S4) The Autonomic Nervous System Flashcards
(35 cards)
What does the autonomic nervous system do?
Regulates physiological functions
- Heart rate
- BP
- Body temperature
- coordinates bodys response to exercise and stress
Describe two general ways in which the ANS can regulate physiological functions
- Sympathetic activity is increased under stress
- Parasympathetic activity is increased under basal conditions
What does the ANS exert control over?
- Smooth muscle
- Exocrine secretion
- Inotropy (increased contraction) & chronotropy (increased heart rate) in heart
Describe the neurotransmitters and receptors acting on the heart in the parasympathetic nervous system and sympathetic nervous system respectively
- PNS action on heart rate is mediated via acetylcholine acting on M2 muscarinic receptors
- SNS action on heart rate and contractility is mediated via noradrenaline acting on β1 adrenoreceptors
Outline the ANS control of the cardiovascular system
The ANS controls:
- Heart rate
- Force of contraction of heart
- Peripheral resistance of blood vessels
- Amount of venoconstriction
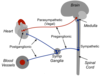
In 4 steps, describe the parasympathetic input to the heart
⇒ Preganglionic fibres via vagus nerve
⇒ Synapse with postganglionic cells on epicardial surface / within heart wall of at SAN/AVN
⇒ Postganglionic cells release ACh
⇒ ACh acts on M2 receptors ( G coupled protein receptors)
What is the effect of the PNS on the heart?
- Decrease heart rate (negative chronotropic effect)
- Decrease AVN conduction velocity
In 4 steps, describe the sympathetic input to the heart
⇒ Postganglionic fibres from the sympathetic trunk
⇒ Innervate SAN, AVN and myocardium
⇒ NA is released
⇒ NA mainly on β1 adrenoreceptors

What is the effect of the SNS on the heart?
- Increases heart rate (positive chronotropic effect)
- Increases force of contraction (positive inotropic effect)
Outline the opposing sympathetic and parasympathetic effects on pacemaker potentials
- Sympathetic activity:
I. Mediated by β1 receptors
II. GPCRs increase cAMP which speeds up the pacemaker potential
- Parasympathetic activity:
I. Mediated by M2 receptors
II. GPCRs increase K+ conductance and decrease cAMP

In 4 steps, explain how noradrenaline increases the force of contraction
NA acts on β1 receptors in myocardium:
⇒ Increased cAMP activates PKA (protein kinase)
⇒ Phosphorylation of Ca2+ channels increases Ca2+ entry
⇒ Increased uptake of Ca2+ in SR
⇒ Increased sensitivity of contractile machinery to Ca2+
=> more contraction
What type of receptors are found in the systemic vasculature?
- Most blood vessels have α1-adrenoreceptors
- Some blood vessels have β2-adrenoreceptors e.g. myocardium, liver, skeletal muscle vasculature
Describe the effects of increased/decreased sympathetic output to the peripheral vasculature

Describe the effect of circulating adrenaline on blood vessels which have both β2 adrenoceptors and α1 adrenoreceptors
Circulating adrenaline has a higher affinity for β2 adrenoceptors than for α1 receptors:
- At [physiological], it will preferentially bind to β2 adrenoceptors
- At [higher], it will also activate α1 adrenoreceptors

Describe the opposing effects of β2 and α1 adrenoreceptors on vascular smooth muscle
- Activating β2 adrenoreceptors causes vasodilation:
I. Increases cAMP → Opens K+ channels & inhibits MLCK
II. Relaxation of smooth muscle
- Activating α1 adrenoreceptors causes vasoconstriction:
I. Stimulates IP3 production → increase [Ca2+]i
II. Contraction of smooth muscle
Describe the cardiovascular control system established by the ANS in terms of afferent and efferent nerves
- Changes are communicated to the brain via afferent nerves:
I. Baroreceptors (high pressure side of system)
II. Atrial receptors (low pressure side of system)
- Alters activity of efferent nerves

What are baroreceptors and what do they do?
- Baroreceptors are nerve endings in the carotid sinus and aortic arch are sensitive to stretch
- Increased arterial pressure stretches these receptors

Briefly, outline the baroreceptor reflex
. - maintains blood pressure over a short time
- re-set to higher levels with persistent increase in blood pressure

What are the three types of drugs which act on the ANS?
- Sympathomimetics
- Adrenoceptor antagonists
- Cholinergics - mimic action of acetyl choline
What are the two types of sympathomimetics?
- α-adrenoceptor agonists
- β-adrenoceptor agonists
Describe the uses of sympathomimetics
- Adrenaline to restore function in cardiac arrest/anaphylactic shock
- β1 agonists given in cardiogenic shock (pump failure)
- β2 agonists used for treatment of asthma
- administer adrenaline to restore function and support
What are the two types of adrenoreceptor antagonists?
- α-adrenoreceptor antagonists (vasodialation)
- β-adrenoreceptor antagonists (bronchoconstirction)
Describe the uses of adrenoreceptor antagonists
- α-adrenoreceptor antagonists – inhibits NA action on vascular smooth muscle α1 receptors, causing vasodilation
- β-adrenoreceptor antagonists – slows HR, reduces force of contraction (β1) and causes bronchoconstriction (β2)
What are the two types of cholinergics?
- Muscarinic agonists
- Muscarinic antagonists







