SM 122a - Physiology of Erythropoiesis Flashcards
An anemic patient with low MCV and low MCHC has what kind of anemia?
Microcytic, hypochromic anemia
What is a “left shift” in the hemoglobin oxygen-dissociation curve?
Anything that increases hemoglobin’s affinity for oxygen causes a left shift in the oxygen dissociation curve
- Decreased temperature
- Increased pH
- Decreased CO2
- Decreased 2,3-Bisphosphoglycerate (BPG)

How is the RBC compartment volume (Vc) measured via isotopic dilution?
- RBCs are labeled with 57Chromium
- A fixed volume of labeled RBCs are injected
- A blood sample is taken at suitable times
- The percentage of radioactive RBCs in the sample is used to calculate the total RBC compartment volume

What is the gold standard measurement for whole blood components?
What is used in clinical practice?
Gold standard = isotopic dilution
Clinical practice = Measure Hemoglobin concentration, RBC count, and Hematocrit in a sample of peripheral blood
What does mean corpuscular hemoglobin concentration (MCHC) measure?
How is it calculated?
The average concentration of hemoglobin in red blood cells
MCHC = 100 * Hgb/Hct (in pg/100uM^3)
What factors impact the marrow erythroid response?
- Severity of anemia
- Hypoxia
- Presence of normal pool of stem cells
- Supply of essential nutrients
- Abnormal structure of marrow
- Ex: radiation damage, myelofibrosis
A patient has abnormal non-alpha globulin chains due to genetic mutation.
Which chromosome contains the mutation?
Chromosome 11
Describe the structure of hemoglobin
Hemoglobin is a tetramer
Each monomer = Heme + globin
How do RBCs derive their energy?
Glucose metabolism
- Emden-Meyerhoff
- Hexose monophosphate shunt
What hormone stimulates the production of red blood cells?
Erythropoietin
What is the marrow erythroid response?
Stem cells in the bone marrow respond to EPO and enter the erythrogenic pathway to proliferate and mature
What does mean corpuscular volume (MCV) measure?
How is it calculated?
The average size of red blood cells
MCV = 10 * Hct/RBC (in uM^3 per cell)
Which hemoglobin is found in the RBCs of a fetus?
Fetal Hemoglobin

What energy metabolites are important for RBC function?
Where do they come from?
- NADH to maintain Fe2+ supply
- ATP for ion transport
- Via glycolytic pathway
- NADPH to maintain membrane protein SH groups
- Via hexose-monophosphate shunt
In which cells does hemoglobin synthesis occur?
Where in these cells?
Erythroblasts in the bone marrow primarily
- Heme is synthesized in the mitochondria
- Globin is synthesized in the cytoplasm by ribosomes
- Final assembly occurs in the cytoplasm
(And to a lesser degree in reticulocytes)
How would Vp respond to a large, abrupt hemorrhage…
- Immediately?
- After 3 days?
- After 1 month?
Vp (Plasma compartment volume) would immediately decrease. Blood volume regulation would work to increase Vp above normal in order to restore Vb. This would decrease Hct, and have no effect on Vc

