Vision loss - occlusions (all occlusions sudden vision loss) Flashcards
What are the causes of sudden vision loss (hint split the causes into painful and painless causes)
Note
- Closed angle glaucoma
- Optic neuritis
- Stroke
Are discussed in other flashcards

What are some of the types of occulsion of the blood supply that can result in sudden vision loss ?
CRAO, CRVO, or occulsion of the branches
What are some of the causes of haemorrhage which results in sudden vision loss?
- Due to abnormal blood vessels (e.g. diabetes, wet ARMD)
- Retinal tears
What are the symptoms/signs of a CRAO (central retinal artery occlusion) ?
Symptoms:
- Sudden vision loss - within seconds
- Painless
Signs:
- Afferent pupillary defect
- Retina appears white
- Cherry red spot at the macula
- Thread like retinal vessels
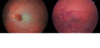
What could potentially have caused the appearance of this retina ?

CRAO
What are the underlying causes of CRAO’s?
- GCA (always rule this out)
- Embolic - Calcific heart valves, Vegetations, Thrombus
- Carotid Artery disease
What is the acute management of CRAO’s if presenting within 24hrs of onset of symptoms?
- Occular massage,
- Paper bag breathing
- IV Diamox (acetazolemide)
to try convert it from a CRAO to a BRAO
What is the more chronic management of CRAO ?
- Carotid doppler to find the source of emboli
- Antihypertensive treatment
- Hyperbaric oxygen
- Surgical removal of aqueous from anterior chamber
Note that CRAO is a form of stroke
There are 2 further types of arterial occlusions relating to the eye what are they ?
BRAO and Amaurosis fugax
What are the symptoms/signs of amaurosis fugax ?
Symptoms:
- Transient painless visual loss - no more than 5 mins
- Like a curtain coming down
- 90% of time visual acutiy is worse
Signs:
- Usually nothing to be seen
What does amuarosis fugax require ?
Immediate referal to TIA clinic
How can CRAO’s be defined as ?
- They are ischaemic attacks
- Therefore amaurosis fugax can be defined as a transient ischaemic attack (TIA)
What are the causes of CRVO’s?
- Atherosclerosis
- Hypertension
- Hyperviscosity
- Raised IOP - due to gluacomas
What are the signs/symptoms of CRVO’s?
Symptoms:
- Sudden vision loss - precieved by the patient as sudden but is less sudden that CRAO
- Reduced visual acuity
Signs:
- Retinal haemorrhages
- Dilated tortuous veins (have a lot of bends)
- Disc swelling and macular swelling
- Cotton wool spots
What could the appearance of the fundoscope shown be due to ?

CRVO
What investigation is done to diagnose CRVO?
Fluorescence angiogram
What is the treatment of CRVO’s?
- If no signs of ischaemia - observe (every 3 months initially then less frequently)
- If ischaemic but no neovascularition - observe closely (every 4-6 weeks )
- If ischaemic with neovascularisation – requires urgent argon laser pan-retinal photocoagulation
Compare the fundoscope appearance of CRVO and CRAO
What is ischaemic optic neuropathy ?
Where the posterior ciliary arteries (PCA) become occluded due to inflammation or atheroma, resulting in infarction of the optic nerve head

What are the 2 types of ischaemic optic neuropathy ?
- Arteritic 50% - inflammation (GCA)
- Non-arteritic 50% - atherosclerosis
What are the visual symptoms/signs of ischaemic optic neuropathy ?
Symptoms:
- Sudden profound vision loss
- Irreversible blindness
Signs:
- Pale, swollen disc

Describe the pathogenesis of arteric ischaemic optic neuropathy
- GCA caused inflammation of medium to large sized arteries
- This results in occlusion of the arteries
- Posterior cilliary arteries become occluded and therefore ischamia of the optic head
What are the key symptoms (not visual ones) that suggest arteric ischaemic optic neuropathy ? (think GCA)
- Headache
- Jaw claudication
- Scalp tenderness
- Tender enlarged scalp arteries
- Very High ESR , PV and CRP
What is the risk in a patient who has gone blind in one eye due to arteric ischaemic optic neuropathy ?
That they will go blind in the other eye


