Cardiac Portion Flashcards
myocardial ischemia
what is this and what is it caused by (3)? what determiens the severity? what are 3 contributatory factors? what how does it present as symptoms? what causes these symptoms in each?
temporary reduction of blood flow to an organ, potentially reversible, caused by mechanical, electrical, and valvular dysfunction
can be reversible or peremanent depending how long it has been happen for, can lead to infarction
this can cause angina when there is increased activity
Contributory factors: significant LVH, aortic stenosis, tachyarrythmias like afib/aflutter
symptomatic:
1. angina pectoris
1. O2 demand in the presence of fixed stenosis
- VASOSPAM and significant narrowing
1. prolonged decreaed O2=unstable angina or infarction
-acute thrombis likely present
sudden cardiac death in CHD
how soon does the pt die? what most likely causes it? when does this happen?
1. death within 1 hour after onset of symptoms usually within minutes
2. malignant arrhytmia commonly present
common presenting manifestation of CHD, frequent end point in patients with CHD propr to MI and imparied LV function
why are women often misdiagnosed when they have CHD? (3)
1. atypical symptoms: pain radiating to right arm, arm pain along
- many women produce false negative stress tests since single vessel disease more common
3. elderly or diabetic womeon complain of general malaise, loss of appetite, vague abdominal pain so if they have RF, GET EKG!!
stable angina pectoris
what does this pain feel like? is it reproducible? what are 3 things that make it better? what is the pattern? what are 6 things that can cause this? what are 4 things you might see to clue you into this?
chest discomfort described as
tightness, pressure, aching, choking that is often REPRODUCIBLE WITH ACTIVITY that resolve after cessation of activity, relaxation, or NTG
positive levine sign substernal to left sternum, with crescendo/decresendo pattern 1-5 mins, less likely to happen in AM (lower threshold)
can be brought on by: exertion, exercise, emotional stress,cold weather, cigarettes, sex
physical exam may be normal between episodes, may see xanthomas from hyperlidemia, AV nicking from HTN/DM, s4 gallop during angina, changes in BP
what are the 3 tests you can do to help identify stable pectoris for CAD? what do they show?
1. EKG:
normal between episodes
ST segment depression/T wave change during angina then normalize after angina passes
2. Stress EKG: most helpful non invasive tool
-increase workload with meds or exercise, compare resing and stress EKG for ischemia, may consider adding image to make it more specific, ability to detect dermines the amoutn of vessel involvment
3. coronary angiography- Gold standard for CAD
-tells which vessels are involved, degree of stenosis, and LV function
what is the drug you give for acute angina pectoris? or for prophylaxsis if the pt is going to be doing exercise?
sublingual NTG
reduces LV volume preload and decreasing O2 consumption
does this by causing venodilation, so that it decreases the amount of blood heading back to the heart, decreasing the volume and decreasing O2 demands
what are the 7 drugs you put someone on to help with chronic stable angina?
1. beta blockers ATENOLOL, METOROLOL: decreases HR, contractility, and BP improving exercise tolerance
*****REDUCE MORTALITY IN POST MI AND HF PATIENTS***
2. long acting nitrates isosorbide dinitrate
****DONT TAKE THIS WITH VIAGRA!!!!*****
****can develope nitrate tolerance so need to dose in intervals!!****
3. Non dihydropyridine calcium channel blockers dilate ARTERIES, decreasing afterload, decrease myocardial O2 consumption
4. dyhydropyridine calcium channel blockersamlodipine, nifedipine dilate ARTERIES, decrease afterload and myocardial O2 consumption
***best used in combination with a BB, reduce risk of HYPOTENSION**
5. diltiazem and verapamil used with nitrates, dilates arterioles decreasing afterload, decrease HR, and O2 consumption
***don’t use in HF patients!!***
6. ranolazine chronic angina that isn’t controled with the above
**increase QT interval, but won’t cause arrythmia**
7. antiplatelet drugs USED IN ALL PTS WITH CHD, PAD, AND CAROTID, DECREASES INCIDENCE OF CARDIAC DEATH AND MI, low dose asprin
what drug do you not want to use in CHD in a patient that has asthma/COPD because it can cause bronchospasm?
nonselective beta blockers
Use selective beta blocker!!
what two drugs decrease the mortality post MI and in HF patients?
Beta blockers
Atenolol and metoprolol
what 4 groups of patients with CHD qualitfy for revascularization?
1. patients with unacceptable symptoms controlled with meds
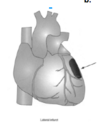
2. 3 vessel CAD with LV dysfunction OR left main coronary stenosis that compromises Left anterior descending (LAD) LEFT main artery consider CABG!!
3. patients post MI with ongoing ischemia
4. acute MI
when should percutaneous coronary revascularization/catherterization be used for CHD?