Where is Erythropoietin (EPO) produced?
Renal interstitial cells
What are the major components of the erythron system?
- Bone marrow
- Stem cells through reticulocytes (stages of maturation)
- Blood
- Mature RBCs
- Aged RBCs
- Plasma
- Amino acid pool
- Fe pool
- Bilirubin pool
- Macrophages
- Degradation of RBCs
- Liver
- Processing of Bilirubin (waste products)
What is the normal concentration of bilirubin in the circulation?
0.5-1.0 mg/dL
List the stages of erythropoiesis
Stop Promoting Basic Polygamist Or Relative Marriages
- Stem cell
- Pronormoblast
- Basophilic normoblast
- Polychromatophilic normoblast
- Orthochromatic normoblast
- Reticulocyte
- Mature RBCs
(Reticulocytes and mature RBCs are not nucleated)
If a patient is hypochromic, what do you know about their RBC properties?
Low MCHC
What are the 2 major factors that determine O2 delivery to tissues?
- The number of RBCs perfusing the tissues
- The O2 carrying capacity of hemoglobin
What drives regulation of erythropoiesis?
Changes in levels of oxygenated hemoglobin, as monitored by the kidney.
The kidney stimulates or suppresses the formation of new RBCs; it does not mediate changes in rate of degradation
If a patient is normocytic, what do you know about their RBC properties?
Normal MCV
How long do RBCs live in the circulation?
118-120 days
How does 2,3 Bisphosphoglycerate (2,3 BPG) affect red blood cells?
2,3 BPG stabilizes the tense (not bound to oxygen) state of hemoglobin in red blood cells, thus lowering hemoglobin’s affinity for oxygen
It has a higher affinity for deoxyhemoglobin than for oxyhemoglobin
What does high erythropoietin (EPO) indicate?
Anemia or hypoxia
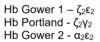
Which hemoglobin is found in the RBCs of an embryo?
How do inflammatory cytokines like IL-1, IL-6, TNF-alpha, and TFG-beta affect serum EPO levels?
Inflammatory cytokines cause a decrease in erythroid marrow mass, leading to increased serum EPO
What does mean corpuscular hemoglobin (MCH) measure
How is it calculated?
The average quantitiy of hemoglobin in a single red blood cell
MCH = 10 * Hgb/RBC (in pg per cell)
What factors increase hemoglobin’s affinity for oxygen?
When the hemoglobin is not in an oxygen-starved environment, it holds onto the O2 (ex: near the lungs)
- Decreased temperature
- Increased pH
- Decreased CO2
- Decreased 2,3-Bisphosphoglycerate (BPG)
What is the effect of an increase in the circulating concentration of oxygenated hemoglobin?
The kidneys sense an increase in the [oxygenated hemoglobin]. This causes the kidneys to suppress the release of erythropoietin, leading to repression of proliferation of new red blood cells
Note: rate RBC degradation is not affected
How would Vb respond to a large, abrupt hemorrhage…
- Immediately?
- After 3 days?
- After 1 month?
Vb (total blood volume) would immediately decrease. It would be restored within 3 days due to rapid increase of Vp.

How is a reticulocyte histologically different from a mature RBC?
A reticulocyte is larger and blue-er compared to the mature RBC.
It is anucleate (like the mature RBC), but still contains some residual RNA
If a patient is normochromic, what do you know about their RBC properties?
Normal MCHC
An anemic patient with normal MCV and normal MCHC has what kind of anemia?
Normocytic, normochromic anemia
What is the clinical presentation of hyperbilirubinemia?
Yellow skin (jaundice) and yellow sclera (icterus)
What percentage of each RBC does hemoglobin make up?
33%
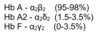
Which hemoglobin is found in the RBCs of an adult?
An anemic patient with high MCV and normal MCHC has what kind of anemia
Macrocytic, normochromic anemia
What happens to hemoglobin upon RBC degradation?
- Globin -> reusable amino acids
- Heme -> Fe3+ is recycled
- The heme ring is oxidized to linear biliverdin, which is reduced to bilirubin.
- This is exported to the plasma, transported to the liver, and excreted
- The heme ring is oxidized to linear biliverdin, which is reduced to bilirubin.
What factors decrease hemoglobin’s affinity for oxygen?
When the hemoglobin is in an oxygen-starved environment, it releases its O2 to the tissues that need it (ex: exercising muscle)
- Increased temperature
- Decreased pH
- Increased CO2
- Increased 2,3-Bisphosphoglycerate (BPG)
How long does RBC production take?
~ 2 weeks from stem cell to mature RBC
At any given time, there are some RBCs undergoing maturation. This is why Vc may begin to recover ~5-6 days after severe hemorrhage
A patient has abnormal alpha-globulin chains due to genetic mutation.
Which chromosome contains the mutation?
Chromosome 16
What is a “right shift” in the hemoglobin oxygen-dissociation curve?
Anything that decreases hemoglobin’s affinity for oxygen causes a rightshift in the oxygen dissociation curve
- Increased temperature
- Decreased pH
- Increased CO2
- Increased 2,3-BPG

