Oral Manifestations of Systemic Disease Flashcards
What are Gastrointestinal Diseases
what are example of them?
Inflammatory bowel diseases associated with oral findings
▪ Crohn disease
▪ Ulcerative colitis
▪ Pyostomatitis vegetans
▪ Celiac Disease
Crohn Disease
Regional Ileitis
What areas does affect?
What are the symptoms?
What areas does affect?
● Primarily affecting distal small intestine and proximal colon
What are the symptoms?
● Symptoms include abdominal cramping, pain, bloating, diarrhea, and nauseas (similar amongst the GI diseases)
● Patients often have weight loss and malnutrition
● 20% have abrupt onset of symptoms resembling acute appendicitis or bowel perforation
Crohn Disease
Regional Ileitis
When it is diagnosed?
Etiology?
Prevalence?
What are the oral implactions?
When it is diagnosed?
● Usually initially diagnosed in adolescents
Etiology?
● Etiology unknown‐ immunologically mediated?
o Theory of being too clean as a child and having a negative response as we grow older since we’re not used to normal bacteria
Prevalence?
● Prevalence increasing, reason unknown
What are the oral implactions?
●Oral lesions can be first sign of disease
Crohn Disease
Histopathology
● Superficial or deep ulceration with adjacent granulation tissue extending into deep submucosa or below
● A transmural granulomatous inflammation
o Sarcoid‐like, non‐caseating, poorly formed granulomas, in all tissue layers (50‐70% of cases) usually adjacent to blood
vessels or lymphatics
● Transmural inflammation with lymphoid aggregates throughout bowel wall
Crohn Disease
Oral Findings
- Recurrent oral ulcerations can mimic those seen with recurrent aphthous lesions
-
Diffuse or nodular swelling of the oral and perioral tissues
- Can look like epulis fissuratum
-
Deep linear granulomatous‐appearing ulcerations (often in the buccal vestibule area)
- Cobblestone mucosal appearance
- Polypoid tag‐like lesions on vestibular and retromolar mucosa
- Enlargement of lips caused by granulomatous inflammation: orofacial granulomatosis
Crohn Disease
Treatment
- Current strategies aim for deep and long‐lasting remission, with the goal of preventing complications, such as surgery, and blocking disease progression
- Immunosuppressant such as cyclosporine
- In more severe cases;
- *high dose corticosteroids and**
- chemotherapeutics to induce a remission
-
Nutritional supplements (iron, folate)
- Because they are unable to absorb nutrients
- If medical means do not keep patient under control► surgical removal of a portion or all of the intestine
- When intestinal symptoms are under control►oral ulcerations resolve
Which systemic disease manifests like this?

Crohn Disease
- Patients can also get angular cheilitis
- Above the Linear ulceration, can see a flap like structure which is the hyperplastic margin
Which systemic disease has this oral manifestation?

- we see the ulceration and hyperplastic tissue surrounding it.
Which systemic disease has this oral manifestation?

Crohn Disease
Nodular appearance of buccal mucosa
Which systemic disease has this oral manifestation?

Crohn Disease
we see more nodules
Which systemic disease has this oral manifestation?

Crohn Disease
Linear granulomatous ulcerations
But they are not the aphthous ulcerations but the more
linear type
Ulcerative Colitis
- What are the symptoms
- What type of Cancer risk it presents?
What are the symptoms
- A chronic inflammatory disease of the colon (mucosa and submucosa) presenting with diarrhea, rectal bleeding, abdominal pain, weight loss and fever
What type of Cancer risk it presents?
- Increased risk of colon cancer
Ulcerative Colitis
Oral Lesions
● In some cases, patients get recurrent oral ulcerations (can have aphthous‐like lesions)
● Papillary mucosal projections with deep linear ulcers and fissures
● Intraepithelial pustules of the mucosa (pyostomatitis vegetans)
Ulcerative Colitis
Management
● Use of anti‐inflammatory medications
o Sulfasalazine or Prednisone
● If medical means do not succeed► then removal of part or all of colon
How different is Ulcerative Collitis from Crohn Disease?
Unlike Crohn’s, lesions extend in a continuous fashion proximally from the rectum (no skip lesions) and histologically don’t have granulomas

What is the difference between Inflammatory Bowel
Disease IBD & Irritable
Bowel Syndrome IBS
● IBD
o Classified as a disease
o Can cause destructive inflammation and permanent harm to the intestines
o The disease can be seen during diagnostic imaging
o Increased risk for colon cancer
● IBS
o Classified as a syndrome, a group of symptoms
o Dose not cause inflammation; rarely requires hospitalization or surgery
o There is no sign of abnormality during an exam of the colon
▪ Usually because it’s only periodic
o No increased risk form colon cancer or IBD
Pseudomembranous
Ulcerative Colitis
Causes?
Bactrial Overgrowth in the pseduomemberane
(C.difficile Overgrowth)
Causes:
- Clindamycin prolonged use ~2 weeks can cause the C. difficile overgrowth.
- Always warn patients if you prescribe clindamycin about possible side effects and stop usage since do not want them to develop untreatable strains

Pyostomatitis
Vegetans
what is it?
Demographics?
Symptoms onset?
What is it?
- Thought to be an unusual presentation of inflammatory bowel disease, especially ulcerative colitis (sometimes with Crohn’s)\
Demographics
- In only a rare subset of patients
- Typically present before 30 years of age
Symptoms onset
- ~25% of cases seen in absence of GI symptoms
- May see oral symptoms before the GI symptoms
Pyostomatitis
Vegetans
Oral Symptoms
and
Most common sites in the mouth?
Oral Symptoms
● Recurrent oral ulcerations _concurrent with, or prior to GI symptoms_
● Oral mucosa is erythematous and thickened with multiple
cream/yellow‐colored pustulesandsuperficial erosions
● Linear “snail track” oral pustules
Most common sites in the mouth?
● Most common sites include buccal and labial mucosa, soft palate, and ventral tongue
Pyostomatitis
vegetans
Treatment
● Treatment is not well standardized, fairly rare disease and good double blind studies rare
● Can use topical corticosteroids
● Werchniak et al had good results with topical tacrolimus
● Sulfasalazine or Prednisone for GI lesions
● If GI symptoms are under control► oral lesions will resolve

Oral Manifestations of which systemic disease?

Pyostomatitis
Vegetans
Oral Manifestations of which systemic disease?

Pyostomatitis
vegetans
Oral Manifestations of which systemic disease?

