Infectious diseaes Kumar Flashcards
What is Human herpes virus (HHV)
what is it’s 8 types?
Large family of double stranded DNA viruses
❏ HHV‐1: HSV‐1‐Herpes simplex virus type 1 (most common in oral cavity)
❏ HHV‐2: HSV‐2‐Herpes simplex virus type 2
❏ HHV‐3: VZV‐Varicella zoster virus
❏ HHV‐4: EBV‐Epstein Barr virus
❏ HHV‐5: CMV‐Cytomegalovirus
❏ HHV‐6: Sixth disease/Roseola (commonly seen in children, spreads through saliva and respiratory droplets)
❏ HHV‐7: Roseola
❏ HHV‐8: KSHV‐Kaposi sarcoma‐associated herpesvirus
What is the Mode of infection of HHV?
Primary infection → Latency → Reactivationn → Recurrent infection
After the primary infection the HHV‐1/HSV1 stays in ————
Sensory ganglia
After the primary infection the HHV‐2/HSV2 stays in ————
Sensory ganglia
After the primary infection the HHV‐3/VZV stays in ————
Sensory ganglia (dorsal root ganglia)
After the primary infection the HHV‐4/EBV stays in ————
B‐Lymphocytes
After the primary infection the HHV‐5/CMV stays in ————
Myeloid cells, salivary gland cells, endothelium
After the primary infection the HHV‐6 stays in ————
CD4+ T‐Lymphocytes
After the primary infection the HHV‐7 stays in ————
CD4+ T‐Lymphocytes
After the primary infection the HHV‐8 stays in ————
- *B‐lymphocytes (latency)**, **endothelial cells (Kaposi
sarcoma) **
Herpes Simplex Virus
types
&
locations
❏ Type 1‐ adapted to oral, facial, and ocular areas (more common in
oral cavity)
❏ Type 2‐ adapted to genital area
❏ Other sites may also be affected
○ Herpetic whitlow (finger)
○ Herpes gladiatorum (wrestlers)
○ Herpes barbae (beard area)
Herpes Simplex Virus
primary infection
○ Acute/Primary Herpetic Gingivostomatitis
○ The easy way to remember where the ulcerations occur?
➢ gingiva and oral cavity
gingivo (=gingiva or fixed keratinized mucosa)
+
stoma (= the movable part of the oral cavity where the CT is
looser, including the labial and buccal mucosa, and the
tongue).
Herpes Simplex Virus
Recurrent infection
two manifestations:
- Herpes labialis: occurs on the vermillion border
-
Intra‐oral herpes: occurs ONLY on the fixed keratinized
mucosa (mucosa that doesn’t move around) MEMORIZE
THIS
What does it mean if a person has a primary infection?
They don’t have antibodies
Who’s the typical group that will get primary herpetic gingivostomatitis?
Children and young patients
What is this infectious disease?
Describe it

HSV‐1: Primary
Infection
it is a raised blister/papule on the
vermilion
The bottom arrow pointing to a mucosal
ulcer w/ tan pseudomembrane.
What is this infectious disease?
Describe it

HSV 1- Primary Herpetic
Gingivostomatitis
Ulcer with an erythematous halo (top two arrows). We
also have ulcerations that are irregular in shape on the gingiva
(bottom two arrows).
❏ Clinical Features:
- Cervical lymphadenopathy
- Chills
- Fever
- Nausea
- Anorexia
- Irritability
- Sores in mouth
- Ulcerations on fixed and movable mucosa
- Variable number of lesions
- Ulcers coalesce and form larger irregular ulcerations
- Gingiva enlarged and painful
- Resolution in 5‐7 days
What is this infectious diseease?
What is its pathogensis ?

HSV‐1: Primary
Infection
pathogensis
❏ Usually young age
❏ Often asymptomatic
❏ Symptomatic = Primary herpetic gingivostomatitis
❏ In adults is usually pharyngotonsillitis (back of throat)
❏ Spread through infected saliva or active lesions
❏ Incubation period = 3‐9 days
These photos represent
gingivostomatitis
multiple irregularly shaped
ulcers present on the fixed and movable mucosa, bilaterally
What is this infectious disease?
What probably this patient also have?

