cuneiform cartilage
- Note 4th and 6 th arches contribute to laryngeal cartilage
Arch 6 is associated with aortic arch?
Innervated by which cranial nerve?
Derivatives are?
Arch 6 associated with aoritc arch 6, conturbutes to priximal pulmonary artery and ductus arteriosus
innervated by CNX
derivatives: muscular:
intrinsic laryngeal muscles (except cricothyroid)
skeletal muscle of oeosphagus
Derivatives: Bone/ Cartilage:
Thryoid/ cricoid/ arytenoid cartilage/ corniculate/ cuneiform cartilages (plus 4th contributes)
What are pharyngeal pouches?
What do pouches 1-4 develop into?
Pharyngeal pouches are the internal indentations between the arches.
Pouch 1 – >develops into tubotympanic recess (middle ear and pharyngotympanic tube)
Pouch 2 – >develops into palatine tonsil (epithelium lining pouch 2 forms crypt of tonsillar mass)
Pouch 3 – > Inferior parathyroid gland and part of the thymus
Pouch 4 –> superior parathyroid gland (doesnt migrate much inferior migrates lower than it), plus parafollicular C cells (migrate to within the thyroid gland).

What happens to many of the pharyngeal pouch derivatives?
Many of the pharyngeal pouch derivatives migrate inferiorly to reach their final position:
Inferior parathyroid gland migrates down to thryoid
Superior parathryoid gland doesnt migrate much
Parafollicular C cells migrate into the thyroid gland
Thymus has to migrate down into to mediastinum (remember within superior mediastinum in children, eventually migrates to anterior mediastinum in adults).

Why is knowledge of migration patterns of pharyngeal pouch derivatives important clinically?
Useful in the case of abnormal migration and surgical removal, derivatives may not be where you think they will be.
What does the pharyngeal cleft and pouch 1 develop into?
Region formed by pharyngeal cleft and pouch 1 develops into the external and middle ear, and tympanic membrane.
1st cleft develops into your external auditory meatus
1st pouch will develop into the tympanic cavity (houses malleus/ incus/ stapes) and mastoid antrum, pharyngotympanic tube (which connects to the nasopharynx).
Tympanic membrane = Thin tissue between cleft 1 and pouch 1 is formed of ectoderm, endoderm and mesoderm = tympanic membrane

What may a remnant of the 1st pharyngeal cleft be observed as?
Remnants of the 1st pharyngeal cleft may be observed externally as auricular (preauricular) sinuses/ cysts
Right pic = preauricular sinus (first cleft did not fully disappear)
Left pic = auricular/ preauricular cyst

Why do we not have ridged neck / gill remnants?
Due to growth of 2nd arch tissue growing downwards to cover over pharyngeal clefts 2-4
as it does so it seals off the cervical sinus, normally an open space that should disappear.

What does the platysma muscles form within?
What innervates platysma?
Platysma forms within the downgrowth of pharyngeal arch 2 and is innervated by CN VII

What can occur if pharyngeal arch 2 fails to grown over the lower arches/ cover the cervical sinus?
Cervical (branchial) cysts, sinuses or fistulas are formed from remnants of the embryological cervical sinus.
Most of sinus can be obliterated, but some can remain and be quiescent. Then suddenly grow over a period of a few weeks, self contained sac full of cellular debris/ fluid = cervical cyst.
Cervical cysts can appear slowly, but many appear quickly.
Often form on the border of anterior border of sternocleidomastoid in the anterior triangle.



