Pyostomatitis
vegetans
Snail track
appearance
Celiac (Sprue) Disease
What is it?
Which gene is involved?
Symptoms?
What is it?
● Chronic disease (diffuse enteritis) of the small intestine which improves upon withdrawal of gluten proteins
Which gene is involved?
● >90% express HLA‐B8 histocompatibility antigen
Symptoms?
● Patients present with diarrhea, gas, weight loss, fatigue, impaired nutrient absorption, etc
Patients with Celiac (Sprue) Disease have risk of developing which cancer?
● 10‐15% risk of GI lymphoma
Celiac (Sprue) Disease
Oral Symptoms
● 10‐15% risk of GI lymphoma
● Oral symptoms include aphthous‐like ulceration of mucosa
● Patients can have enamel defects and pitting
Amyloidosis
What is it?
From what does it form?
Seen with what disease?
What is it?
-
Protein deposits in tissue
- Paucicellular eosinophilic deposits amorphous eosinophilic deposit
From what does it form?
- Form fibrillar β‐pleated sheets within the tissue
Seen with what disease?
- multiple myeloma
Amyloidosis
what are its Types and what they are associated with?
- ▪ Primary amyloidosis is associated with multiple myeloma
- Reactive systemic amyloidosis
- Hemodialysis associated amyloidosis kidney dysfunction
- Hereditary amyloidosis (Familial Mediterranean Fever), present with polyneuropathies, cardiac arrhythmias, renal failure, CHF
- Localized dermal amyloidosis
Primary amyloidosis is associated with which cancer?
multiple myeloma
Hemodialysis associated amyloidosis leads to ——
kidney dysfunction
Amyloidosis
Organ Limited
Clinically
- Rare in oral cavity
- Amyloid nodule, asymptomatic submucosal deposit
- Not associated with systemic symptoms
Primary or Muliple Myeloma associated Amyloidosis
Systemic
Demographics & Clinical presentations
- Older adults > 65yrs
- Male predilection
- Amyloid deposits lead to macroglossia, carpal tunnel syndrome, hepatomegaly, dry mouth
- Skin lesions: Waxy papules and plaques, smooth surface (eyelid area, retroauricular, neck, lips), orangy, red appearance
Secondary Amyloidosis
systemic
Etiology & Effects
- Due to chronic inflammatory process
- *(osteomyelitis, TB,** sarcoidosis)
- Affects liver, kidney, spleen, adrenals but not heart
- can affect multiple organs, heart is usually spared
Hemodialysis associated Amyloidosis
Etiology & Effects
o Accumulation of normal protein (beta‐2 microglobulin) in plasma
_o Deposits in bones and joint_s
o Carpal tunnel syndrome, cervical spine pain
o Tongue deposits can have macroglossia
Amyloidosis
Clinical Presentations
-
Deposition of an extracellular proteinaceous material‐often immunoglobulins
- all types have common feature of a β‐pleated sheet molecular configuration
-
Macroglossia
- can be massive and exhibit dental indentations (crenation) with yellowish peripheral nodules
- Gingiva: usually normal in color, but may be bluish, spongy and enlarged
- Xerostomia if deposits in salivary glands
- Mucosal petechiae can be seen
Oral manifestation of which Systemic Disease?

Amyloidosis
Nodular “waxy” depositions in skin
deposition on the eyelid
Which systemic disease has this oral manifestation?

Amyloidosis
orange, red, yellow tinge
Which systemic disease has this oral manifestation?

Amyloidosis
Macroglossis and crenation of tongue (indentation near the teeth area)
skin deposits on the comissure,
Which systemic disease has this oral manifestation?

Amyloidosis
macroglossia
Which systemic disease has this oral manifestation?

Amyloidosis
Submucosal amyloid deposit
Which systemic disease has this oral manifestation?

Amyloidosis
Amyloid deposition on the tongue is amyloid, you have papule and nodule like area, can see the crenation of the tooth
Which systemic disease has this oral manifestation?

Amyloidosis
Amyloid deposition with ulceration and petechiae
Which systemic disease has these oral manifestations?

Amyloidosis
▪ different color compared to normal tongue with amyloid
Amyloidosis
Mangement
- Medical work‐up to determine type of amyloidosis
- Treat underlying disease when possible
- No treatment available for most types
- Chemo drugs (Colchicine, Prednisone, Melphalan, Thalidomide, Cyclophosphamide) for multiple myeloma
- Serum electrophoresis – monoclonal gammopathy very complicated and time consuming treatment
- Renal transplant for dialysis‐associated type
- Death due to cardiac failure, arrhythmias or renal failure is not uncommon within a few year of dx
Diabetes Mellitus
Endocrine Disease
- a group of metabolic disorders with one common manifestation: hyperglycemia
- Basic problem is either a decreased production of insulin or tissue resistance to insulin
Diabetes Mellitus
Pathophysiology
▪ Insulin is hormone produced by beta cells of the pancreatic islets of Langerhans
▪ It is required for the uptake of glucose by body cells
▪ Insulin binds specific receptors which trigger the intracellular events necessary for glucose uptake
Diabetes Mellitus
Types
Type 1
Type 2
Diabetes Mellitus
Type I
Definition
Demographics
Symptoms
Etiology
Definition
insulin‐dependent diabetes mellitus (IDDM)
Demographics
5‐10% of cases
Juvenile onset (avg age 14)
Symptoms
- Severe absolute lack of insulin
- Hyperglycemia and ketoacidosis
- Blood glucose levels of 200‐400 mg/dl (70‐120 normal)
- Ketoacidosis from using protein and fat for energy instead of glucose body can’t use glucose
- Thin body habitus
Etiology
- Autoimmune disease
- Thought to be possible viral infection as trigger to Islet cell antibody destruction of beta cells
Diabetes Mellitus
Type II
Definition
Demographics
Symptoms
Etiology
Definition
- non‐insulin‐dependent diabetes mellitus (NIDDM)
Demographics
- About 90% of cases
- Onset in older, obese adults (80‐90%); ketoacidosis is rare
Symptoms
- _Patients produce some insuli_n, can typically be treated with oral medication
- “insulin resistance”‐ insulin levels appear WNL or elevated
Etiology
- Decreased number of insulin receptors or defective receptors
- Genetic abnormalities, multifactorial
- Growing percent of the US population as well as around the world
Diabetes Mellitus
Complications
▪ Decreased neutrophil chemotaxis ►do not fight off infections as well as
you should
▪ Peripheral vascular disease►microangiopathy
o Results in ischemia: kidney failure, gangrenous complications of lower limbs, retinal involvement leading to blindness
o Amputations, CVA or MI
o Ketoacidosis may lead to diabetic coma
Diabetes Mellitus
Oral Findings
Most often associated with Type I but may be seen with Type II
- Periodontal disease‐ more frequent occurrence, more rapid progression
- Poor healing post oral surgery/extractions
- Enlargement and erythema of the attached gingiva
-
Increased risk of infections
- Candidiasis
- Xerostomia‐ 1/3 of pts complain of dryness
- Diabetic Sialadenosis‐ both type I and type II
- Mucormycosis‐ in uncontrolled disease and the tissue becomes necrotic because it is not getting any blood supply
-
Dental Carieso Benign migratory glossitis
- Increased prevalence in type I
Diabetes Mellitus
TYPE I
Management
- Insulin injections
-
Insulin shock‐ if blood glucose falls below 40 mg/dl
- Treat with dextrose
Diabetes Mellitus
TYPE II
Management
- Dietary modification and weight loss
-
Oral hypoglycemic agents
- ex. tolbutamide, glyburide, metformin
- Drugs may cause a lichenoid drug reaction
Oral Manifestation of which systemic disease