HSV1: primary herpetic gingivostomatitis
there are multiple irregularly shaped
ulcers present on the fixed and movable mucosa –> most likely
diagnosis is primary herpetic gingivostomatitis since the patient has
fever and malaise.
How is Primary HSV
(Herpes Simplex) diagnosed?
❏ Clinical diagnosis → based on putting all the features together
❏ Culture (may take 2 weeks) → not worth it
❏ Tissue biopsy → very invasive
❏ Cytologic smear (less invasive)
○ easiest bc you take a popsicle stick to scrape an ulceration
then you put those cells on a slide, you send it to a
pathologist after fixing the cells with some alcohol then you
can see the virally‐altered cells
❏ Serologic testing→ to look for antibodies 4‐8 days after they were
exposed.
HSV‐ Histopathology
❏ Molding
❏ Margination
❏ Multinucleation
❏ Also Tzanck cells

What is a
definitive diagnosis for HSV1 Herpes simplex
HSV‐ Cytology‐
Papanicolaou Stain
(PAP)

How to interpere HSV‐ Laboratory
Results based on IGg and IGm a
If you have positive IgM and negative IgG → that means it’s an acute
recent infection.
Then you have to wait 4‐6 weeks
If you do the serology then and get positive IgG and negative IgM → that means the person has the established infection.

What is the treatment of Primary Herpetic
Gingivostomatitis ?
- ❏ Supportive/Palliative Treatment
- ❏ Fluids, nutrition, rest, avoid spreading to others
- ❏ Avoid touching eyes, genitals
- ❏ Possible referral to MD if infant is not drinking because of pain
- ❏ Medications:
- Topical anesthetic (OTC vs Rx)
- Mucosal coating (OTC)
- Analgesic (OTC vs Rx)
- Antiviral (Rx)
What are the medications used to treat Primary HSV?
❏ OTC Magic Mouthwash Formulation: helps the person to actually be able to eat bc they have so many ulcerations
○ 1 Part‐ Diphenhydramine/ Benadryl (anticholinergic)
12.5mg/5mL elixir
○ 1 Part‐ Lidocaine (topical anesthetic)
○ 1 Part‐ Magnesium hydroxide/ Maalox (mucosal coating
agent)
○ Disp: 4 oz bottle
○ Label: Rinse with 5mL every 2 hours for 30 sec. then spit
out
❏ Rx‐Topical Anesthetic
○ Lidocaine 2% viscous solution* (viscous lidocaine)
○ Disp: 100mL bottle
○ Label: Rinse with 10 mL for 2 minutes and spit out
*May diminish the gag reflex therefore better suited for older
patients‐ shouldn’t be prescribed to kids. Remember serious sideeffects of seizures and methemoglobinemia in pediatric population.
❏ OTC Analgesic
○ Acetaminophen (Tylenol) OR ibuprofen (NSAID)
suspension/ tablets as directed for body weight
❏ Rx Antivirals
○ Generally only indicated for immunocompromised or
dehydrated patients
○ Limited evidence for other cases‐ see Cochrane Oral Health
Group Review* (*Amended recently)
○ Oral acyclovir suspension (Zovirax) is typically used
○ 15 mg/kg up to adult dose of 200mg
○ Rinse and swallow, 5 times a day for 5‐7 days
HSV-1 RECURRENT INFECTION
- §Secondary herpes
- §Mild, self-limiting
- §Vermilion border
- §Intraorally on fixed keratinized mucosa
- §7-10 days
- §Unilateral
- § Prevalence‐15‐45%
- 90% of adults have the antibodies, but 15‐45% of them can get recurrent herpes. Most of us have the antibodies, but we never exhibited the primary infection or a recurrent infection*.
- § 1‐6 outbreaks a year
Reccurent HSV-1 Latency place is ——–
trigeminal ganglion
What are the Stages of recurrent Hsv-1?
Prodrome►papules►vesicles►ulcer►crust►heals►no scar
What is this infectious disease?
describe it

recurrent Hsv-1/Recurrent herpes
It is raised
(papule), so it’s in the middle stage
What are some of triggers of the Recurrent HSV?
- Old age, Allergy
- UV light ,Trauma
- Physical / emotional stress, Dental treatment
- Fatigue, Respiratory illnesses
- Heat, Fever
- Cold, Menstruation
- Pregnancy, Systemic Diseases
- Malignancy
What is HSV‐ Recurrent Infection‐
Shedding ?
Asymptomatic shedding can occur in seropositive patients
❏ More common after surgical procedures and in
immunocompromised patients
❏ We need to take Universal precautions
What is this infectious disease?
describe it

Recurrent HSV-1
papule bc its
raised
What is this infectious disease?
describe it

Recurrent HSV-1
crust → later
crust comes off and then
you’ll have
epithelialization
underneath
What is this infectious disease?
describe it

Recurrent HSV-1
Vesicle stage (unilateral)
What is this infectious disease?
describe it

Recurrent HSV-1
Bilateral > THIS IS KEY
-differential diagnosis with a Staph infection
that occurs periorally with kids -> impetigo
What is this infectious disease?
describe it

