ENDO Portion Flashcards
what is the most common cause of hyperthryoidism?
GRAVES DISEASE!!!
hyperthyroidism:
Graves disease
what is important to knwo about this?
who is it common in?
what causes this?
3 things it leads to?
MOST COMMON CAUSE OF HYPERTHYROIDISM
women more common 20-40 years old!!
autoimmune TSH-R AB-IgG antibodies aka TSI directed to TSH receptor over-activate gland leading to hypersecretion
leads to: hypertrophy, hyperplasia, commonly goiter!!

hyperthyroidism:
graves disease
13 sxs
2 3 key ones you need to remember
- hyperactivity, irritability, restlessness
2. heat intolerance, sweating
- palpatations
- increased appetite, weight loss
- tachycardia
- arrythmia
- fine tremor
8. goiter
- warm, oily hair
- proximal muscle weakness
- opthalmopathy
-proptosis/exopthamos
-lid lag
-
dermopathy
- pretibial myxedema - hyperreflexes

hyperthyroidism:
Graves disease
OPTHALMOPATHY
3 things causes?
why?
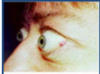
unique to graves disease

- proptosis/exopthalmos “lid lag”
- conjunctival inflammation/edema
- corneal drying
******occurs because the lympocytes infiltrate the orbit, muscles, eyelids and may cause diplopria and compression of optic nerve*****
hyperthyroidism:
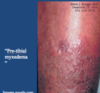
Graves Disease
DERMOPATHY
what is the name for this?
what does this cause?
apperance?
3% occurance
“pre-tibial myxedema”
*******noninflammatory induration and plaque formation of the pre-tibial area leading to thickened skin, and orange skin appereance*****
hyperthyroidism:
Graves disease
2 tests to check
what don’t you need to check?
- very low TSH
since the T3 and T4 high, negative causes this to be low
2. total and T4 elevated
**don’t need to check TSH-R AB for dx**
hyperthyroidism:
Graves disease
9 tx options?
what is the toc?
who do you use each in?
- endocrinology consult essential
- propanolol for sxs
-
methimazole (thiourea) -MILD TO MOD 12-18 months!
- inhibits thyroid peroxidases and block organification of iodine to decrease hormone production
-monitor WHB, pruirits, and FT4
- propylithiouricil (PTU) (thiourea) if pregnant
- saturated iodine solution- severe
- iodinated contrast agens- severe or thyroid storm
- prevents conversion of T4 to T3 - glucocorticoids-severe
- prevents conversion -
radioative iodine-DEFINITIVE TX and TREATMENT OF CHOICE IN THE US!!
- destroys the overactive gland because concentrates here
- uses I-131 - thyroidectomy
no longer TOC but used in children or pregnancy or those that can’ be controlled with medication
hyperthyroidism:
Graves disease
what do you need to keep in mind about the toc for this? what is it? what might worsen?
radioactive iodine
used to destroy the gland because it concentrates here
permanent hypothyroidism often develops within 1 year and may need replacement tx FOR LIFE!!!!
***opthalmopathy may worsen esp in smokers with this tx***
hypothyroidism:
Hashimoto’s thyroiditis
what is important to remember about this?
what type of disease?
how does it show up?
2 things ath cause this
what to keep in mind?
MOST COMMON CAUSE OF HYPOTHYROIDISM
AUTOIMMUNE, with insidious onset
thyroperoxidase and thyroglobulin antibodies present in high titers
*****keep in mind, this can itially cause a hyperthyroidism from release of stored hormone, but the end result is hypothyroisim*****

hypothyroidism:
Hashimoto’s thyroiditis
5 early sxs
8 late sxs
early:
- cold intolerance
- dry hair, hair loss
- headaches
- mennorhagia
- thin, brittle nails
late:
- slow speech
2. hoarse voice
3. weight gain
3. goiter
4. alopecia
4. facial and eyelip puffiness
5. bradycardia
6. edema non pitting
7. myxedema
8. pleural/pericardial effusion