Diabetes Mellitus
Gingivitis = puffy red papillae here between the
central and lateral incisors
Oral Manifestation of which systemic disease ?

Diabetes mellitus
Anterior papillae are very puffy and red and fill of pus
Posterior gingiva are very
hyperplastic
Oral Manifestation of which systemic disease ?

Hyperplastic gingiva
Oral Manifestation of which systemic disease ?

Diabetes Mellitus
Sialadenosis
Oral Manifestation of which systemic disease ?

Diabetes Mellitus
diabetic patient who
developed Mucormycosis
Notice it is causing necrosis in the palate
Which systemic disease has this oral manifestation?

Lichenoid mucositis looks like lichen
planus
-same reticular white pattern, but there are
areas of erosion and some ulceration as
well
-some diabetic medications can lead to this
Hyperthyroidism
what is its most common form?
Graves’ Disease is the most common form
o An autoimmune disease attacks thyroid (TSH receptor)
o Leads to elevated release of thyroxine
o Most often a diffuse thyroid enlargement (goiter)
Benign and malignant tumors of thyroid and pituitary gland can cause which systemic disease
hyperthyroidism
In Hyperthyroidism, what happens to
T4 (thyroxine) and TSH values
- Serum T4 (thyroxine) is elevated
and
- TSH is decreased
Hyperthyroidism
Demographics
▪ 5‐10X more common in females ‐ 2% of women
▪ 3rd ‐ 4th decade of life
Hyperthyroidism
What patients might complain of?
What are the symptoms?
What patients might complain of?
- nervousness
- heart palpitations
- heat intolerance
- muscle weakness
- emotionally labile
What are the symptoms?
- weight loss, excessive perspiration, tachycardia,
tremors, eyelid retraction and exophthalmos
- 20‐40% have ocular involvement
o Early in the disease‐ characteristic stare with eyelid retraction and lid lag
o Exophthalmos or proptosis
▪ Oral findings in children can include early eruption of teeth
Hyperthyroidism
Treatment
- Treatment includes:
- Surgery – complete or partial removal of thyroid gland
-
Medications
- Propylthiouracil and methimazole block normal use of iodine by thyroid gland
- Radioactive iodine 131I
- Treatment often results in hypothyroidism

Which systemic disease has this oral manifestation?

Hyperthyroidism
- enlargement of the neck
- characteristic stare
Hypothyroidism
What happens in Hypothyroidism?
What it is called in children & adults?
How it is diagnosed?
What happens in Hypothyroidism?
- Decreased levels of thyroid hormone
What it is called in children & adults?
- cretinism in children
- myxedema in adults
How it is diagnosed?
- Diagnosed by measuring T4 (free thyroxine) in serum
Hypothyroidism
Primary and secondary etiologies and T4,TSH profile?
▪ Primary Hypothyroidism
‐ due to abnormality in thyroid gland
o T4 low, TSH elevated
▪ Secondary Hypothyroidism (less common)
‐ pituitary gland doesn’t produce adequate
amounts of TSH
o T4 low, TSH low or borderline
Hashimoto’s thyroiditis or thyroid surgery are main causes in adults of which systemic disease?
Hypothyroidism
Hypothyroidism
Symptoms
Oral findings
Symptoms
- Symptoms include lethargy, dry skin, thinning hair, swelling (edema) of face and extremities, huskiness of voice, weakness and fatigue
- ▪ Infants have failure to thrive
Symptoms
o Thickened lips and macroglossia due to accumulation of glycosaminoglycans (GAGs)
o In children can see failure of tooth eruption even though teeth have normal development (enamel pitting can be seen)
Hypothyroidism
Treatment
▪ Treatment is thyroid hormone replacement
▪ Prognosis is generally good
▪ If children are not treated in a timely fashion ► permanent CNS damage can occur (mental retardation)

Which systemic disease has this oral manifestation?

hypothyroidism
woman who had
hypothyroidism, lips are thickened, thick creases in the face
Which systemic disease has this oral manifestation?

hypothyroidism,
in child, still has
deciduous teeth even though its an older child
Radiographically we see the teeth have not erupted in the oral cavity

Which systemic disease has this oral manifestation?

Hypothyroidism
Macroglossia and crenation (scalloping)
of the lateral tongue
Before and after tx of which systemic disease?

