Pulmonary Portion Flashcards
what are the three broad types of pneumonia source categories? which one is most common? which are most difficult to treat?
- community acquired pnuemonia (CAP)
**most common**
- healthcare/hospital acquired pneumonia (HCAP)
- most difficult to treat - ventilatror associated pneumonia (VAP)
what are four important ways to reduce ventalator associated pneumonia (VAP)?
- avoid ET tube
- keep head of bed elevated
- reduce sedation
- hand washing
what is important to do once you have finished treating pneumonia?
post treatment xray
want to make sure everything is cleared up and that the treatment has worked!
what is the most common organism seen in pneumoniae overall?
s. pneumoniae
what four patient populations make you at an increased risk for pneumonia?
- ETOH
- asthma
- immunosupressed
- elderly
Typical pneumonia
what are four common organisms associated with this and their characterist sputum color? how long do symptoms increase? what are some of the things on the long list of symptoms
“common symptoms”, usually responsive to B-lactams
#1 most common: streptococcus pneumoniae (rusty red color)
#2: haemophilis influenzae (green sputum)
staph aureus
klebsiella (currant jelly)
pseudomonas (foul smelling)
SX:
1-10 day increase in cough, purlulent sputum, SOB, dullness to precussion, rigors, tachycardia bronchial breath sounds, tactile fremitis (say 99), friction rub, pleuritic chest pain, night sweats
atypical pneumonia
“walking pneumonia”
usually unresponsive to beta lactam, use macrolide or fluorquinolone
1. mycobacteria pneumoniae (bullous myringitis..ear)
2. chlamydia pneumonia
3. legionella
4. viruses->
(RSV and parainfluenze in kids, and influenza in adults)
PE: often normal physical exam, can have extrapulmonary symptoms
DX: use macrolides (erythromycin, azithromycin, clarithromycin, doxycycline) or fluoroquinolones
what are the three most common organisms that cause community acquired pneumonia (CAP)?
#1: streptococcus pneumoniae
#2: haemophilis influenzae (esp in COPD)
#3 mycoplasma pneumoniae (atypical)
what are the three common organisms that cause hospital acquired pneumonia?
- gram negative pseudomonas
- ancinetobacter
- staph aureus
what is the mortality rate in hospital acquired pneumonia?
50-70%
what are the five tests you use to diagnose pneumonia?
- clinical syndrome, empirically
- gram stain- GCP
- sputum culture
- urine tests (only in legionella and pneumococcus)
- xray showing white infiltrate
streptococcus pneumoniae=
pneumococcus
they are the same thing, so if used in a test question, they mean the same thing, its just an abreviated name for this **important since this is the most common organism to cause pneumoniae**
if a patient has pneumonia with MRSA, what should you use to treat?
vancomycin
streptococcus pneumoniae in pneumonia
(what color is the sputum? what is it sensitive to? what can happen if this is systemic? is there a immunization for this?)
- rusty blood colored sputum
- beta lactam sensitivity
- if systemic can cause confusion
**immunizable** this is what the vaccine is for!
what is the treatment for patients with pneumonia? how long is the treatment regimen?
- 80% can be treated as outpatient with macrolide azithromycin/erythromycin/clarithromycin
(atypical or “walking pneumonia)
- if ths same patient has chronic illness combine with beta lactam
- if MRSA infection use vacomycin or fluroquinolone
**5- 14 day treatment**
Explain the new vaccine regimen that is reccomeded?
PVC13: childhood vaccination
PV23: used in 65 +
****new recommendations say 65+ recieve BOTH, adults get PCV13 first then PV23 second 8 weeks later***
if they have already had PV23, wait a year and give PVC13
explain which pneumonia organism these populations are at the most risk to get:
ETOH-
COPD-
CF-
Air-conditioning-
children
Children
ETOH- klebsiella
COPD- haemophilis influenzae
CF-pseudomonas
Air-conditioning-legionella
children
Children
what is the most common lung cancer seen in non smokers?
adenovirus
general bronchogenic carcinoma
“Lung cancer”
what is this the leading cause of? what are the two types? where are the four locations these mets are likely to spread? what is the main cause of these? what are 7 symptoms associated with lung cancer in general?
leading cause of cancer in men and women
made of two categories:
- small cell lung carcinoma
- non small cell lung carcinoma
mets to brain, bone, liver, lymph
SX:
****ASYMPTOMATIC, mostly incidental finding on CXR****
- ***change in nature of cough (squamous, small cell)
- hemoptosis
- vague nonpleuritic chest pain
- reccurent pneumonia
- WEIGHT LOSS ANOREXIA ASTHENIC (CLASSIC)
- HYPERCALCEMIA, don’t miss this
cigarette smoking is the main cause, 85% of lung cancer in smokers