what are the rates of restenosis with angioplasty, stent, and drug eluting stent? what do you do to compensate for this?
angioplasty restenosis rate: 30-40%
angioplasty with stent placement: 15-20%
drug eluting stents restenosis: 5-8%
- single or 2 vessel disease
- 3 vessels disease in pt that doens’t qualify for operative
drug eluting stents helped decrease rates of restenosis a lot, however probles with late thrombosis so requires intense anti-platelet RX of ASA and clopidogrel
coronary artery bypass for CHD
what happens during this procedure? which two vessels are most commonly used? which one is the best one to use and why? what two factors increase mortality rates?
coronary arteries are bypassed using arteries or veins, low mortality if LV preserved
saphenous veins and mammary arteries most commonly used
internal mammary artery graft has highest patency rate over time**BEST OPTION WHEN POSSIBLE because arteries last longer than veins**
mortality increase with age and EF
coronary vasospasm
what can bring this on? what does the spasms cause? what will the pt feel and what will you see on the EKG? what can happen if this doesn’t resolve?
can be in normal cornary arteries or superimposed o atherosclerotic ones, the spasms cause the artery to close
often induced by cold, emotional stress, meds, and cocaine
angina at rest with ST elevation
**can progress to MI if symptoms don’t resolve**
prinzmetals angina
what is this caused by? when do you get symptoms? who is it more common int? what does arteriography show? what are the two treatment options?
coronary ishchemia from vasospasms
symptoms at rest, usually in AM
women> men
ateriography shows normal looking arteries
Tx: nitrates and calcium channel blockers (dihyrdopyridines)
what percent of people with unstable angina remain unstable and need revascularization?
what percent improve medically? and what do you need to do before allowing them to leave?
20% will remain unstable and need revascularization
80% will get better clinicallly and need to get stress test once stable, if they produce a positive test then it might be an indication for revascularization
unstable angina
what is this? what are you at high risk for? how do you differentiate between this and a NSTEMI? what are the two presentations of this? what are two things you do to diagnose this? what are the two things you need to do for tx and the three drugs they need to be on?
angina at rest with minimal activity >10 minutes
GET VERY CLOSE TO HAVING A MI BUT DONT, RIGHT AT THE BRINK OF CELL NECROSIS BUT TISSUE HASN’T DIED YET, high risk for developing MI in following days/weeks so much treat aggressively and quickly
VERY SIMULAR TO NSTEMI, except in unstable angina negative cardiac markers
new onset: angina
accerating or cresendo angina in pt with previously stable angina (gets worse doing less activity)
DX:
NEGATIVE CARDIAC ENZYMES
EKG: ST depression, T wave inversion
Tx:
- HOSPITALIZE THEM!! BEDREST!!
- full anticoagulation and antiplatelet therapy
-HEPARIN +ASA+
prasurgrel/ticagrelor/clopidigrel OR glycoprotein IIb/IIIa
3. nitrates, Beta blockers, and Ca-blockers to decrease MVO2
what percent of people with unstable angina will have abnormal EKG?
50%
so worry about the 50% that have a normal one, still might need to work them up
since the pathology of unstable angina and NSTEMI are the same….what is the only thing that you use to tell them apart?
cardiac enzymes
ck-creatine kinase
MB
troponins
these indicate cell death and that the scale has tipped over the point of unstable angina and cell death is occuring, this is a myocardial infarction
non-stemi acute myocardial infarction
what is this caused by? what is this nickname for these? relate to morality? why must we treat aggressively? how do you differentiate between that and unstable angina?
infarcts caused by prolonged ischemia
CAD to plaque rupture to platelets to clotting to thrombus
small infarcts that are unstable and could go on to cause a bigger infarct so that is why we treat aggressively
“incomplete infarcts” with lower initial mortality but high risk of re-infarction with HIGH MORTALITY
DX: like unstable angine with POSITIVE CARDIAC ENZYMES
acute myocardial infarction
STEMI
what is the cause of this? what does it lead to? what does patient complain of? what does this most likely occur? how does the patient appeare (3)? what often accompanies this? what are 6 signts of this? what are the 5 things you use to diagnose this?
prolonged ischemia resulting from inadequate tissue profusion leading to cell death and necrosis
total occulsion CAD to plaque to rupture to platelets to clotting, to occlusive thrombus
“elephant sitting on my chest and the worst pain I have felt in my life”
often early in the AM since coronary tone, SEVERE PAIN, anxious, diaphoretic, and distress, LV dysfunction
variable pulse and BP, S4 gallop, apical mitral regurgitation, cold, cyanotic, low CO, ST elevation
DX:
- Creatinine kinase (CK) ALWAYS ELEVATED!
check CK-MB, specific to damanged heart muscle
2. troponins cTnl represents muscle breakdown, sensitive to small infarcts