Recurrent HSV-1
This is recurrent intraoral herpes. We have
punctate (point‐like) ulcerations which sometimes have clusters of
coalescing ulcers. That’s the words you wanna use
Other features of the ulcers:
○ Erythematous border
○ Irregular shape
○ Fixed mucosa
○ Unilateral
What is this infectious disease?
describe it

Recurrent HSV-1
Punctuate ulceration
erythematous border, irregular shape, fixed mucosa, unilateral
What is this infectious disease?
describe it

Recurrent HSV-1
healing stage cause
you might see this one day
How to diagnose Recurrent HSV?
❏ Clinical‐ if you see punctate ulcers unilaterally on the palate, it is
usually recurrent herpes simplex.
❏ Culture (may take 2 weeks) ‐ takes too long
❏ Tissue biopsy‐ if it wasn’t typical
❏ Cytologic smear‐ the ideal way if you want a definitive diagnosis
What is the Treatment Recurrent HSV-1?
❏ Depends on severity/frequency
❏ Preventive/suppressive vs episodic/abortive strategies
Two types of treatment:
Preventive/Suppressive: taking antivirals everyday to prevent an outbreak
Episodic: taking antivirals here and there to abort the process; episodic: abortive.
❏ Drugs used:
❏ Antiviral agents
❏ Antiviral‐steroid combination agents
❏ Avoid precipitating factors, like use sunscreens – avoid any triggers
e At which stage should the
abortive/ episodic treatment be done to avoid the outbreak?
❏ the prodrome, prodrome treatment is abortive
**remember this!**
RECURRENT HERPES LABIALIS-RX TOPICAL/SYSTEMIC AGENTS
Topical like Acyclovir
or Acylovir + steroid combination
There are many OTC topical medications
suppressive or preventative therapy of Recurrent HSV-1
: taking antivirals everyday to prevent those 6 outbreak/year.
There is modest evidence
that systemic acyclovir or
valacyclovir prevents
recurrent herpes labialis
these drugs tend to only affect virally‐altered cells. They don’t
affect the mammalian cells; they’re very safe.
Episodic/ Abortive
therapy of reccurent HSV1
❏ Episodic‐Occurring, appearing, or changing at usually irregular
intervals
❏ Abortive‐Tending to cut short the course of a disease
○ Medication has to be taken during Prodrome
○ When the patient feels a burning, itching, and tingling
What are Recurrent Herpes
Labialis‐ FDA Approved
Topical Treatments?
❏ Rx: Acyclovir cream 5% (Zovirax)
Disp: 5g tube
Label: dab on lesion every 2 hours for 4 days
❏ Rx: Penciclovir cream 1% (Denavir)
Disp: 5g tube
Label: dab on lesion every 2 hours for 4 days
❏ Rx: Docosanal cream (Abreva) OTC
Disp: 2g tube
Label: dab on lesion five times per day for 4 days
Acyclovir and Penciclovir
should be taken during
the prodrome stage
❏ Rx: Acyclovir 5%/ hydrocortisone 1% cream (Xerese)
Disp: 5g tube
Label: dab on lesion 5 times a day for 5 days
❏ Rx: Acyclovir buccal tablets (Sitavig) 50mg
Disp: 2 dose pack
Label: apply to canine fossa within 1 hour of symptoms
(single dose)
What are Recurrent Herpes
Labialis‐ FDA Approved
Systemic Antivirals ?
❏ Rx: Valacyclovir 1g tablets
Disp: 4 tabs
Label: 2 tabs stat PO, then again in 12 hours (ie 2 doses)
Given during prodrome.
❏ Rx: Famciclovir 500mg tablets
Disp: 3 tabs
Label: 3 tabs stat PO
What are other Topical
Agents for treating Recurrent Herpes
Labialis?
❏ Ice
❏ L‐lysine
❏ Bioflavonoids
❏ Evaporants ‐ Desiccants
❏ Emollients
❏ Bioadhesives (Zilactin‐benzyl alcohol, topical pain reliever)
❏ Wound‐healing modification/ occlusive agents
What is this infectious disease?

Atypical recurrent HSV
❏ Immunocompromised host
Atypical recurrent HSV can have this
appearance on the movable mucosa too, not just fixed
What is this infectious disease?