hypothyroidism
Hyperparathyroidism
Can be Primary or Secondary
- Reduced amounts of PTH
- Parathormone normally stimulates osteoclasts in bone and resorption in kidney, to bring serum levels of calcium back to normal with decreased parathyroid function, serum calcium levels drop → hypocalcemia
- Lab findings ‐ PTH ↓, calcium ↓, phosphate↑, and normal renal function
- Postive Chvostek’s sign ( sign of low Calcium)
Females 2 to 4 times more than males
Primary Hyperparathyroidism
Charcterstics
o Uncontrolled PTH production
o 80‐90% caused by parathyroid adenoma
o ~15% caused by hyperplasia
o ~ 2% caused by parathyroid carcinoma
Secondary Hyperthirydoism
Charcterstics
o PTH continuously produced in response to chronic low serum calcium (usually associated with chronic renal disease)
Hyperparathyroidism
Classic triad
of
bones, stones, and groans (& moans)
-
Bones – Changes in the bones:
- Subperiosteal resorption of distal phalanges (early in disease)
- Loss of lamina dura around roots (early in disease)
- Loss/blurring of trabecular density in bone with resultant “ground glass” appearance in radiographs
- Brown tumor
- Stones – renal calculi (especially with primary disease) due to elevated serum calcium basically kidney stones
- Groans – duodenal ulcers
- Moans – changes in mental status mild dementia
What are the manifestation of Brown tumor in Hyperparathyroidism
- uni‐ or multilocular Radiolucency (pelvis, ribs, mandible)
- seen with persistent disease
- histology of giant cell lesion (like CGCG)
What is the most severe bone manifestation in people with hyperparathyroidism
Steitis fibrosa cystica
Where we see central degeneration and fibrosis of longstanding brown tumors
Hyperparathyroidism
Bones Manfestiation
- Subperiosteal resorption of distal phalanges (early in disease)
- Loss of lamina dura around roots (early in disease)
- Loss/blurring of trabecular density in bone with resultant
- “ground glass” appearance in radiographs
- Brown tumor
- Steitis fibrosa cystica
Hyperparathyroidism
Treatment
It is typically surgical removal of a portion or all of the
parathyroid glands
Hypoparathyroidism
Etiology
▪ Can be due to inadvertent surgical removal when thyroid gland is excised or to autoimmine destruction.
▪ DiGeorge syndrome (anomaly) and endocrine‐candidiasis syndrome can show this.
What is a Chvostek’s sign?
- The Chvostek sign is a clinical finding associated with hypocalcemia, or low levels of calcium in the blood.
- This clinical sign refers to a twitch of the facial muscles that occurs when gently tapping an individual’s when the facial nerve below the zygomatic process
Hypoparathyroidism
in young children
- If develops in young children tooth development can be affected
- pitting enamel hypoplasia and failure of eruption
- Persistent oral candidiasis in a young patient may be a sign of the onset of endocrine‐candidiasis syndrome (check for other endocrine abnormalities)
An Oral Manifestaion of which systemic disease?

Hyperparathyroidism
in young children
Hyperparathyroidism
Management
- Oral vitamin D precursor
- vitamin D2 (or ergocalciferol)
- Dietary supplements of calcium
- Teriparatide (a portion of PTH) injections twice daily
Pseudohypoparathyroidism
Also known as?
What is it?
How it appears clinically
What is its lab findings?
Also known as?
Albright hereditary osteodystrophy
What is it?
▪ Normal parathyroid and PTH, but activation of target cells is dysfunctional
How it appears clinically?
▪ Clinically, patient appears to have hypoparathyroidism
o Based on elevated serum levels of PTH seen with hypocalcemia,hyperphosphatemia and normal renal function
Lab findings
PTH ↑, calcium ↓, phosphate ↑
Pseudohypoparathyroidism
Types
What causes it
Type of inheritance & mutation
Types
Two broad disorders multiple subtypes
Type I and Type II
What causes it
Abnormal biochemical pathways that result in lack of target cell activation despite normal levels of PTH
Type of inheritance
Can be autosomal dominant inheritance –
defective PTH receptor on the target cells
Pseudohypoparathyroidism
Management
- Vitamin D and calcium supplements
- Serum and urinary calcium are monitored
Pseudohypoparathyroidism
Oral Findings
- *- Generalized enamel hypoplasia**
- Widened pulp chambers with pulpal calcifications (“dagger” shaped pulp stones)
- Oligodontia
- Delayed eruption
- Blunting of root apices
Which systemic disease has this oral manifestation?

Pseudohypoparathyroidism
pulp chambers are very
elongated
Which systemic disease has this oral manifestation?

Pseudohypoparathyroidism
issues with eruption, no
pulp stones present
Hereditary
Hypophosphatemia
Also known as?
What type of inheritance?
What mutation causes it?
Also known as?
vitamin D‐resistant rickets looks like they have rickets.
What type of inheritance?
▪ Most cases are X‐linked inheritance (males)
What mutation causes it?
o Mutation in PHEX ‐ zinc metalloproteinase gene
▪ phosphate regulating gene with endopeptidase activity on
the X chromosome
▪ Mutation affects metabolism of vitamin D precursors to the active metabolite
o Therefore low or no absorption of calcium
▪ Decreased capacity for reabsorption of phosphate from the renal tubules
Hereditary
Hypophosphatemia/vitamin D‐resistant rickets
Clincal Findings
Lab findings
Clinical Findings
▪ Clinical features similar to those of rickets, but resistant to treatment with vitamin D
o Short stature (upper body fairly normal, lower body shortened)
o Lower limbs short and bowed
▪ Similar to Vitamin D‐dependent rickets except no hypocalcification of teeth
▪ Teeth have enlarged pulp chambers and elongated pulp horns (extend to DEJ)
▪ With minor attrition of occlusal cusps, pulp is exposed to the oral cavity
▪ Exposures are often very small and when note periapical radiolucencies, it appears that otherwise normal teeth have periapical pathology
Lab findings:
↓ serum phosphate
What systemic disease causes this oral symptoms?

Hereditary
Hypophosphatemia/vitamin D‐resistant rickets
teeth look fairly
normal, have a draining abscess with ulcers and perilous
What systemic disease causes this oral symptoms?

Hereditary
Hypophosphatemia/vitamin D‐resistant rickets
teeth look fairly
normal, have a draining abscess with ulcers and perilous
Hereditary
Hypophosphatemia
Histology
Enlarged pulp horns
o Can extend up to DEJ
Abnormal globular dentin
o Dentin may exhibit clefting
Enamel clefts
Bacteria noted in enamel, dentin and pulp
o Pulpal involvement leads to necrosis and development of the periapical pathology