3. leukocytosis
4. EKG ELEVATED ST
5. echo left ventricular function, identify mitral regurge
what are the treatments for a acute STEMI? (3)
1
1
2
1. percutaneous coronary intervention to reprofuse tissue (CATH)
- goal: open artery within 3 hours of onset of symptoms
goal: open atery within 90 mins presenting to hospital
***If within hour and a half of hospital that does this, consider transfer!!! Must also have CABG CAPABILITY****
2. thrombolytic (finbrinolytic) therapy: done if no access to cath lab, t-PA (altepase)
-done when ST elevation >1 mm in tow or more adjacent leads
50% reduction in mortality if given withint 1-3 hrs of symptoms
3. post thrombolytic management
a. ASA ongoing
b. heparin 24 hours
acute myocardial infarction
STEMI
what is the cause of this? what does it lead to? what does patient complain of? what does this most likely occur? how does the patient appeare (3)? what often accompanies this? what are 6 signts of this? what are the 5 things you use to diagnose this?
prolonged ischemia resulting from inadequate tissue profusion leading to cell death and necrosis
total occulsion CAD to plaque to rupture to platelets to clotting, to occlusive thrombus
“elephant sitting on my chest and the worst pain I have felt in my life”
often early in the AM since coronary tone, SEVERE PAIN, anxious, diaphoretic, and distress, LV dysfunction
variable pulse and BP, S4 gallop, apical mitral regurgitation, cold, cyanotic, low CO, ST elevation
DX:
- Creatinine kinase (CK) ALWAYS ELEVATED!
check CK-MB, specific to damanged heart muscle
2. troponins cTnl represents muscle breakdown, sensitive to small infarcts
3. leukocytosis
4. EKG ELEVATED ST
5. echo left ventricular function, identify mitral regurge
what are the treatments for a acute STEMI? (3)
1
1
2
1. percutaneous coronary intervention to reprofuse tissue (CATH)
- goal: open artery within 3 hours of onset of symptoms
goal: open atery within 90 mins presenting to hospital
***If within hour and a half of hospital that does this, consider transfer!!! Must also have CABG CAPABILITY****
2. thrombolytic (finbrinolytic) therapy: done if no access to cath lab, t-PA (altepase)
-done when ST elevation >1 mm in tow or more adjacent leads
50% reduction in mortality if given withint 1-3 hrs of symptoms
3. post thrombolytic management
a. ASA ongoing
b. heparin 24 hours
what are 3 drugs taht might be used to try to help in a actue MI early on pre hospital or in the ED?
- morphine sulfaste
- aspirin in ED
- nitro IV
what are the contraindications (4) and realtive contraindications (1) for thromboltic therapy for a STEMI?
absolute contraindications:
- uncontrolled HTN
- stroke within 1 year
3. cerebral hemmorahage
4. recent head trauma
relative contraindications:
- abdominal or thoracic surgery within 3 weeks
what are 3 drugs taht might be used to try to help in a actue MI early on pre hospital or in the ED?
- morphine sulfaste
- aspirin in ED
- nitro IV
what 5 medications is a person who had a STEMI put on after intervention or thrombolytic therapy?
1. BETA BLOCKERS: decreases wall tension preventing MI complications, decreases morality!
2. nitrates
2.5 heparin
3. asprin/clopidigrel
4. ACE inhibitors: i_mprove short and long term survival, decrease LV remodeling post MI,_** great for **large infarcts
5. alosterone blockers
6. statins LDL goal
what are the drugs that you use to treat unstable angina or NSTEMI?
- full anticoagulation and antiplatelet therapy
-HEPARIN +ASA+
prasurgrel/ticagrelor/clopidigrel OR glycoprotein IIb/IIIa
- nitrates
3. Beta blockers
4. Ca-blockers
explain when the CK MB isoenzymes rise, peak, and fall?
rise: 4-6 hours
peak: 16-24 hours
fall: 2-3 days
explain when the troponin cTnI rise, fall, and stay elevated? what is diagnostic? what is good about this test?
rise: 4-6
peak: 8-12
remains elevated: 5-7 days
dianostic if >.1, abornal if >.05
This test is the most specific and sensitve, can test for small MI
in a failing heart you get________
so the body tries to compensate by increasing ______
in a failing heart you get decreased stroke volume
so the body tries to compensate the decreased cardiac output by increasing sympathetic control to increase contractility, but the volume it is pumping out still isn’t as much as a normal heart
in HF, how doese the body attempt to increase cardiac output?
- if cardiac output is low and can’t support normal circulatory function, body stimulates sympathetic stimulation to increase vasoconstriction and venous return
- causes increase in RA pressure and fluid retention at kidneys because of decreased filtration rates from decreased cardiact output
- cardiac output rises a little from fluid retention and increased venous return
- continue to increase right atrial pressure, fluid retention accelerates this causes overstretching of the heart of edema of the heart muscle
- cardiac output drastically decreases and the pt dies of DECOMPENSATION
sinus rythmn
rate?
rythmn?
p waves?
QRS?
rate 60-100
rythmn regular
p waves yes and upright
QRS narrow