HSV Associated
Erythema
Multiforme
❏ Skin immune reaction in response to infection
❏HSV implicated in trigger for erythema
multiforme where you get target lesions
and crusted ulcerations on the
lip
❏ need to prescribe :antiviral prophylaxis
HHV3
What is it’s primary infection and Secondary infection known as?
❏ Primary infection
○ Varicella/ Chicken pox
❏ Secondary infection
○ Zoster/ Shingles
○ May affect oral cavity/ face if reactivation
along distribution of V1/2/3
What is this infectious disease?
describe it

HHV3
Varicella (chickenpox)
It is caused by
Varicella Zoster
Virus Infection
a typical macular, papular, vesicular rash –
it’s bilateral
What is this infectious disease?

Herpes Zoster/
Shingles
- It is affecting the intraoral region
- and the maxillary branch.
- Picture on the far right looks like recurrent HSV (cluster of coalescing ulcers)
- Looking at the picture on the left you can determine it is NOT a recurrent intraoral herpes because we have vesicles that opened up and crusted over on the skin.
VZV histopathology is the same as HSV.
VZV remains latent in the
dorsal root ganglion
travels down the sensory nerves to skin upon reactivation.
❏ The reactivation presents as a painful rash in one or two adjacent
dermatomes that does not cross the midline.
❏ The rash is maculopapular and develops into vesicles.
❏ One complication of zoster is post‐herpetic neuralgia: pain that
persists in the area where the rash once was present.
HHV‐4
Latency?
and
What are the EBV inducded diseases?
Epstein‐Barr Virus
Infection
Latency in lymphocytes
§Infectious mononucleosis
§Oral hairy leukoplakia
§Nasopharyngeal carcinoma
§EBV mucocutaneous ulceration
§Burkitt lymphoma
§Other lymphomas (Hodgkin, post transplant)
What is this infectious disease?

Infectious mononucleosis
Epstein‐Barr Virus/EBV‐induced disease
The virus spreads through saliva, which is why it’s sometimes called “kissing disease.” Mono occurs most often in teens and young adults. However, you can get it at any age. Symptoms of mono include:
Fever
Sore throat
Swollen lymph glands
- when you have salivary transfer, your lymph nodes get swollen
- people feel fatigue and fever
- they have tonsilitis
- can lead to the secretion of white or gray‐ green tonsillar exudate
- they can get petechiae on the palate too.
What is this disease?
Which virus causes it
describe it

Oral hairy leukoplakia
Epstein‐Barr Virus induced disease
❏ Corrugated white
keratotic lesion
on the lateral
tongue in HIV+ people
What is this diseases?
Which virus is asscoaited with it?

Nasopharyngeal carcinoma
❏ Associated w/ HHV‐4 (EBV)
❏ You might be one of the first people to detect this
cancer – the first sign is the swelling of the lymph
nodes
In this case, these are late stages of the disease.
this photo from google
What is this infectious diasese?

EBV mucocutaneous ulceration
Very rare
Photos from google
Which disease has Stary sky pattern histopathology?

Burkitt
Lymphoma
caused by EBV
What is this diasese?
which viruse causes it

Burkitt
Lymphoma
Epstein‐Barr Virus
Infection
- Fast growing tumor discovered by Dr. Burkitt
- High grade lymphoma B cells‐ Usually affects the jaws of children.
- It is the fastest growing tumor/cancer.
- There is translocation of c‐myc
HHV5
is it symptomatics?
where does the diseases predominantly found?
Latency?
Cytomegalovirus
Infection
❏ Usually asymptomatic
❏ Symptomatic infections are nonspecific: chills, fever, sore throat
❏ What’s interesting here: ❏ When the cells are affected, they form these owl eyes – they are nuclear inclusions and cytoplasmic inclusions.
❏ Disease states found predominantly in:
- ○ pregnancy/neonates (congenital infection)
- immunocompromised patients, particularly transplant and HIV+ patients
❏ Latency in myeloid cells, salivary gland
cells and endothelium
What is this infectious disease?

HHV 5
Cytomegalovirus
Infection
Histopathology look like an owl eyes
means the cells are affected- they are nuclear inclusions and cytoplasmic inclusions.

What is this infectious disease?
Desercibe it

HHV 5
Cytomegalovirus
Infection
When a person is immunocompromised, particularly those who’ve had a transplant or HIV+ patients, only these people will present with ulcerations
It’s very hard to identify
based on photo alone
- it’s very nonspecific
HHV‐8
What is it?
Assoicated with what?
How it evolved?
How it is treated?
Kaposi sarcoma–associated herpesvirus (KSHV)
❏ Vascular neoplasm of endothelium
❏ Associated with immunosuppression
❏ Usually evolves through 3 stages:
○ Patch►plaque►nodular
- More commonly seen in patients with HIV infection.
- Treated with topical agents and chemotherapy.
What is this disease?
Describe it

Kaposi sarcoma
HHV 8
Kaposi sarcoma on
the skin:
>1cm
Different color, so
this is called a patch.
Erythematous
patches present on
multiple areas of the
face.
Kaposi sarcoma
Histopathology
Histopathology shows malignant endothelial cells proliferating.
There are tiny spaces. Extravasation of RBCs can be seen

What is this disease?