small-cell carcinoma “oat cell”

is this fast or slow? WHERE IS IT LOCATED? what is the doubling time? what are the 6 paraneoplastic syndroms associated with it? what is the treatment? what is the difference between limited and extensive stage?
bad actor!!-grows quickyl metastasizes early!! assume m micrometasizes on presentation!
CENTRAL bronchial epithelium (near hilum because thats where all the vessels are so it can get a lot of nuitrients)
doubleing time: 30 day!!!
limited stage: tumor on the same side of chest, supraclavicular lymph nodes, or both (20% 2 year survival)
extensive stage: anyhting beyond limited stage (5% 2 year survival)
associated paraneoplastic syndromes: cushings, hyponaturemia, SAIDH, periphreal neuropathy, eaton lambert, cerebral degeneration
TX: since it matastasizes so quickly, CHEMO is the treatment
squamous cell cancer

which cells does this occur in? where is it located? how can you dianose/what is major symtom? what is a random paraneoplastic syndrome associated with this? what is interesting about the metastsis of this? who is this most common in?
MOST COMMON NON-SMALL CELL IN SMOKERS!!!
basal cells of bronchial epithelium
centrally located, frequency hemoptysis and change of cough, CAVITATION
hemoptosis diagnosed with cytology
late metastasis–so if you catch it early in the patient the prognosis is better!
paraneoplastic synderome: hypercalcemia
TX: surgical

adenocarcinoma

what is this the most common of? where does the cancer occur and where does it appear? what does it metastasize to? what is the treatment? what are two paraneoplastic syndromes? what can you get it from? smokers or nonsmokers?
most common bronchogenic CA
common in non-smokers
peripheral, lung parenchyma
originates in the mucous glands of tracheobrachial tree and appears in the periphreay of lung
moderate growth and metastatic rate
NON SMOKERS, can get from ASBESTOS!!!
paraneoplastic syndrome: thrombophlebitis, PTH-rp
TX: surgical

large cell cancer
where is this located? what is the doubling time? is there metastasis? what is the paraneoplastic syndrome? what is the treatment?
periphreal or centrally located
cavitation
rapid growth
early metastasis
doubling time 100 days
paraneoplastic syndrome: gynecomastic
TX: surgical

bronchial carcinoid tumor
what type of tumor is this? where else is it commonly found? describe what this tumor would look like if you saw it? what does it secrete (4), what are two symptoms you can have with this? what is the treatment?
CENTRAL neuroendocrine tumor, slow growth, slow mets
also commonly found in GI tract
typical: SESSILE (attached to base) or pedunulated (cylander)
atypical
pink/purple well vascularized central tumor, pedunculated or sessile
secretes SEROTONIN, ACTH, ADH, MSH
often asymptomatic, but can have hemoptosis and c_arcinoid syndrome_ (diareah from increased serotonin and left sided hear fibrosis)
TX: steroids and surgery, resistant to chemo and radiation