sinus tachycardia

rate?
rythmn?
p waves?
QRS?
causes?
rate >100 bpm
rythmn regular
p waves yes
QRS narrow
causes:
1. normal, seen with exercise
2. changes in SA node firing seen with CHF, lung disease, hyperthyroidism in eldery
sinus bradycardia
rate?
rythmn?
p waves?
QRS?
causes?
rate?
rythmn? regular
p waves? yes
QRS? narrow
causes? common rythmn seen in early stage of acute MI
sinus arrythmia

rate?
rythmn?
p waves?
QRS?
causes?
rate? slight irregularity of sinus rythmn
rythmn? slightly irregular
p waves? yes
QRS? narrow
1. phasic speeding up with inspiration and slowing down with expiration
2. variation in vagal tone as result of herring breuer reflex
premature atrial contractions

rate?
rythmn?
p waves?
QRS?
other? 3
ATRIAL RE-ENTRY or increase AUTOMATICITY, premature atrial depolarization

rate? single beat
rythmn? premature complex
p waves? yes, but looks different than a regular p wave
QRS? narrow
other?
1. if early coduction can be blocked at AV node
2. if there is no preceeding p wave then it is called junctional premature beat (only difference)
3. can appear as bigeminy, trigeminy
atrial fib

rate?
rythmn?
p waves?
QRS?
other? 3
MULTIPLE REENTRANT CIRCUITS IN THE ATRIA
rate? 400-600 atrial contractions (blocked at AV by refractory period)
rythmn? irregullarly iregular supraventricular
p waves? NO!!! undulating baseline
QRS? narrow QRS
other:
- in new onset without med control: ventricular rate is very fast 120-180 bpm
- goal in ED: slow rate with meds
- Risk: BLOOD CLOT and stroke if they break off
atrial flutter

rate?
rythmn?
p waves?
QRS?
other? 4 things!
RENTRY CIRCUIT around annulus of tricuspid valve
250-350 flutter waves
regular
no p waves, flutter waves
QRS narrow
- most common presentation is 2:1 AV block with QRS ~150 bpm
- SAW TOOTH APPEARANCE in II, III, aVF
- after meds given to slow AV conduction given, most common form of block is 4:1 with ventricular rate ~75
- carotid masage can help slow VR down, allowing flutter waves to be seen
paroxysmal supraventricular tachycardia (PSVT)
rate?
rythmn?
p waves?
QRS?
who is it in? tx? 3 causes?
AV NODAL REENTRY!
abrupt onset and termination
carotid massage may help terminate
150-220
regular
not usually present
narrow QRS
- most in young healthy people without cardiac disease, can tell you the second it started and stopped. cardiovert with adenosine 90-95% of the time if carotid massage doesn’t work
- can be caused by coffee, alcohol, and excitement

multifocal atrial tachycardia
what must be present?
rate?
rythmn?
cause?
what is it connected to?
enhanced automaticity
3 or more p wave morphologies present, irregullarly irregular, >100 bpm
usually underlying pulmonary pathology present
junctional escape rythmn

what is this caused by?
when can it happen?
rate?
QRS?
p waves?
what can happen if sinus rate and AV rate are similar?
caused by the sinus slowing or sinus arrest so that the AV node takes over
**can occur during sleep due to increased vagal tone, if sinus rate slows during sleep, this takes over**
40-60 bpm
narrow QRS
no p waves usually seen
ususally well tolerated
may compete with sinus rythmn if rates similar
premature ventricular contractions (PVCs)

what is this the most common of?
reentry or automaticity?
QRS? p waves? rythmn? after? shape? what type of hearts? pattern?
most common ventricular rythmn
reentry more than automaticity
premature QRS complex that is wide and biazarre
no p waves
WIDE QRS >.12
irregularlly iregular, or regularly irregular (trigeminiy)
often followed by a pause
uniform or multiform
healthy and diseased hearts
bigeminy and trigeminy

junctional tachycardia
what is this chracterized by? what can it be confused with? what are two clinical connections?
very uncommon, but discussed for ACLS
NARROW QRS REGULAR TACHYCARDIA WITHOUT P WAVES
may be confused with PSVT but slower rate
clinical: digital toxicity, somtimes inferior wall MI
ventricular tachycardia
what is this defined as?
what is sustained mean?
is the heart diseased?
hemodynamicaly stable?
what does it deteriorate into?