Hypophosphatasia
What is it?
Type of inheritance?
Clincal findings?
Lab Findings?
What is it?
Rare metabolic bone disease
Type of inheritance:
Autosomal recessive inheritance, generally the younger the age of
onset the more severe the expression
Clincal findings:
Bone abnormalities resemble rickets
Often presents with premature loss of primary teeth
o not from periodontal disease, thought that marked reduction, or lack, of cementum allows exfoliation
Lab findings:
↓ alkaline phosphatase, ↑ blood and urinary
phosphoethanolamine
Hypophosphatasia
Types
4
Perinatal
Infantile
Childhood
Adult
Hypophosphatasia
Perinatal
o Most severe manifestations
o Death in a few hours secondary to respiratory failure
o Marked hypocalcification of skeleton
Hypophosphatasia
Infantile
o Diagnosed ~4‐6 months due to failure to grow
o Skeletal malformations
shortened bowed limbs, rib and skull abnormalities
o Nephrocalcinosis, nephrolithiasis
Can have premature exfoliation of teeth
Hypophosphatasia
Childhood
o Diagnosed at later age, variable clinical expression
o Early sign is premature loss of primary teeth, may be the only teeth affected
o Large pulp chambers and alveolar bone loss
o Premature fusion of cranial fontanels can lead to increase
intracranial pressure and brain damage
Hypophosphatasia
Adult
o Mild presentation
o Premature loss of primary or permanent dentition; patient may be edentulous
o Stress fractures in feet
o Increased number of fractures assoc. with minor trauma
Acromegaly
vs
Gigantism
Acromegaly – excess production of growth hormone after closure of the epiphyseal plates
Gigantism – excess production of growth hormone before
closure of the epiphyseal plates
Acromegaly
Etiology
Clinical signs
Oral Findings
Etiology
▪ Usually due to a pituitary adenoma
Clinical signs
▪ Renewed growth of small bones of the hands and feet as well as membranous bones of the skull and jaws
▪ Soft tissues are also affected
Oral Findings
▪ Mandibular prognathism, macroglossia, and diastema formation
Which systemic disease has these clinical manifestations?

Acromegaly
Addison’s Disease
also known as
etiology
when do clinical symptoms appear?
also known as
Hypoadrenocorticism
etiology
Insufficient production of corticosteroid hormones due to destruction of adrenal cortex (autoimmune, infection, tumors, etc.)
when do clinical symptoms appear?
▪ Need ~90% destruction of gland before clinical symptoms
Addison’s Disease /Hypoadrenocorticism
Clincal symptoms
Lab findings
Clincal symptoms
- diffuse hyperpigmentation of skin (bronzing), fatigue,
- irritability, depression, weakness, etc.
- Oral mucosa shows diffuse or patchy macular pigmentations flattened pigmentations
Lab findings
failure of cortisol to rise in response to a rapid ACTH stimulation
Which systemic disease manfiest like this?

Addison’s Disease
Which systemic disease manfiest like this?

Addison’s Disease
Vitamin B3 (Niacin)
Deficiency known as
Classid Triad
Oral symptoms
Deficiency
pellagra
Classic triad
Dermatitis, Dementia, Diarrhea
Oral symptoms
stomatitis and glossitis
Which systemic disease is associated with this symptom?

Pellagra
Deficience in Vitamine B3 (Niacin)

Pellagra
Deficience in Vitamine B3 (Niacin)
Dermititis of the skin
Which systemic disease manifests like this?

Pellagra
Deficience in Vitamine B3 (Niacin)
erythema of the tongue
Vitamin C
Deficiency
Known as
scurvy
Iron Deficiency
Anemia
Charcterstics of the Anemia
Symptoms
Charctersics of Anemia
a hypochromic, microcytic anemia
decrease in color, smaller
than normal
Symptoms
fatigue, light headedness, lack of energy
.
Iron Deficiency
Anemia
Oral Symptoms
- Angular cheilitis (corner of the mouth ulceration)
- Dysphagia (difficulty swallowing)
- Atrophic glossitis (bald tongue, loss of papilla) beefy colored tongue
- Glossodynia (burning tongue)
Iron Deficiency
Anemia
Treatment
Treated with iron supplements, extreme cases with blood infusions
Plummer‐Vinson
Syndrome
What is it ( assiosited with what difficiency)?
Demographics?
What is it ( assiosited with what difficiency)?
- Iron deficiency anemia with glossitis and esophageal strictures
- Similar signs and symptoms as iron deficiency
Demographics
- Mostly women 30‐50 years old
- Northern European heritage more common
Plummer‐Vinson
Syndrome
Why it is a concern?
Why it is a concern?
Premalignant process
o ↑ incidence of oral and esophageal SCCa

Plummer‐Vinson
Syndrome
Iron Deficiency
Anemia
Treatment
- Treated with iron supplements
- Need long term follow up for eval of SCCa
Which systemic diseaswe associated with these oral manifestations?

PLUMMER‐VINSON
SYNDROME
denuded tongue
and angular chelitis
Which systemic diseaswe associated with these oral manifestations?

PLUMMER‐VINSON
SYNDROME
Angular chelitis (top) hard to get rid of them
Atrophic Glossitis (bottom) red beefy tongue
How blood looks with
Top photo: in Iron Deficiency Anemia, Plummer‐Vinson Syndrome, small area that is pale in the center
Bottom photo : normal smear, center is not pale

Pernicious Anemia
Type of Anemia?
What difficiency?
Causes?
Type of Anemia?
Megaloblastic Anemia
What difficiency?
Vitamin B12 difficiency
Causes?
- Poor absorption of vitamin B12 (extrinsic factor, cobalamin)
- These patients lack intrinsic factor, usually due to autoimmune destruction of parietal cells
- Intrinsic factor produced by parietal cells in the stomach is needed for absorption of B12
Pernicious Anemia
Symptoms
- Have burning sensation of tongue, lips and buccal mucosa
- One of the things you need to rule out in patients with burning mouth syndrome
- 50‐60% of patients have tongue symptoms, see atrophy (papilla denuded) and erythema
Pernicious Anemia
Treatment
- monthly IM injections of cyanocobalamin
- cannot take B12 orally, you need injections
Smear blood of Pernicious Anemia vs normal blood smear
not biconcave

Pernicious Anemia
CLASSIC TRIAD
1 – Generalized weakness
2 – Painful tongue
3 – Numbness or tingling of the
extremities
Which systemic disease manifests like this?

Pernicious Anemia
glossitis, denuded papillae
This is a before and after of which systemic disease?

Pernicious Anemia
denuded tongue and then the papillae is back again after the treatment. You have to get injections for the rest of your life
UREMIC STOMATITIS
What is it?
What causes the oral lesions?
What is it?
- Uncommon complication of renal failure
- Patients have markedly elevated levels of urea in their blood stream
What causes the oral lesions?
- Cause of oral lesions is unclear, may be urease produced by normal flora degrades urea in saliva liberating free ammonia which damages mucosa
UREMIC STOMATITIS
Clinical Presentation
Most cases in patients with acute renal failure
▪ Abrupt onset of white plaques or crusts
o Bad taste and burning also possible
o May be painful
▪ Usually on the buccal mucosa, tongue and floor of mouth
o If localized to the tongue can mimic oral hairy leukoplakia
▪ May detect an odor of ammonia or urine on the patients breath
Which systemic disease has this oral manifestation?