what are the three types of non small cell carcinoma?
(NSLC)
1. squamous, (smokers) central with cavitary lesions
2. adenocarcinoma (non smokers), periphreal, Asbestos
3. large cell very aggressive!
which is more common, small cell or non small cell lung carcinoma
non small cell carcinoma
80-85% of LC
where are four most common places for metastases for lung?
liver-common
bone-symptomatic
adrenal
brain
*****which cancer is associated with paraneoplastic type syndromes******
what are the 6?
SMALL CELL CARCINOMA
associated with:
cushings (buffalo hump), cortico levels, hyponaturemia, SAIDH, periphreal neuropathy, eaton lambert, cerebral degeneration
idiopathic pulmonary fibrosis
aka idiopathic interstitial pneumonia
what type of pulmonary condition is this? what is caused by? how long does a patient typically have after diagnosis? what are the three types?

RESTRICTIVE!!
remodeling of the lung to look like honeycomb lung, fibroblasts come in and lay down fibrosis tissue, can be associated with age
dismal prognosis, 3 years from diagnosis
3 Types:
- usual interstitial fibrosis
- respiratory bronchiolitis, associated with this
- acute interstitial pneumonitis

idiopathic pulmonary fibrosis

what are 3 symptoms you would see of this? what are the 3 tests you would use diagnose this? what do you see on them?
SX:
-inspiratory “squeaks” crackles
- clubbing of digits
- progressive dyspnea with dry non productive cough
DX:
1. chest CT:
-diffuse reticular opacities with HONEYCOMBING, ground glass opacities
2. PFT shows decrease FEV1 and FVC, so FEV1/FVC appears normal
3. lung biopsy important for confirmation
idiopathic pulmonary fibrosis
what is the treatment

none, you’re out of luck!!
can give supplement O2 if needed but nothing has been shown to increase survival or quality of life.
lung transplant may be the only choice
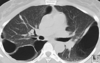
who wants some pics of idiopathic pulmonary fibrosis?
these help to show honeycombing!!

acute bronchitis
What is this condition characterized by? how long does the cough last? what other symptoms might you see? what are 90% caused by (4)? what are the 3 bacteria that cause it in CHRONIC disease? when do you do a CXR?
inflammation of trachea, bronchi, and bronchioles resulting from RTI or chemical irritant characterized by COUGH, often follors URI
COUGH LASTS 10-20 DAYS!!, SEE EXPIRATORY RALES/RHONCHI
90% caused by viruses including rhinovirus, adenovirus, coronavirus, and RSV
in chronic lung disease, commonly caused by: haemophilis influenzae, strep pneumoniae, m cartillis
CXR: ONLY DO IF TRYING TO DISTINGUIS BETWEEN THAT AND PNEUMONIA
acute bronchitis
what are the four OTC treatments for this? what is the DOC for bacterial and what two types of patients qualify for this treatment?
- hydration
- expectorants
- analgesics
- cough suppressants (children)
for bacterial: DOC cephalosporin
-reccomended only for ELDERLY pt with underlying cardiopulmonary disease and a cough for >7-10 days and ANY IMMUNOCOMPRISED PT
***for acute exacerbations in otherwise healthy…..NO TREATMENT NEEDED****
acute bronchitis in normal host
do you treat this patient? what is the requirement for the length of time before giving them treatment? what are the two abx reccomended if they meet the criteria? what is the treatment for the different age groups?
THE TREATMENT WITH ABX IN NORMAL PATIENT HAS NOT BEEN CONFIRMED, use bronchodilators instead because they are more effective at getting rid of cough than abx
exception: >10-14 days, then can treat since this is beyond the viral process and happens in atypical pathogen like mycoplasma pneumoniae, chlamydophilia, pertussis
>55 years old= macrolide (mycins) or tetracycline
>8= doxycycline
bronchiectasis
explain the pathophys of this aka how does this happen? what are the two ways this can happen?
secondary disease that is caused by infection or other conditions that injure the walls of the airways or prevents the airways from clearing mucous. the mucous build up causes increased infection and each infection causes more damange and eventually the airways can’t move air in and out from damage and scarring.
*can be congenital with CF or from obstruction*
*as mucous builds up and stretches everything, the membranes become more floppy and can collapse easier, which is why this is obstructive, not just because of the mucous*

if a patient has bronchiectasis what four infections do you worry about?