3 or more consective PVCs at rate >100
sustained: >30 seconds
more often uniform and regular, but can be irregular like torsades
seen in presence of structual cardiac pathology
rarely hemodynamically stable
deteriorates into vfib
torsades de points

what type of vtach is this?
what is it associated with?
what does it turn into?
“twisting of the fingers”
polymorphic vtach, very fast, very dangerous, 200-300, pt unconcious
associated with prolonged QT interval
difficult to treat and turns into vfib

ventricular fibrillation
what is this? does it contain any waves?
terminal arrhythmia associated with death
DEFIB ASAP (if you are outside the hospital pt will likely die but if happens at the hospital, the pt will likely live depending on how long it takes you to defib them)
UNDILATIONS ONLY, choatic oftren preceeded with vtach
rarely seen in pts with structually normal hearts
mitral regurgitation
what happens in the pathophys for this? what can you get? what are the common 3 symptoms patient presents with? what are the five descriptors used to describe this? what are two things you might see on EKG? what will you see on echo?
most common valvular condition
left ventricle backs up into left atria, both dilate overt time
increase in LA pressure, and LVEDV
backup causes pulmonary sxs
sx: DOE, orthopnea, symptoms of left HF and eventually right HF if backs all the way up through the lungs
Holosystolic systolic murmer (heard throughout entire systole), THRILL, HIGH PITCHED BLOWING, S3 gallop if severe
DX:
EKG: LA enlargement, often Afib!
echo: LA and LV dilation but decrease in function
In MOST murmers, what would you expect to see in results when squatting down and standing up quickly?
WHAT IS THE EXCEPTION OT THIS?!
squatting down: increases the volume of the heart and venous return making the murmer WORSE
standing up: decreases the venous return making the murmer less noticeable
mitral valve prolapse is opposit!! since large leaflets, making the heart bigger actually decreases the murmer (sqautting) because the leaflets fit better. Standing makes it worse because now you have the extra tissue!
what are the four tx options for mitral regurg? what must you consider regarding surgery?
- decrease activity
- ACE INhibitors esp in HTN or HF, decrease preload and after load
- diuretics decrease preload
- sugey!! if decreased EF or LV dysfunction with progressive sxs
***the timing of sugery is really important because need to do it before you get left ventricular failure from response to stress, otherwise the valve only helps to much****
repair better than replacement here
what are the five most important descriptors for mitral regurg?
- Holosystolic systolic murmer (heard throughout entire systole), 2. THRILL
- HIGH PITCHED
- BLOWING
- S3 gallop if severe
what are two random defomirites that are associated with mitral valve prolapse?
high arched palate
pectus excavatum!!
weird
mitral valve prolapse
What happens in this? what are the two causes of this? which is most common? and what two systemic conditions can cause this? what does this present with for symptoms? what else can be present? what are the 3 key PE things you see?
abnormal connective tissue growth causing the leaflets to buckle
caused by:
- familia hx, most common autosomal dominant (only get growth on valve)
- systemic connective tissue disease MARFANS, EHLERS danlos
SXS: ususally asymptomatic but in women presents as ATYPICAL CP thats “FLEETING” with palpitations, Arrythmias present
mid to late systolic click between s1 and s2 (tensing of chordae), high pitched late systolic murmer,
NOISE/MURMER SOFTENS WHEN SQUATTING KEY THIS MAKES HEART LARGER SO LEAFLETS FIT BETTER, OPPOSIT OF OTHER MURMERS
mitral valve prolapse
what are the 3 PE things you might find to indicate this?
- mid to late systolic click between s1 and s2 (tensing of chordae)
- high pitched late systolic murmer
- NOISE/MURMER SOFTENS WHEN SQUATTING KEY THIS MAKES HEART LARGER SO LEAFLETS FIT BETTER, OPPOSIT OF OTHER MURMERS
what are the 3 tx options for mitral valve prolapse?
- reassurance #1!!!!!
- Beta blocker if CP or arrythmia
- surgery if MR severe (VERY RARE!!))
mitral stenosis
what condition cases this? what happens to the valve..what is the nickname for this appearance? does it effect the lungs? how wide does the opening need to be? what becomes the issue? what are the symptoms? hat rythmn is common? what would echo show? what are the four PE findings for this?
only caused by rheumatic fever
leaflets thicken and calcify narrowing the space cause “FISH MOUTH DEFORMITY”
can back up to the lungs
diastole becomes the issue because it can’t fill
SXS: DYSPNEA, orthorpnea, pulmonary edema, AFib common
DX: eco: abnormal valve motion, LAE
LA DILATION, LV NORMAL WITH LVEDP NORMAL!! s1 and s2 loud, opening snap after S2, diastolic rumble low pitch from slow blood flow into LV
what are the 4 PE findings for mitral stenosis?
- LA DILATION, LV NORMAL WITH LVEDP NORMAL!! (just not getting blood)
- s1 and s2 loud
- opening snap after S2
- diastolic rumble low pitch from slow blood flow into LV
what are the 4 treatment options for mitral stenosis?
- decrease Na consumption, direutics
- control afib if present
- preferred intervention: precutaneous balloon vulvoplasty (alternative to surgery, first option for most patients)
