The Liver Flashcards
THE HEALTHY LIVER
oSynthesis and secretion of _.
oMetabolism
oPlasma proteins– major source of plasma proteins including albumin and _ factors (see blood lectures)
oEndocrine function
oExcretory and degradative functions
oIron storage
Bile
Clotting
SUMMARY OF LIVER FUNCTIONS
Exocrine (digestive) Functions- synthesis and the secretion of bile for the adequate digestion and absorption of _.
Secretes _ into a bicarbonate rich solution that helps to neutralize acid in the duodenum
Endocrine functions– e.g. Secretes insulin-like growth factor 1 (IGF-1) in response to growth hormone. This promotes cell division in a number of tissues including bones.
Clotting factors- Produces many of the plasma clotting factors including prothrombin an fibrinogen.
Bile salts – essential for the absorption of fat soluble vitamin K that is required for the formation of _ factors in the liver.
Plasma proteins- Synthesizes and secretes proteins including plasma _, acute phase proteins, binding proteins for a variety of hormones and lipoproteins
Metabolism-
- Coverts plasma glucose to _ and triglycerides
- Converts plasma amino acids to fatty acids
- Synthesizes triglycerides and secretes them as lipoproteins
- Produces glucose from glycogen (_)
- Converts fatty acids to _ during fasting
- Produces urea – major end product of amino acid (protein) catabolism and releases into the blood
Cholesterol metabolism-
- Synthesizes cholesterol and releases into the blood
- Secretes cholesterol into bile
- Covers plasma cholesterol into bile salts
Iron and vitamin B12 storage
Fats
Bile
Clotting
Albumin
Glycogen
Glyconeogenesis
Ketones
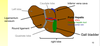
ANATOMY

WHAT IS THE LIVER COMPOSED OF?
Four incompletely separated lobes that are supported by two ligaments
GROSS LIVER ANATOMY
oApprox 1.5 kg (2 % body weight in adults)
oAnatomically four lobes: left, right, caudate and quadrate
oFunctionally considered as two lobes - left and right
oDiaphragmatic surface is the superior upper surface of the liver
oVisceral surface faces adjacent abdominal organs (faces downwards); the porta hepatis and gallbladder are located on this surface.
WHAT ARE THE FOUR LOBES OF THE LIVER CALLED?
Left
Right
Caudate
Quadrate
ANATOMY 2
- Caudate (cauda = tail)
- Quadrate (quadratus = squre)
The Caudate lobe is next to the _ vena cava
The Quadrate lobe is next to the _ bladder

Inferior
Gall
WHERE IS THE CAUDATE LOBE OF THE LIVER?
Next to the inferior vena cava
WHERE IS THE QUADRATE LOBE OF THE LIVER?
Next to the gall bladder
LIVER STRUCTURE
oFalciform ligament: separates the major right and left lobes and attaches the liver to the _ and anterior abdominal wall
oRound Ligament: Found at the lower edge of the falciform ligament.
oGall bladder – accessory organ – pear shaped sac 7-10 cm long
-Rests in a recess on the inferior, visceral surface of the liver
FACIFORM LIGAMENT – secures the liver to the anterior abdominal wall
Round ligament – remnant of the _ _.
Diaphragm
Umbilical cord
LIVER LOBES FROM VISCERAL SURFACE
HEPATIC BLOOD CIRCULATION
oThe liver receives blood from two sources; the _ and GI tract.
oHepatic portal vein delivers poorly _ blood from the GI tract.
oHepatic artery delivers oxygenated blood from the heart.
oHepatic portal vein and artery divide into two to supply the left and right side of the liver
Heart
Oxygenated
WHAT TWO SOURCES DOES THE LIVER RECEIVE BLOOD FROM?
Heart
GI Tract
HEART STRUCTURE

HEPATIC CIRCULATION
- The hepatic portal vein carries blood form the GI tract, _ and pancreas,
- Rich in nutrients but poor in _.
- Hepatic artery – branches from _ and eventually splits into right and left hepatic arteries
- Hepatic vein –at the centre of each lobule is the central vein that drains into the hepatic vein
oAorta supplies oxygenated blood via the hepatic artery
oBlood supplied to the liver via the hepatic portal vein and hepatic artery
oHepatic portal vein drains blood from the capillary beds of the GI tract including spleen and pancreas.
oHepatic vein carries blood away from the liver back to the _.
Spleen
Oxygen
Aorta
Heart
WHERE DOES THE HEPATIC PORTAL VEIN CARRY BLOOD FROM?
Carries blood from the spleen, GI tract and pancreas
HOW IS BLOOD SUPPLIED TO THE LIVER?
Via the hepatic portal vein and hepatic artery
WHAT DOES THE HEPATIC VEIN DO?
Carries blood away from the liver back to the heart
LIVER HISTOLOGY
o50,000 – 100,000 functional units called _. Hepatic lobules have a small polyhedral shape; these are the functional units of the liver.
oWithin each lobule are cells called _.
oAt the edge of each lobule are portal triads – these are formed by the hepatic portal vein, the hepatic artery and the bile duct
oCentral Vein empties into the hepatic veins and then the vena cava.
Lobules
Hepatocytes
WHAT ARE PORTAL TRIADS FORMED BY?
Formed by the hepatic portal vein, the hepatic artery and the bile duct
WHAT ARE THE CELLS INSIDE LIVER LOBULES CALLED?
Hepatocytes
CLASSIC LIVER LOBULES
Blood flows from the portal triad (contains the portal vein and hepatic artery) towards the central _.
Bile flows in the opposite direction towards the portal triad (contains the bile _)
Vein
Duct
LIVER LOBULE STRUCTURE

The numerous projections of the wheel spokes are the hepatic sinusoids – thin walled leaky _ where venous and arterial blood mix as they slowly flow through the hepatic lobe towards the central vein.
Hepatocytes absorb nutrients from blood and produce bile that collects in the small bile caniculus.
Capillaries
WHAT ARE HEPATIC SINUSOIDS?
Thin walled leaky capillaries where venous and arterial blood mix as they slowly flow through the hepatic lobe towards the central vein.