hyperthyroidism:
Graves disease
in txing it with thiourea drugs what percent will have reccurance?
(propylithiouricil or methimazole)
50%
reccurence are common if tx is only with thiourea, propylthiouracil or methimazole
what are 4 complications that can come from graves disease?
- CV
- ocular
- psychological complications
- post tx hypothyroidism common, but easily txed
thyroid storm
what is this?
3 labs?
4 sxs?
3 tx options?
rare, but life-threatening of extreme hyperthyroidism, can be fatal and need to be admitted and txed STAT
elevated T3 and T4
decreased TSH
high fever
tachycardia
sweating
delierum
tx:
- satruated iodine solution
- iodinated contrast agents
- glucocorticoids
what are the 5 causes of hypothyroidism?
- hasimotos thyroiditis
2. congenital hypothyroidism
- idiopathic
- iatrogenic
- drug induced- amiodarone
hypothyroidism:
congenital
what testing?
why is it key to identify?
screening of TSH in newborns should elimate disease
early detection is key to prevent cretinism** and **hypodevelopment

hypothyroidism:
hashimotos thyroiditis
myxedema
what can this lead to?
5 sxs?
abnormal interstitial fluid acculuation in skin giveing it a waxy/coarsened (non-pitting) appearence
can lead to mydxedema crisis EMERGENCY:
severe form of hypothyroidism
- bradycardia
- CNS depression (coma)
- respiratory depression
- hypotension
- hypothermia
hypothyroidism:
hashimotos thyroiditis
2 complications
4
1
-
Cardiovascular
- pericardial effusions
- cardiomyopathy
- accerlerated CHD
- HF - encephalopathy
coma/confusion
hypothyroidism:
Hashimotos thyroiditis
5 dx?
- High TSH
- low T3/T4
- increased triglycerides
- decreased HDL
- anti-thyroid antibodies
hypothyroidism:
hashimoto’s thyroiditis
what is the tx?
how is it dosed?
monitoring?
goal? time frame?
levothyroxine (synthetic T4)
a. start 50-100 ug/day and titrate to full dose over time, following TSH levels
b. recheck TSH levels every 2-3 months until normal
GOAL: clinically euthyroid state (normal)
**sxs improve slowly over months**
hypothyroidism:
iatrogenic (we caused it)
tx?
radioative iodine for initial hyperthyroidism that leads to gland destruction
thyroiditis:
suppurative
what is this caused by?
3 sxs?
1 dx?
1 tx?
caused by gram positive bacteria
STAPH AUREUS
1. tender thyroid
- fever
- pharyngitis
DX:
fine needle aspiration
Tx:
drainage
thyroiditis:
De quervains aka granulomatous
what is this?
when is it most common?
when does it occur?
explain the progression?
2 dx?
- tx?
MOST COMMON CAUSE OF PAINFUL THYROID GLAND
***peaks in the summer….weird****
MC POST VRAL INFECTION
thyrotoxicosis initially presents followed by hypothyroidism and euthyroid within 12 months
DX:
- markedly increase ESR
- very low anti-thyroid bodies
Tx:
TOC=aspirin!!!
bb
ionated constrast agent
thyroiditis:
drug induced amiodarone
what does the medication contain?
what percent get this?
3 progression steps?
contains 37% iodine by weight or 75 mg per tablet
causes thyroid dysregulation in 20% of patients
Progression:
- can cause rise in T4 during first month of tx
- causes cellular resitsance to T4
- hypothyroid picture ensues with elevated TSH
thyroiditis:
fibrous thryoiditis (riedel)
who is this in?
what hapens to the thyroid?
key description
what happens to RAI?
ab?
1 dx method
1 tx method?
rarest form of thyroiditis, 80% are in females
formation of dense fibous tissue in the thyroid
causes
hard “woody” asymmetric thyroid feeling
the fibrosis can spread outside of the thyroid
radioactive iodine is decreased in involved areas of the thyroid
antibodies may be present in 45%
DX:
BIOPSY
tx:
tomoxifan
hyperparathyroidism
what are 2 most common causes?
what is hypersecreted?
2 hallmark lab findings?
what are 5 things this can lead to?
- MC cause parathyroid adenoma
- parathyroid hyperplasia/enlargement
hypersecretion of PTH
HALLMARK:
1. elevated PTH
2. elevated serum total and ionized Ca
- increased excretion of Ca and PO4 by the kidney overwhlems the tubular Ca absorptive capacity leading to hypercalciURIA
- chronic bone reabsorption
- sever leads to
osteopenia
osteoporosis
pathologic fractures