- surgery if repair by #3 doesn’t work/can’t work
aortic stenosis
what are the 3 causes of this? which is most common? what the two many symptoms you see with this? what is the hallmark in pathology? what must it narrow to? what are the 6 characteristics of this condition?
Males!
three main causes:
- born with bicuspid valve
- rheumatic fever
-
IDIPATHIC, wear and tear in eldery (sclerocacific), MOST COMMON
sx: DOE, angina pectoris, syncope with exercise ( periphreal vasodilation with decrease CO)
hallmark: left ventricular pressure higher than aortic pressure in systole, L sided heart failure, angina pectoralis (since heart has to work so hard to overcome increase in pressure, it requires more blood but the opening for coronary arteries is on the other side of this valve!)
carotid pulses climb, apex displaced, s4 gallop, systolic murmer with cresendo/decresendo, sawing gratting sound during systole, harsh low pitch
what are the 6 main things to remember about aortic stenosis sounds?
what two pt symptoms key?
- carotid pulses climb
- apex displaced
- s4 gallop
- systolic murmer with cresendo/decresendo
- sawing gratting sound during systole
- harsh low pitch
patient sxs: syncope, angina pectoris
what must you determine aortic stenosis from? what do you do to determine between the two?
aortic sclerosis
thickening/calcification without fusing, don’t have symptoms
need to get echo to determine between the two?
what do you need to do before surgery for aortic stenosis? what does this help you determine?
cath
identifies gradient between LV and aorta, and determines the presence/absence of CAD since these can opften go together.
**want to distinguish if pt gets angina pectoris from block in the coronary=CHD, or just no blood flow =aortic stenosis*
what are the 3 surgery options for aortic stenosis?
if surgical candidate, get surgery
- mild w/o symptoms: monitor, ACE, ARBS
- SURGERY!!! replacement with tissue or mechanical valve
- balloon valvuloplasty/transcather aortic valve implant- palliative for those who aren’t surgical candidate…except in young adults
where do you hear aortic stenosis? what can help make it easier to hear?
2nd RICS
patient sitting leaning foward
what do you hear mitral stenosis and what can make it easier to hear?
apex
left lateral debiscus position
tricuspid regurgitation
where do you hear it?
during what?
where does it radiate?
noise?
whats often elevated?
what can it icnrease slightly with?
heard: lower left sternal border
holosystolic, pansystolic
radiates: right sternum to xifoid area
blowing noise
JVP often elevated
increases slightly with respiration
pulmonic stenosis
where do you hear this?
where does it radiate?
what might you hear?
when do you hear it?
heard: 2-3rd left intercostal spaces
readiates to: left shoulder and neck
early pulmonic edjection sound heard
timing: systolic
SICK SINUS SYNDROME
WHat does it encompass?
who do we see it in? why?
what can cause it or it be a result from?
is it reversible?
what is it characterized by and what are the three types?
CLinical presentaiton?
DX
TX
- encompasses physiologically inappropriate sinus bradycardia, sinus pause, sinus, arrest, or episodes of alternating sinus tachy and brady.
most often in elderly: caused by scaring of the hearts conduction system
could occur in an infant who had heart surgery
- may be causes of exacerbated by digitalis, calcium channel blockers, beta blockers… so on and so on.
- also could result from underlying collagen vascular or metatastic disease or surgical injury
REVERSIBLE if caused by digitlalis, quinidine, beat blockers , or aerosol propellants
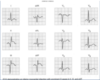
- AV block is characterized by refractory conduction of impulses from the atria to the ventricles through the AV node or bundle of HIS and divided into 1st degree, 2nd degree (Mobitz 1 or mobitz II) and complete 3rd block
- FIRST degree heart block: all atrial beats conducted to the ventricles, PR interval is greater than 0.21 seconds
- SECOND degree heart block: not all atrial beats are conducted to the ventricles
- Mobitz type 1 (wenckebach) is has lengthening of PR interval with shortening of RR interval. All atrial impulses will not be conducted to the ventricles. Typical pattern is repeated cycle of: normal PR interval, long PR, longer PR, even longer PR, and dropped beat. This is due to abnormal conduction in AV node
- Mobitz type II: non conducted atrial beats. block within HIS bundle system. secondary to organic disease involving infra nodal system. can progress to complete heart block
- THIRD degree heart block: (complete) complete dislocation between atria and ventricles. due to lesion distal to the HIS bundle
Clinical Prenenstation:
most asymptomatic, but may have syncope, dizziness, confusion, HF, palpitations, or decreased exercise tolerance
- 1st degree AV conduction block usually asymptomatic.
- higher grade blocks may have weakness, fatigue, light headedness, syncope
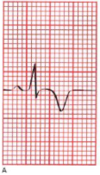
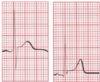
DX: ECG changes (SEE PICTURE)
TX:
permiinnant pacing
1st degree AV conduction block require no tx
- only effective long term tx for other AV conduction disorders is permanent cardiac pacing
- temporary transthoracic or transvenous pacing should be followed by permanent pacing when Mobitz type II or complete heart block dx.