1: haemophilis influenzae (most common in world)
the mucous build up creates a perfect breeding ground for pathogens
#2: pseudomonas (CF, #1 cause in US)
- aspergillis (brown sputum)

bronchiectasis

what are the 6 symptoms you would see with a pt with bronchiectasis? what are the 3 tests you would do to test patient for this? what would you see on these?
- recurrent pneumonia
- chronic cough
- hemoptysis (50-70%), bronchiectasis is main cause of this
- foul smelling mucopurlulent sputum
- clubbing (as seen with CF)
- crackles at base
DX:
- high resolution CT; imaging of choice, dilated tortuous airways
2. CXR; crowded bronch markings, basal cystic spaces, Tram Track markings (bronchial wall thickening), honeycombing, signet ring sign (pulmonary artery coupled with dilated bronchus)
3. bronchoscopy warrented to eval hemopytsis and remove secretions

bronchiectasis
what are the 4 treatment options?

- ABX for 10-14 days for infections
- supressive therapy
- bronchodilators
- lung transplant

solitary pulmonary nodules
what is the nickname for these? what makes it likely defined? what percent are benign/maligant? how do you diangnose? what are the three treatment for high, medium, and low maligancy risk?
“coin lesions”, KEEP IN MIND THIS IS THE FIRST MANIFESTATION OF ANY TYPE OF LUNG CANCER, THIS ISN’T A CANCER TYPE BUT THE CLASSIFICATION FOR ANY FIRST APPEARNCE OF CANCER
Defined:
Most at asymptomatic
60% benign, 40% malignant
often infectious granulomas from old reactive TB, fungal infection, or foreign body rxn
DX:
- CT for nodules
- PET for >1 cm and intermediate probability
TX: if high probability….RESECT LESION
if intermediate……biopsy
if low… can be watched, need CT every 3 months for a year, then decrease to every 6 months for two years
if

what is kartagener syndrome? what is it associated with?
associated with bronchiectasis
classic triad:
- sinusitis
- situs inversus
- infertility
what are three symptoms that can help push you towards cancer?
- hemoptosis
- fever
- weight loss
sarcoidosis

what is this condition? what type of cells respond to this? what percent of people have lung involvment? what is the intial lesion called? and what about when its progressed? what are the 6 common parts of the body that it effects?
MULTISYSTEM DISEASE MADE OF NONINFECTIOUS NONCASEATING GRANULOMAS CAUSING INFLAMMATION IN INVOLVED ORGANS
the granumlomas form in response to exagerated T cell response, these granulomas “masses” take up space and disrupt organ function
90% have lung involvement
- initial lesion in lung called: CD4 T cell alveolitis*
- progression of disease: transforms into noncaseating granuloma*
most effected: 1. pulmonary 2. lymphadenopathy (_hilar lymph nodes_) 3. skin (erythema nodosa) 4. lupus pernio 5. PAROTID ENLARGEMENT 6. visual defects (20%)

what are the three tests you can do to confirm sarcoidosis?

1. serum blood tests
-Leukopenia
-eosinophilia
-elevated ESR
-hypercalcemia
-hypercalciuria
2. CXR
billateral hilar lymphadenopathy
2. elevated angiotensin (40-80%)
3. needle biopsy needed to confirm noncaseating granulomas

what percent of people with sarcoidosis can be asymptomatic?
what is the treatment?

50% can be asymptomatic
Very responsive to high dose corticosteroids!

what percent of solitary pulmonary nodules are primary lung cancer?
75%
what is the structure of influenza? what family? what types?
- single stranded RNA
- orthomyxovirdae family
- A, B, C types