Quiz 2- Lectures 5-6 Flashcards
cervical spine (lordosis/kyphosis)
lordosis
thoracic spine (lordosis/kyphosis)
kyphosis
lumbar spine (lordosis/kyphosis)
lordosis
sacral spine (lordosis/kyphosis)
kyphosis
lordosis: define
normal inward CONCAVE curvature of the lumbar and cervical regions of the human spin
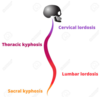
kyphosis: define
normal outward CONVEX curvature in the thoracic and sacral regions; means “bent backward”
fetus: spinal stage
primary curve; large curve

newborn: spinal stage
start seeing concavity in POSTERIOR CERVICAL region and in lumbar region; when patient starts holding up their head, the curves become more pronounced

why doesn’t it take much muscular activity to keep adult body upright?
line of gravity passes through curve of vertebral column

two main segments of the typical vertebrae
arch and body

orientation of facets: cervical
oblique/ horizontal plane

orientation of facets: thoracic
coronal plane

orientation of facets: lumbar
sagittal plane

describe LUMBAR vertebrae
(shape, superior/inferior surfaces, and discs)
- shape: kidney bean vertebral bodies
- superior/inferior surfaces of L1-L3 are parallel**, and L4/L5 are **wedge-shaped
- Discs are wedge-shaped and contribute to most typical lumbar curve (lordosis)

describe venous drainage of vertebrae
*(check)
- basivertebral veins
- anterior & posterior external vertebral venous plexus
- anterior & posterior internal (epidural) vertebral venous plexus
basivertebral veins
- emerge from the foramina on the posterior surfaces of the vertebral bodies.
- communicate through small openings on the front & sides of vertebral bodies with the anterior external vertebral plexuses, and converge behind to the principal canal, and open by valved orifices into the transverse branches which unite the anterior internal vertebral plexuses
ANTERIOR EXTERNAL vertebral venous plexus
- lie in front of the bodies of the vertebrae
- communicate with the basivertebral and intervertebral veins
- receive tributaries from the vertebral bodies
- In cervical region, these anastomose with the vertebral, occipital, and deep cervical veins

POSTERIOR EXTERNAL vertebral venous plexus
- placed partly on the posterior surfaces of the vertebral arches and their processes, and partly between the deep dorsal muscles.
- In cervical region, these anastomose with the vertebral, occipital, and deep cervical veins

ANTERIOR INTERNAL vertebral venous plexus
- consist of large veins on the posterior surfaces of vertebral bodies and IV fibrocartilages on either side of the posterior longitudinal ligament (PLL);
- under cover of PLL they are connected by transverse branches into which the basivertebral veins open
- opens into the vertebral veins and is connected above with the occipital sinus, the basilar plexus, the condyloid emissary vein, and the rete canalis hypoglossi.

POSTERIOR INTERNAL vertebral venous plexus
- one on either side of the middle line in front of the vertebral arches and ligamenta flava
- anastomose by veins passing through those ligaments with the posterior external plexuses.
- opens into the vertebral veins and is connected above with the occipital sinus, the basilar plexus, the condyloid emissary vein, and the rete canalis hypoglossi.

how many processes are there?
what if you include the mammillary processes?
7 processes; but 9 total if you count the mammillary processes
what are the 7 articular processes on the vertebrae?
1 spinous process
2 transverse processes,
4 articular processes (=2 superior/2 inferior)

which processes “arise from junction of pedicles & laminae, except for L5”
transverse process
how do transverse processes change in the lumbar region?
From L1-L3:increasein size fromL1-L3, whereas
L4/L5: decrease in size of transverse processes

where does transverse process arise?
from the vertebral body
where are articular processes located?
at junction of pedicle and lamina

what muscle attaches to the mammillary processes?
multifidous muscle
- (consists of a number of fleshy and tendinous fasciculi, which fill up the groove on either side of the spinous processes of the vertebrae, from the sacrum to the axis.
- Very thin but importnat in stabilizing the joints within the spine.
- One of the transversospinales)
which direction do the following face?
superior articular facets
face medially

which direction do the following face?
inferior articular facets
face laterally

in which plane do the articular facets lie?
sagittal/median plane

how do superior and inferior articular processes differ?
- Spacing: superior articular proc. are further apart (except L5) than inferior articular processes
- Facet Orientation:
- Superior articular facets: face MEDIALLY
- Inferior articular facets: face LATERALLY

How is L5 different than the other lumbar vertebrae?
- largest body
- *wedge-shaped body
- *INF. ARTIC. PROC. are further apart than superior
- transv. proc (TP): thick, arise partly from vertebral body; and shortest TP
- spinous processes: shortest, but thickest
- narrow lateral recesses
- INF ART Facets (IAF): oriented in frontal/coronal plane, whereas the SAF are mostly oriented sagittally
*Movement is possible at L5 due to position of facets

boundaries of vertebral foramen
- formed by the anterior segment (the body),
- and the posterior part, the vertebral arch:
- Pedicle
- Transverse process
- Laminae
- Spinous process

what is shape of LUMBAR vertebral foramina?
triangular in shape; often w/ sharp lateral recesses (esp. L5)

CC: osteoarthritic lipping around vertebral bodies posteriorly can cause…
lateral or central spinal stenosis (narrowing of vertebral canal)

the contents of the vertebral canal or intervertebral foramen can be compressed
CC: Facet joint hypertropy (facet syndrome, osteoarthritis) anteromedially can cause…
lateral spinal stenosis; and anteriorly in foraminal stenosis

the contents of the vertebral canal or intervertebral foramen can be compressed
CC: Spondylosis
(What is it, and what are the sxs)
- any degenerative osteoarthritic change in the spine
- causes impingement upon contents of spinal canal or intervertebral foramen
CC: Lumbar spondylosis w/o acute disc herniation
how common?
nearly as common cause of lumbar nerve root encroachment as disc disease (particularly in the elderly)
In L3/L4, why is there a large interlaminar space between adjacent laminae?
Because laminae in the lumbar region are *not as tall as the vertebral bodies
describe the lumbar spinous processes of L3/L4;
what is the clinical implication?
- lumbar spinous processes are stout, squared off, and do not overlap; these project straight posteriorly
- CC: these make the lumbar spine a good level to do a spinal tap or lumbar puncture
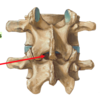
what are the red arrows pointing to? green arrows?
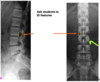
Red arrows: intervertebral foramen
Green arrow: pedicle