hyperparathyroid:
how is this normally found?
pneumonic for sxs?
leads to what what 6 presentations?
often discovered as incidental lab finding
“moans, groans, stones, bones”
- skeletal: loss of cortical bone with bone pain and arthalgias
- nephrologic disorders:
- decreased sensitivity to ADH with polyuria and poly dipsea
- increased calcium stones from saturation
- nephrosclerosis
- renal failure
hyperparathyroidism:
5 lab findings
what is important to do?
- serum Ca over 10.5
- increased ionized calcium over 5.4
- PO4 low
- alk phos increase if presence of bone disease
- PTH assay via radioimmunoassay
**important to do a 24 hour urine to quantify***
hyperparathyroidism:
4 tx options
what are the indications for the last?
1
4
- normal saline to increase intravascular space
- furosemide facilitates Ca excretion
3 biphosphonate stop osteoclast bone resorption
- parathyroidectomy
symptomatic:
presence of bone or kidney disease
asymptomatic:
1. hypercalcemia with significant hypercalcuria
2. BD ovr 2 SD below normal
3. age less than 50
4. pregnancy
what is a complication from thyroidectomy used to tx hyperparathyroidism?
tx?
rapid drop of PTH levels and can lead to acute hypocalcemia post-op
RX: calcium supplements
until parathyroid resumes function
what are five complications of hyperparathyroidism?
- pathologic fractures, esp in women
- urinary stones, obstruction, UTIs
- if Ca rises rapidly-CNS changes, renal failure
- PUD and pancreatitis form high CA levels
hypoparathyroidism
what are the 3 causes?
MC?
hallmark
- MC_-post-thyroidectomy_ or removal of parathyroid adenoma
- rarely polyglandular autoimmune
- chronic magnesium deficiency which impairs PTH release
HALLMARK:
low ionized Ca
hypoparathyroidism
6 acute sxs
5 chronic sxs
acute:
muscle cramps
irritability
tetany
seizures
paresthesias of hands and feet
carpopedal spasm
chronic:
- personaity changes
- decrease cognitive function
- cataract
- dry brittle nails
- chevosteks sign-twitching of facial nerve with tapping
- trousseaus sign-blow up BP cuff around arm and hand will twitch
hypoparathyroidism tx:
1 acute
3 chronic
acute

IV CALCIUM GLUCONATE
do until tetant and other sxs resolve
chronic
1. oral calcium
2. active metabolite of vitamin D 1,25-dihyrdroxycholecalciferole AKA CALCITROL
3. magnesium supplement
**goal: maintain serum Ca in low normal range**
hypoparathyroidism
4 lab findings
1. low serum total and ionized Ca
- elevated PO4
- decreased PTH
- prolonged QT and arrythmias
PARATHYROID HORMONE
what is the overall effect?
2 ways it accomplishes this
INCREASES BLOOD CA LEVELS
1. STIMULATES RELEASE OF CA FROM BONE (RESORPTION)
2. STIMULATES VITAMIN D ACTIVATION BY KIDNEY TO INCREASE INTESTINAL CA ABSORPTION
calcitonin
what secretes this?
overall funciton?
3 ways it accomplishes this?
secreted by the thyroid c-cells
**decreases blood Ca levels**
1. inhibits intestinal Ca absorption
2. inhibits osteoclast and stimulates osteoblast activity
3. inhibits renal tubular reabsorption of Ca
osteoporosis
what is this?
what type of bone is lost more commonly?
percentages
MOST COMMON METABOLIC BONE DISEASE
comprimised bone strength leading to an increased risk for fracture
bone resorption occurs most commonly in the trabecular bone** **“spongy bone” than the corical bone
Net bone loss over 10 years:
trabecular 25-30% and MC!!
cortical 10-15%
bone density
describe the progression throughout life? 5
what do people suggest about the tx based on this progression?
- increases dramatically in puberty due to gonadal steroids
- peaks in early 20s
- bone loss beings before menses creases
- accelerated bone loss in the 1st 5-10 years post menopause
- slows after age 60
***this is why people think that you could theoretically prevent with estrogen, and might be helpful in subsets like hypogonadism or premature menopause** **but NOT as long term option due to adverse outcome risks****
what are 7 conditions that increase the risk someone will develop osteoporosis?
- sex hormone deficiency, esp post menopause
- excess glucocorticoids (cushings)
- hyperparathyroidism-increased PTH stimulates bone breakdown
- thyrotoxicosis-increased bone metbolism
- alcoholism
- anorexia
- vit d deficency
opsteopenia definition
BMD 1-2.5 SD below peak bone density
osteoporosis definition
BMD over 2.5 SD from normal
when classifying between osteopenia, osteoporosis, or just normal person, what do you NEED to keep in mind?
presence of fracture without S&S or trauma indicates severe osteoporosis regardless of what the SD is!!
do men get osteoporosis?
how many?
YEP!!
1 out of 5 dxed people are men
hip fracture is a significant predictor for mortality!!
what are 7 RF that increase your risk for osteoporosis?
- prior fractures
- FH of osteoporosis related fractures
- low body weight
- cigarette consumption
- excessive ETOH use
- chronic inflammation: RA
- patients at high risk for falls or frailty
osteoporosis

