The Respiratory System Flashcards
RESPIRATORY TRACT

Upper
- Humidify & warm air
- Defence – mucus and cilia
- Sensory
- Speech
Lower
- GAS EXCHANGE
- Defence
- Metabolic
WHAT IS THE FUNCTION OF THE LARYNX?
To generate different sounds
WHAT PARTS OF THE LUNGS ARE KNOWN AS THE ‘CONDUCTING ZONES’?
The tubes (e.g. trachea and primary bronchus)
LOWER RESPIRATORY TRACT

WHAT IS THE PARENCHYMA?
The part of the lungs where gas exchange occurs
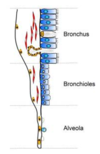
LUNG BRANCHES

AIRWAY RESISTANCE
- Proportional to 1/radius4
- But conduction summative
–huge numbers of respiratory bronchioles
–small airways make a small contribution to total Resistance
•Conducting zone bronchioles largest influence
Inversely proportional to conductance; higher the resistance, the less efficient conduction.
AIRWAY RESISTANCE IS INCREASED IN MANY DISEASES
- Smooth muscle contraction
- Obstruction with mucus
- Collapse
- Structural changes occur in the conducting airways
- Smooth muscle growth
- Fibrosis

LUNG EPITHELIUM
- Lining cells in airway
- Specialisation changes down the airway
–Bronchi
•ciliated, goblet, glandular
–Bronchioles
•ciliated, non-ciliated, goblet, club cells
–Alveoli
•Squamous, cuboidal
Ciliated= waft
Goblet cells secrete mucus (as do glandular cells)
Club cells (secretory cells)
Highly specialised cells in the alveoli (specialised for gas exchange).
AIRWAY STRUCTURE

AIRWAY INNERVATION
Sensory (afferent) nerves FROM the airway epithelium and smooth muscles signal to the brain.
Autonomic fibres TO glandular epithelium and smooth muscle from CNS
- Parasympathetic branches of the vagus nerve (vagus nerve is the main nerve supplying the lungs).
- Excitatory (e) and inhibitory (i)
- Very little sympathetic innervation (most nerves are parasympathetic).
- ß-adrenoceptors on airway smooth muscle are stimulated by circulating adrenaline.

THE RESPIRATORY UNIT
•Massive network of airways and air sacs (around 500 million) to maximise surface area (50-100 m2).
Pneumocytes are very thin, flat cells to allow maximum _ exchange.
Also surrounded by dense _ network= gas exchange.

Capillary
Gas
ALVEOLAR EPITHELIUM CELLS (PNEUMOCYTES)
•Type I (Gas exchange cells)
–Very large surface area
- cover 95% of alveolus
- 10% of cells
–squamous
–gas exchange
•Type II cells (secrete surfactant, they also replace TI cells when the TI cells die)
–cuboidal
•majority of cells
–secretory
•surfactant
–precursors for type I
WHAT DO TYPE II CELLS SECRETE?
Surfactant
SURFACTANT
•Produced by type II alveolar epithelial cells
–Lipid (90%) – mostly phospholipid
–Proteins – SP-A, -B, -C, -D
•Reduces surface tension
–prevents alveolar collapse (atelectasis)
- Innate immunity function
- Instilled into babies with Infant Respiratory Distress Syndrome
–Beractant (bovine)
–Pumactant (synthetic, lipid only)
LUNGS AT BIRTH
- Lung epithelium develops in last trimester of pregnancy.
- Maturation stimulated by _ in premature babies
- Lung is fluid filled in foetus - must rapidly empty
–Surge in corticosteroids and catecholamines at birth
–Activation of absorptive channels
•Epithelial Sodium Channels (ENaC)
–Pressure changes (squeeze through birth canal)
•Caesarian section – reduced drive for fluid absorption
Corticosteroids
BLOOD SUPPLY TO THE LUNGS
•Pulmonary circulation
–Artery flows directly from the right ventricle
- LOW oxygen
- HIGH flow
- _ pressure
–Capillaries pass around the alveoli
–Pulmonary _ returns oxygenated blood to left heart
•Bronchial circulation
–From aorta (left ventricle)
–HIGH pressure
–Supplies oxygen and nutrients the conducting airways
–Not involved systemic respiration processes
–Only 2% of cardiac outflow

Low
Vein
VENTILATION IS AUTOMATIC AND CONTROLLED BY THE CNS.
TRUE OR FALSE?
TRUE
NEURONAL CONTROL OF BREATHING

MUSCLE INNERVATION
Somatic motor nerves
Innervate skeletal muscles in the thorax
- Phrenic
- innervates the diaphragm
- irritation => hiccough
- Intercostal
Autonomic nerves
Bronchial
•supply smooth muscle & secretory cells
–branch from vagus
–reflex bronchospasm and mucus secretion
–important in asthma
Sensory output
RESPIRATORY MUSCLES
Intercostals are between the _.
External intercostals contract to lift ribs _.
Internal intercostals contract to pull ribs down again and to force air out.
Ribs
Upwards
SENSORY AFFERENT PATHWAYS FROM THE LUNG (MYELINATED)
•Send impulses via vagus to medullary centres
Slowly adapting
–Stimulated by stretch receptors in airway smooth muscle
–Elicit reflexes
- Shortened inspiration
- Hering-Breuer reflex
–Promotion of expiration following steady inflation
–Prevents over-inflation of lung
Rapidly adapting stretch receptors
–Stimulated by sudden, sustained inflation
–Also by ‘irritant receptors’ among epithelium
–Elicit reflexes:
- Cough
- Bronchoconstriction
- Mucus secretion
WHAT STIMULATES RAPIDLY ADAPTING STRETCH RECEPTORS?
Sudden, sustained inflation of the lungs





