sick sinus syndrome
sinus arrest with alternations of paroxysms or atrial tachycardia and bradyarrythmias
caused by sinoatrial disease
tx: permanent dual chamber pacer with auto ICD
chronic artieral insufficiency
BATES:
1. intermittent claudication, progressing to pain at rest
2. PALE ON ELEVATION, DUSTY red when laid down
3. ulceration on the toes or points of trauma
4. COOL temp of limb
5. thin, shiny, atrophic skin, loss of hair on legs
atherosclerosis
what size arteries does this involve? what forms and where? what does this make and what is it made up of? what does it lead to? what are three example conditions that are caused by atherosclerosis?

medium and large artery
gradual plaque formation on the intima of the medium/large vessels of ATERIES, material grows under the endothelia layer creating plaques: fat cholesterol and calcium
leads to:
gradual reduction in aterial lumen that prevents oxygen rish blood from geting to the tissues causing ischemia
the location of the arteries determines the name of the disease AKA
- coronary heart disease (coronary artery disease)
- cartotid artery disease
- periphreal vascular disease

what are 9 risk factors for atherosclerosis?
which two are the most important?
- smoking
- diabetes mellitus
- dyslipidemia
- elevated CRP
- hypertension
- family hx in 1st degree relative
- males
- inactivity
periphreal vascular disease
what is this condition? what type of involvment, occuring where? what is it the leading cause of? what are the 3 MOST IMPORTANT RF? what are the four must important symptoms, which one is most important? when does this come on and when does it stop and where does it occur? in sever disease, what are four things that can happen?
atherosclerosis of the extremities, segmental involvement often at branching points!!!!
leading cause of occludive arterial disease in pts over 40
RF: DIABETES MELLITUS, SMOKING, >60YRS
claudication symptom most common (pain, aching, cramp, numbness or fatigue of muscle during exercise and relieved by rest!! claudication symptoms occur distal to stenosis), dimished distal pulses, hair loss with shiny skin appearance, with elevation of extremities get pallor of soles of feet and rubor (redness) in the leg, bruits in artery
in severe: pain at rest, ulceration, necrosis and gangrene from ischemia from lack of blood flow

in periphreal arterial disease, if you have a clot in these areas, where will the claudication symptoms radiate?
aorti-iliac
femoral popliteal
aortoiliac: radiates to butt, hip, and thigh pain
femorapopliteal: radiates to calf
claudication is…..
distal to the site of stenosis
Think about it. if you have a clot in your leg, your blocking the distal tissue from getting blood, so this is where the ishchemia happens and this is where the symptoms appear!
periphreal arterial disease
what are the three tests you can do to help diagnose it?
- ankle/brachial index (higly sensitive and specific, compares systolic BP in brachial atery and posterior tibial artery) values less than .9 suggest PAD (ankle/arm) PRESSURE IN THE LEG DECREASES since isn’t being profused with blood
2. duplex US, pulse wave doppler
3. contrast angiography **GOLD STANDARD** and definitive, done before endocasulcar or surgical revascularization
periphreal arterial disease
what are the 5 treatment options for PAD?
GOAL: prevent progression
1. lifestyle modification
-control glucose, BP, decrease BMI, stop smoking!!!
2. exercise: suprevised walking program
walk until pain comes on, stop, rest, and then begin again, creates collateral artery formation 30 mins 4x week PROVEN TO WORK BETTER THAN ANY DRUG!!
3. asprin/clopidigrel as secondary prevention to prevent against MI, STOKE, Death
- cilostozol: only drug shown to help improve the symptoms of PAD other than a walking program, but not great, increased walking distance by 35%, this is PDE inhibitor, increases cAMP and prevent platelet aggregation and promotes flow by vasodilation
5. revascularization
how much can a supervised walking program increase pain free walking by?
150%….most important because it has shown to work better than any drugs!!
periphreal arterial disease
explain in extreme cases what the two options are for revascularization? Who is it appropriate for?
improves quality of life for pts with DISABLING CLAUDICATION ALREADY ON MAXIMUM THERAPY AND HAVE REST PAIN. PRESERVE LIMB VIATALITY AND PREVENTS AGAINST AMPUTATION
1. endovascular revascularization: angioplasty with a stent to restore blood flow, decreased complications over surgery
2. surgery to bypass: fancy plumbing, anticoagulation with heparin to prevent propogration of the thrombus
acute aterial occlusion

what is this caused by and why is it acute? what are the 5 common causes of this? what are the four risk factors that you want to control? what are the 5 symptoms? what are the three things you use to diagnose it and which is the gold standard? what is the treatment option? and what are the 2 tx options if it is severe?
caused by embolism since happens quickly, something travels and blocks the artery , thrombus in situ
most common causes: afib, ventricular aneurysm, anterior MI, prostetic valve, thrombis at site of stenosis
RF: smoking, control of DM, HTN, hyperlipidemia so NEED TO CONTROL THESE!!!
rapid onset of pain, parenthesia, numbness, coldness in involed extremity, loss of distal pulses
DX: doppler US (DO FIRST), ABI, angiography gold standard
Tx:
1. anticoagulation with heparin to prevent propogation of the thrombus
2. if severe: reprofusion
- embolectomy
- streptokinase, urokinase, tPA