what are 4 sxs you may see with this?
what is usually the inital presentation?
1. many asymptomatic till fracture (often spontaneous)
- ******may see back pain, decrease in height, or kyphosis***
- dietary calcium, vit D deficiency
osteoporosis
4 texts for dx
1 TOC? interpretation
- DEXA is TOC!!!
includes spine, femur
T-score: SD away from young healthy adults
over 2.5=osteoporosis
over 2: osteopenia
- check calcium levers
- check vitamin D levels (25-hydroxy vit D)
- consider checking putuiary hormones when indicated
who do you screen for osteoporosis in?
- early menopause
- RF
FH
malnourished
alcoholism
renal failure
- 65+
can you reverse established osteoporosis?
no
can increase BD, decrease fractures, and hald or slow progression
osteoporosis
what are the 5 drug classes used to tx this? First DOC? how is it taken? key things to know?
1. bisphosphonates-DOC
ALENDRONATE: take 30 mins before AM meal with 8ox water and remain upright 30 minutes after
-increased risk of unusual fracture so not longer than 5 years
inhibits osteoclasts
dental care important-jaw issues
very long half-life, in bone 10 years
- SERMS
serum estrogen receptor agonist/antagonist
alternative to estrogen in postmenopausal woman with decreased risk of adverse effects since no BC risk
- calcitonin
- Vitamin D; calcium
always supp vit D, Ca only if it is low!
- PTH synthetic analog
***normally PTH stimulates osteoclasts BUT when given in synthetic form it increases osteoblast activity and new bone formation=paradox**
INCREASES BONE DENSITY MORE THAN ANY OTHER DRUG BUT IS NEW AND CAN LEAD TO BONE CANCERS SO NOT USED AS MUCH NOW
6.estrogen replacement
only used in patients with premature menopause or hypogonadism**…dose related issues and increased risk for BC, DVT, endometrial cancer etc and **short term use only
what are the percent prevalence of T1DM and T2DM?
T1DM=10%
T2DM=90%
what are 5 brief features you find in Type 1 diabetes?
insulin deficiency
hyperglycemia
dyslipidemia
metabolic wasting
ketoacidosis
what are 4 brief features of T2DM?
hypoinsulinemia
hyperglycemia
dyslipidemia
obestiy often
what is the clinical importance of the insulin structure?
contrains C peptide
this is present only on endogenous insulin so measuring this will tell you how much insulin the Beta cells are actually producing and how much of their function is lef
WE MEASURE THIS TO TELL US HOW WELL THE BETA CELLS ARE WORKING
what are 5 overall broad functions of insulin secretion?
- decrease blood glucose
- decrease blood fatty acid
- decrease blood amino acid
- increase protein syntheisi
- increase fuel storage