Uremic Stomatitis
Uremic Stomatitis
Treatment
▪ Usually clears within a few days after renal dialysis has begun
▪ Mildly acidic mouth rinses seem to clear oral lesions (ex. diluted hydrogen peroxide)
▪ Palliative treatment for pain includes ice chips or a topical anesthetic
Before and after treatment of which systemic disease?

Uremic Stomatitis
Before and
After Tx with Dialysis
changes on ventral and lateral side
of the tongue, better outcome after dialysis
Reiter’s Syndrome
also known as?
Corrlate with which antigen?
Associated with what?
also known as?
Reactive arthritis
Corrlate with which antigen?
Correlation with HLA B27 (> 70%)
Associated with what?
Typically seen after patient has either a bacterial dysentery or an STD sometimes chlamydia
Reiter’s Syndrome (Reactive Arthritis)
Etiology
Demographic
Clinical Presentation
Etiology
- Thought to be due to an abnormal immune response to the infection
Demographic
- Almost exclusively seen in males in their twenties
Clinical Presentation
- Oral lesions (~ 20% of cases) include painless oral ulcerations, erosions/erythema of mucosa, as well as erosions of the tongue which can mimic geographic tongue (both clinically and histologically)
Which systemic disease has these oral manifestations?

Reiter’s Syndrome (Reactive arthritis)
This not actually a geogrpahic tongue!
Which systemic disease has these oral manifestations?

Reiter’s Syndrome (Reactive arthritis)
Top: erythema on the palate and
areas of ulceration
Bottom: classic look of geographic
tongue, but it is not geo tongue. They are symptoms of Reiter’s
Reiter’s Syndrome
Classic Triad
Reiter’s Syndrome
Classic Triad
▪ 1 – Polyarthritis (lasting more than one month)
▪ 2 – Conjunctivitis or uveitis
▪ 3 – Urethritis
Infective endocarditis
▪ Janeway lesions
o Seen on palms of hands and soles of feet (tiny micro emboli that are causing lesions on the hands and feet)
▪ Erythematous macule or petechiae
▪ Painless
▪ Septic micro emboli

Which systemic disease has these clinical manifestations

Infective Endocardiatios
Janeway lesions
These are Septic Emboli
Hyperparathyroidism
What is it?
What are its types?
What is it?
- Excess of circulating parathyroid hormone important in formation of osseous structures
- Increase bone remodeling but tips the balance of osteoblastic and osteoclastic activity in favor or osteoclastic resorption
- it’s a systemic endocrine disease
What are its types?
o Primary hyperparathyroidism Type 1
▪ Uncontrolled parathyroid hormone production by
parathyroid neoplasm (adenoma >> hyperplasia >
adenocarcinoma)
o Secondary hyperparathyroidism Type 2
▪ Continuous parathyroid hormone production in
response to chronic low serum calcium levels
▪ Renal osteodystrophy
Which systemic disease is this?

Hyperparathyroidism
Here we see we see
- a granular appearance of the max and mand bone everywhere, it is not localized.
- There is a loss of bone density and the loss of definition of cortical bone.
- Here we see a loss of definition of lamina dura as well because it is now granular, and is not as clear.
Which systemic disease shows radiographically like this ?

Hyperparathyroidism; this is the brown tumor which is sometimes well or ill defined, multi or unilocular radiolucency with granular septation.
If you have a patient that is younger than 15-20 years old that has a central giant cell granuloma ► you have to check that patient for hyperparathyroidism, because it could be a brown tumor.
Which systemic disease shows radiographically like this ?

This is another medical CT scan. You see the granular appearance of
the maxilla, skull, and well-defined multilocular radiolucency with
granulation. We call this a brown tumor because it is associated with
hyperparathyroidism.
( systemic endocrine diseases)
Which systemic disease shows radiographically like this ?

Hyperparathyroidism
On our intraoral radiographs, we see loss of definition of lamina dura because the bone now has a granular appearance which extends to the lamina dura.
The teeth are usually normal, but there is a loss of lamina
dura around the teeth. These teeth are not mobile.
Which systemic disease shows radiographically like this?

a medical CT scan of a patient with secondary hyperparathyroidism.
We see a lack of cortical bone – no normal cortical bone. Inside the skull
we have a granular appearance, with radiolucent and radiopaque dots, we call this a salt and pepper dots.
This is why we call this a salt and pepper appearance, there is no normal cortical bone.
( systemic endocrine diseases)
Hyperparathyroidism
Radiographic features
▪ Stones, bones, moans, and groans
▪ Radiolucent appearance (generalized osteopenia) What we see in the bones is one of the earliest radiographic features that we see = sudden erosions in the phalanges in the bones of the hands followed by mineralization of the skeleton including max and mand, skull base. As a
result, you have generalized osteopenia. 10% of these patients have brown tumors
▪ Brown tumors: Brown tumors are the same as central giant cell granulomas. When they are associated with hyperparathyroidism, we call them brown tumors.
▪ Punctate or nodular calcifications in the joints and kidneys =stones
▪ Entire calvaria has a granular appearance classically known as the “salt and pepper” skull as a result of the generalized osteopenia, we have this granular appearance in the skull
Hypoparathyroidism
Radiographic features
What is Hypoparathyroidism:
Insufficient secretion of PTH
o Damage or removal of the parathyroid glands during thyroid surgery
Principal radiographic change: calcification of the basal ganglia
Sometimes we have pseudohypoparathyroidism. This happens when we have a normal amount of PTH, but there is something wrong with the response of the target tissue. So, we have normal PTH but abnormal response to PTH.
dental enamel hypoplasia, external root
resorption, delayed eruption, or root dilaceration
Which systemic disease shows radiographically like this?