Would exercise cause a left shift or a right shift in the hemoglobin oxygen-dissociation curve?
Why?
Exercising muscles would cause a right shift in the hemoglobin oxygen-dissociation curve.
Exercising muscles are warmer, more acidic, and contain more CO2 than non-exercising muscles.
All of these factors decrease hemoglobin’s affinity for oxygen, so it can be delivered to the exercising muscles efficiently
Which body system senses changes in the circulating concentration of oxygenated hemoglobin?
What is the effect of an increase?
A decrease?
The kidney senses changes in the concentration of oxygenated hemoglobin that circulates in the blood.
A decrease in the [oxygenated hemoglobin] causes release of erythropoietin, which stimulates the proliferation of new red blood cells
An increase in the [oxygenated hemoglobin] causes suppression of erythropoietin release, which represses the proliferation of new red blood cells
What degrades RBCs?
Macrophages
If a patient is anemic, what would you expect their EPO levels to look like?
You would expect them to be high.
Anemia indicates that RBCs are being destroyed, so you would expect the body to compensate by generating signals to make more RBCs
Describe the degradation/processing of bilirubin
Bilirubin is a waste product of RBC degradation.
- In the macrophage, the heme of hemoglobin is…
- Oxidized to linear biliverdin
- Biliverdin is reduced to bilirubin
- Bilirubin is exported to the cytoplasm
- In the cytoplasm
- Bilirubin is bound to an albumin complex and delivered to the liver
- In the liver
- Bilirubin is conjugated with glucuronic acid to bilirubin diglucuronide
- Bilirubin diglucuronide is secreted into the bile
- Bile travels through the biliary tract to the duodenum
- Intestinal bacteria turn bile into urobilinogen
- Urobilinogen is excreted through the feces
How is plasma volume (Vp) measured via isotopic dilution?
- 131I-albumin is injected into the patient
- A blood sample is taken at suitable times
- The percentage of labeled albumin that is recovered is used to calculate the total plasma volume

What are the clinical implications of hyperbilirubinemia?
Liver disease
OR
Increased RBC destruction
Describe the structure and size of a mature RBC
Biconcave, pliable disk with no nucleus or mitochondria
8 uM x 2 uM
What is the effect of a decrease in the circulating concentration of oxygenated hemoglobin?
The kidneys sense a decrease in the [oxygenated hemoglobin]. This causes the kidneys to release erythropoietin, which stimulates the proliferation of new red blood cells
Note: rate RBC degradation is not affected
How is whole blood volume (Vb) calculated from isotopic dilution?
Vb = Vp + Vc
How would Hct respond to a large, abrupt hemorrhage…
- Immediately?
- After 3 days?
- After 1 month?
Hct (the proportion of RBCs in your blood) would not show any immediate changes. However, it would decrease as Vp increases to restore Vb. It would be lowest 2-3 days after hemorrhage, and recovery by ~1 month

If a patient is macrocytic, what do you know about their RBC properties?
High MCV
Which general pathway does EPO function through?
Binding of EPO to the EPO receptor (EPOR) activates the JAK/STAT pathway, that leads to RBC proliferation
If a patient is microcytic, what do you know about their RBC properties?
Low MCV
How would Vc respond to a large, abrupt hemorrhage…
- Immediately?
- After 3 days?
- After 1 month?
Vc (RBC compartment volume) would immediately decrease due to loss through hemorrhage. It would begin to recover after ~5-6 days due to proliferation of new RBCs

What is the normal percentage of reticulocytes in the circulation?
What do high levels indicate?
Low levels?
Normal = 0.5-1.5%
-
Too high => rapid erythropoiesis
- Normal response to anemia or 4-5 days after hemorrhage
- May indicate cancer if there is no physiological basis for increased RBC synthesis
- Too low => insufficient erythropoiesis
What is the erythron?
Mature RBCs and progenitors of RBCs