what are the symptoms that suggest an acute arterial occlusion is an emergency?
6 p’s
- pain
- pallor
- pulselessness
4. parenthesia
5. poikilothemia
6. paraylysis
these indicate tissue could die and threatens limb vitality so what to get vascular on board stat to hopefully prevent amputation

chronic venous insufficiency

what does this most commonly come from? what four other things can cause it? what are the 2 contributing factors to this? what are the 6 symptoms/exam findings you will see? when is it the worse? what can it lead to? what are the three tx options?
can result as consequence of both DVT (75% of the time) and superficial venous insufficiency
other causes: varicose veins, trauma, neoplastic venous obstruction
veins become functionally inadequate due to damage of the valves which results in bidirecitonal flow, and loss of venous wall tension that results in stasis
gradual progression of leg edema from ANKLE TO CALF!! OFTEN PAINFUL!!! NORMAL LIMB TEMP! pools at the bottom. shiny skin, skin ulcers, cyanotic aching when standing, edema worse at the end of the day, and best in the morning, secondary skin changes ulcers above the ankle on medial aspect leads to stasis dermatitis with brownish pigmentation and stippling
Tx: ruduce swelling and prevent breakdown
- intermittent leg elevation
- compression stockings
- calf exercise
if chronic venous insufficiency transitions into stasis dermatitis, how do you treat it?
wet compresses
hydrocortisone cream
possibly zinc if chronic
aortic aneurysm
what is the problem with this condition? what is the pathophys? what are three things that can cause it? what are the four symptoms you see? what are the two diagnostics you wanna do, which is the one of choice?
dilation of a segment of blood vessel, thoracic or abdominal
most are asymptomatic until they rupture which is the issue, so goal is to identify them before they get to this point
weakness in vessel wall and subsequent dilation of vessel caused by genetics, atherosclerosis, medial cystic necrosis or damnage to intima
suddent onset, “ripping or tearing” abdominal, flank (abdominal), or back pain (thoracic), hypotension, shock, pulsatile mass
DX:
- abdominal US **study of choice**
2. CT angiography or MRA (magnetic resonance angiography) prior to intervention OR for thoracic
who is important to screen for aortic aneurysm? 3
- male
- smoker
- >6o years old with PAD and family history of AAA
explain the risk of rupture for aortic aneurysm based on the size and what are the tx reccomendations at each stage?
- watch it and monitor it
- >5cm: 20-40% over 5 years rupture, surgical to remove ELECTIVE SURGERY ADVISED!!
- >6cm: 15% risk it will rupture annually, ALWAYS SURGERY, REMOVE IT!!!!
Tx:
- open surgical repair (open with graft placement)
- endovascular (no surgical candidates, stents placed to reduce risk of rupture
prognosis of aortic aneursym is related to what two things?
- size of aneurysm
- CAD
what is the mortality rate of ruptured aortic aneurysm?
90%!!!!!
thats why its important to try to monitor it and find it early!!!!
aortic regurgitation
is this more common in m/f? what are four things that can cause this? what is the pathophys about what happens in this? what is important to note about the symptom onset??
75% in males
failure of the aortic valve to close all the way causing backflow into left ventricle
- rheumatic heart disease
- endocarditis on different valve
- bicuspid valve
- connective tissue disease
increase LVEDV, causing LV dilation leading to LV dysfunction with decrease EF and backs up to the lungs
- blood still flowing from the RA
- blood backing up from the aorta
*****LV failure often preceeds symptoms by 10-15 years so you MUST do serial echo/dopple to analyze to catch it before it is too late*****
aortic regurgitation
what are 5 interesting presentations that can occur at the arteries/pulses with aortic regurg?
- Water hammer pulse: rapid rising and collapsing of the pulse, bounds against finger
2. Quinke’s pulse: alternating flushing and paling at the skin at the root of the nail
3. pistole pulse over femoral artery
4. Derosiez’s sign to and from murmer over femoral artery
5. arterial pulse pressure widening: larger systolic and smaller diastolic so the difference is larger
aortic regurge
where do you hear it? what does it sound like? what can you feel? what happens with the apex?
- apex displaces laterally/inferiorlly
- diastolic thrill along left sternal border
- S3 with “blowing” diastolic decresendo murmer
- best heard with pt leaning foward 2-3rd LICS
what are the 3 test you use to dx a aortic regurg?
- EKG: LVH over time
2. echo: LV dysfunction later on, can see the aortic regurg jet detectable and semi quantifiable best!
- cath: tells regurg amount, LV dysfunction, intracardiac pressure (not usually need in young pt)
what are the 3 treatment options for aortic regurg?
- vasodilators: ACE/hyrdralizazide to decrease afterload
2. diruertics: decrease preload
3. Surgery with tissue or mechanical valve replacement
what is the most common cause of HF?
- *coronary heart disease**
- *aka MI/ischemia accounts for 75% of all HF cases!!!**