we have 2 Pas of patients
with pseudohypoparathyroidism.
- hypoplasia of enamel, tooth material
- hypoplastic tooth bud ( hypoplastic means arrested development)
- delayed eruption,
- external root resorption.
Hyperpituitarism
What is it?
What is its types
What is it?
- Hyperfunction of the anterior lobe of the pituitary gland caused by a benign functioning tumor of the anterior lobe
- it’s a systemic endocrine disease
What is its types ?
▪ Types based on age of onset
- Gigantism happens in children, generalized overgrowth of most long bones, hard and soft tissue. These patients are usually very tall. Proportion in these patients may be normal, but very large appearance.
- Acromegaly Increased hyperfunction in adult patients. In these patients, the epiphysis of the long bones already closed, you can see in the mand or max. One of the observable features is enlargement of the whole mandible/skull/sinuses/soft tissue. Patients usually present with “My hat is not fitting anymore, my denture is not fitting anymore”
Hyperpituitarism
Radiographic
Features
▪ General features
- Enlargement (ballooning) of the sella turcica
- Enlargement of the paranasal sinuses (especially the frontal sinus)
- Thickening of the outer table of the skull
▪ Jaws
- Enlargement of the jaws, most notably the mandible
- Class III skeletal as a result of the mandible enlargement with growth centering in the condylar head
▪ Teeth and associated structures
- Spacing of the teeth, enlargement of tongue, it could result in spacing of teeth in the anterior region
o Hypercementosis the forces are higher now
- so you may see Hypercementosis
- Hypercementosis is excessive deposition of non-neoplastic cementum over normal root cementum, which alters root morphology. This cementum may be either hypocellular or cellular in natur*
Which systemic disease shows radiographically like this?

Acromegaly (Hyperpituitarism)
- enlargement of the mandibular bone with a high degree of enlargement
- a class III appearance
- enlargement of sella tursica because of the pituitary gland enlargement
Hypopituitarism
What is it?
What is it called?
How it appears radiographically?
What is it?
Reduced secretion of pituitary hormones
it’s a systemic endocrine disease
What is it called?
Dwarfism
How it appears radiographically?
▪ Finding of the jaws
o Normal eruption of primary dentition but delayed exfoliation
o Small jaws -> crowding and malocclusion because there is not enough space for the teeth to erupt
Which systemic disease manifests radiographically like this?

Dwarfism
- hypopituitarism*
- We see* multiple dental anomalies: hypodontia, radicular fusion, fused roots of left lateral incisor and left canine and impacted permanent teeth.
- (from google)*
Osteoporosis
What is it?
Why it happens?
What the bone are like?
What is it?
▪ Generalized decrease in bone mass in which the histologic appearance of bone is normal, it is a metabolic bone diseases (MBD)
Why it happens?
- Aging process (postmenopausal women) bone mass usually increases until 30 years of age, and then there is a gradual decrease- about 8% loss in females and 3% loss in males
- Nutritional deficiencies
- Hormonal imbalance
- Inactivity
- Corticosteroid or heparin therapy
What the bone are like?
▪ More prone to fracture (distal radius, proximal femur, ribs, and vertebrae)
Which systemic disease shows radiographically like this?

Osteoporosis
- reduction in bone density,
- larger bone marrow spaces.
We need more tests to confirm osteoporosis besides dental radiographs.
Osteopetrosis
What is it?
How is the bone is like?
What are the effects on other structures?
What are the consquences?
What is it?
Defect in the differentiation and function of osteoclasts, (osteoclasts that are used to resorb bone in the bone modeling process. They are not functioning properly ►so we have an increase in bone density.) It is a metabolic bone diseases (MBD)
How is the bone like?
Bone is dense, fragile, and susceptible to fracture _and infection ►we now have a_n osseous structure but small bone marrow spaces
What are the effects on other structures?
It compromised vascular structures and cranial nerves
Osteopetrosis
What are the consquences?
- Compression of the cranial nerves as they pass through the narrowed skull foramina -> blindness, deafness, vestibular nerve dysfunction, and facial nerve paralysis.
- Compromises hematopoiesis Poor vascularity -> osteomyelitis
Which systemic disease shows radiographically like this?

medical CT scan with a patient with osteopetrosis- very dense. Not a
nice definition of the cortical bone. We see decreased in size of skull
foramina.
Which systemic disease shows radiographically like this?

pt with Osteopetrosis
we see
Hypovascular bones so they are more prone to osteomyelitis. This is a sign of sequestrum which is a sign of osteomyelitis.

pt with Osteopetrosis
- Generalized increase in bone density, increased trabeculation, loss of large bone marrow spaces.
- These patients are more prone to osteomyelitis because they are Hypovascular.
- We have to be careful in extractions because they don’t have the same vascularity as other healthy patients have.
- We see an onion skin appearance by the white arrow.
Rickets and
Osteomalacia
What are they
Differences
Effects on Bones
What happens?
They are metabolic bone diseases (MBD)
Inadequate serum and extracellular levels of calcium and phosphate, failure of normal activity of vitamin D.
There are different levels in the conversion from I,12- dihydroxy vitamin D that can have errors, not just
the consumption of vitamin D.
Differences
Rickets: disease affects the growing skeleton in infants and
children
Osteomalacia: disease affects the mature skeleton in adults
Effects on bones:
A softening and weakening of bones
In Rickets and
Osteomalacia, there is Failure of normal activity of vitamin D, what causes it?
o Lack of vitamin D in the diet
o Gastrointestinal malabsorption problems
o Lack of exposure to UV light
o Liver disease
o Kidney disease
o Defect in the intestinal target cell response
Clinical presentation
Ricket
vs
Osteomalacia
Rickets
o Growth retardation
o Short stature
o Bowing of long bones of the legs, waddling gait
o Radiograph manifestations in the teeth (especially <3 years of age) and jaws
Osteomalacia
o Weak fragile bone structure
o Diffuse skeletal pain
o Susceptible to fracture with minor injury
o Radiographic manifestations in the jaws are uncommon
o you may see hyperplasia or thinning of mineralization of teeth. You can see hyperplasia of enamel in patients.
Which systemic disease has this radiographic manifestation?
Ricket / Osteomalacia
hyperplasia or thinning of mineralization of teeth. We
can see hyperplasia of enamel in patients.
Renal
Osteodystrophy
What is it?
what can it lead to?
What is it?
Chronic renal failure produces bone changes by interfering with the hydroxylation of vitamin D in the kidneys -> hypocalcemia -> inhibit the normal calcification of bone and teeth (it is a metabolic bone disease)
what can it lead to?
(secondary hyperparathyroidism)
level of calcium is low leads to having hyperparathyroidism secondary to osteodystrophy
Which systemic disease manifest radiographically like this?

Renal
Osteodystrophy 1
Presentation is variable. Sometimes you see denser or granular
appearance of bone. You see increase here
but you sometimes will also see loss of definition of lamina dura, sometimes a sclerotic appearance
and trabeculation.
Which systemic disease manifest radiographically like this?

Renal
Osteodystrophy 2
sometimes you see:
- increase in bone density
- loss of definition of lamina
- dura and cortical bone
Hypophosphatasia
What is it?
What are the types?
What is it?
- Rare metabolic bone disease due to lack of tissue-nonspecific alkaline phosphatase
What are its types?
Four types: prenatal, infantile, childhood, adult
- The younger the age of onset, the more severe the
- manifestations
- It may have premature loss of these patients because loss of function of the lungs in these patients
Hypophosphatasia
Common factors?
Dental manfestations?
Common factors?
- Low levels of tissue-nonspecific alkaline phosphatase
- High blood and urinary phosphoethanolamine
- Rickets-like skeletal malformations
Dental manfestations?
- Premature shedding of primary incisors
- Enamel hypoplasia
- Enlarged pulp chambers and root canals
Which systemic disease manifests radiographically like this?

Hypophosphatasia
Which systemic disease manifests radiographically like this?

large root canal structures, large root chambers, premature loss of
teeth = hypophosphatasia.
Hypophosphatemia
What is it?
_Clinical Manifestations?
Dental Manifestations?_
What is it?
- A rare, heterogeneous group of inherited metabolic disorders characterized by decreased phosphate reabsorption in the distal renal tubules
Hypophosphatemia
Clinical Manifestations?
Dental Manifestations?
Clinical Manifestations
- Rickets-like skeletal malformations
Dental Manifestations
- Enlarged pulp chambers and root canals
- Periapical and periodontal abscesses of no obvious cause
- Enamel hypoplasia
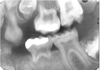
Which systemic disease manifests radiographically like this?

Hypophosphatemia
- Periapical lesions with radiolucency but no caries on the crown.
- There is loss of definition of cortical bone.
- On the teeth, you have:
- large pulp chambers
- hypoplasia of enamel and dentin
- periodontal and periapical lesions.
Progressive Systemic
Sclerosis
(scleroderma)
What is it?
Demographics?
What is it?
- Excessive collagen deposition resulting in hardening (sclerosis) of the skin and other tissues can have involvement of GI tract, heart, kidney,etc
Demographics?
- Middle aged female
Progressive Systemic
Sclerosis
(scleroderma)
Clinical symptoms
Oral Manifestations
Clinical Presentation
- Thickened, leathery quality skin
- joint pain
- exaggerated response to cold (Raynaud’s disease)
- heartburn.
- more prone for heart problems and respiratory
insufficiencies,
Oral Manifestations
- microstomia (small mouth)
- Xerostomia (dry mouth)
- telangietasia (“spider veins”)
- Increased decayed, missing and filled teeth.
- higher Gingivitis scores (usually)
- Deeper Periodontal Pockets
Progressive Systemic
Sclerosis
(scleroderma)
Treatment
Treatment for generalized symptoms may involve:
- corticosteroids
- immunosuppressants, such as methotrexate or Cytoxan
- nonsteroidal anti-inflammatory drugs
Depending on your symptoms, treatment can also include:
- blood pressure medication
- medication to aid breathing
- physical therapy
- light therapy, such as ultraviolet A1 phototherapy
- nitroglycerin ointment to treat localized areas of tightening of the skin
(from google)
Which systemic disease manifests radiographically like this?

Progressive Systemic
Sclerosis
(scleroderma)
sharp areas of resorption in the bones near muscles attached to the
angle of the mandible= masseter and medial pterygoid. You see
resorption at the coronoid process at the attachment of the temporal
bone as well.
Which Systemic disease manifests radiographically like this?

Progressive Systemic
Sclerosis
(scleroderma)
- presence of widening of the PDL space everywhere around the root of the tooth.
Sickle Cell Anemia
What is it?
What causes it?
What is it?
Chronic hemolytic blood disorder
What causes it?
▪ Abnormal hemoglobin, resulting in anemia -> by increasing the production of red blood cells -> requires compensatory hyperplasia of the bone marrow
Sickel Cell Aniema
Radiographics findings
- loss of this cortical bone area
- See the hair-on-end appearance on the skull
- enlargement of bone marrow spaces
- less trabeculation, more osteoporotic bone
- periapical pathology associated with teeth
with no obvious reason
Which systemic disease mainfest radiographically like this?

On a sickle cell anemia patient, you see:
- loss of this cortical bone area
- the hair-on-end appearance on the skull
Which systemic disease mainfest radiographically like this?

Sickel Cell Anemia
enlargement of bone marrow spaces, less trabeculation, more
osteoporotic bone. You see periapical pathology associated with teeth
with no obvious reason. You see the radioluscencies around the apex of
the mandibular teeth.
Thalassemia
What is it?
What causes it?
What is it?
- Defect in hemoglobin synthesis
What causes it?
- RBC with reduced hemoglobin content and short life span
Thalassemia
Clinical and Radiographic findings
- Hyperplasia of the bone marrow component of the bone which results in fewer trabeculae per unit area and can change the overall shape of the bone
- Protrusive premaxilla
- Radiographic appearance very similar to Sickle Cell Anemia
Which systemic disease mainfest radiographically like this?

Thalassemia
- osteopenic bone (loss bone mass and bones get weaker)
- radiolucent appearance of bone
- thinning of cortical bone around the mandible and maxilla.
- Usually there is hypoplasia of the paranasal sinuses.
Suspect systemic endocrine and metabolic disease if radiographs show what?
generalized decrease in bone density of jaws (thin cortices; granular cancellous bone; loss of lamina dura).
- Refer to physician for lab tests to make the diagnosis
We can include certain systemic endocrine and metabolic diseases as radiographic differentials in the presence of:
o Localized focus of radiolucency- think what?
o Mandibular prognathism and incisor flaring- think what?
o Premature shedding of primary incisors-think what?
o Enamel hypoplasia, enlarged pulp chambers and periapical abscesses of no obvious cause- think what?
o Localized focus of radiolucency► think brown tumor and
hyperparathyroidism
o Mandibular prognathism and incisor flaring► think acromegaly
o Premature shedding of primary incisors► think
hypophosphatasia
o Enamel hypoplasia, enlarged pulp chambers and periapical
abscesses of no obvious cause► think hypophosphatemia