Kaposi Sarcoma
(HHV‐8)
Right photo: we see Patch, slightly raised plaque stage
○ This is different from hemangioma because if you press on it, it
doesn’t blanch (where all the blood goes away, and it looks
white)
Left photo: Nodular is when it becomes very exophytic
You need to do a biopsy for this because it looks irregular.

what are the charcterstics of
HUMAN PAPILLOMA VIRUS (HPV)
?
§Small, non-enveloped icosahedral DNA virus that infects
skin or mucosal cells of humans.
§Circular DNA
§198 types established
§High and low risk types
‐ HIGH risk = CANCER
‐ LOW risk = WARTS
What can HPV Epithelial Lesions
cause?
(3)
▪ Benign: neoplasms of squamous epithelium
▪ Pre‐malignant: epithelial dysplasia – can lead to cancer
▪ Malignant: squamous cell carcinoma – infiltration of epithelial cells
What are HPV types that cause
Non‐genital Benign Involving the Skin?
2 & 4

What are HPV types that cause
Non‐genital Benign Involving Mucosa?
6 & 11

What are HPV types that cause
Genital Benign Lesions?
6, 11, 16, 18
(condyloma – can be malignant)

What are HPV types that cause
Malignant & Potentially Malignant Disorders?
16, 18

What are Routes of Transmission for HPV?
▪ Sexual/non‐sexual direct contact
▪ Salivary transfer
▪ Contaminated objects (fomite) – not well established
▪ Autoinoculation – child puts finger into mouth
▪ Perinatal/pre‐natal transmission
What is HPV Pathogenesis and Incubation period?
Incubation period: 3 weeks – 2yrs
▪ Basic Explanation: Basal epithelial cell infection ► Genome
replicates ► DNA released into stratum corneum
▪ Detailed Explanation:
- HPV accesses and infects cells of the epithelial basal
layer through breaks in the skin or mucosa - The virus becomes incorporated in the genome of the
infected cell - The site of HPV integration into the cellular genome is
in the general region of known oncogenes - The virus replicates during keratinocyte
differentiation in the spinous and granular cell layers - A portion of the HPV genome encodes proteins that
are capable of inducing cell proliferation and
transformation (E6, E7)

HPV Pathogenesis – High Risk
▪ Break in the skin ► HPV (dark dots) invades and infects basal cells
▪ HPV incorporates into DNA ► moves up epithelium as it matures ► releases
Then 2 things happen
1.
or
2.

- Completely have infection go away
or
2 .Stays and forms wart or affects maturation (becomes cancer, depending on strain)

HPV Genome
Organization
▪ LCR: long control region
▪ P97: promoter protein
▪ E1‐E7: early region genes
▪ L1,L2: late region genes

What is the Molecular Mechanism
of HPV?
**E6 = degrades p53 E7 = inactivates pRb**
- E2 = attachment location of Integrated HPV
- transcription of E6 + E7
- Binding of the viral E7 protein to pRb ► release of E2F and other proteins ► signals for the cell cycle to progress
▪ As long as the E7 protein stays attached to pRb, uncontrolled cell proliferation will continue
HPV E6 protein is:
‐ A ubiquitin ligase
‐ contributes to oncogenesis by attaching ubiquitin molecules to p53 ► making
p53 inactive and subject to proteasomal degradation
▪ Normal function of p53 = to stop cell division + repair damaged DNA so that damaged cells do not reproduce (apoptosis)
▪ When p53 is inactive, cells with changes in the DNA, such as integrated viral DNA, are not repaired ► destabilizes the cell ► increases the risk of malignant transformation
What is Persistence of HPV
▪ Low‐risk types: clear faster, less likely to become persistent
▪ High‐risk types: clear slowly, more likely to become persistent
What is the Prevalence of Oral (HPV)
Overall: 6.9% (CI 6.7‐8.3)
▪ Gender: Men (10.1%) > Women (3.6%) – women clear faster
▪ Age: bimodal distribution – 30‐34yo and 60‐64yo (she says 30‐34 but Dr. Kerr’s
graph shows mid‐20s
▪ High Risk HPV (3.7%) > Low risk HPV (3.1%)
▪ HPV‐16 infection most prevalent (1% or 2.13 million Americans)
▪ Based on NHANES study w/ oral rinse sampling and PCR
What are Risk Factors Associated
w/ Prevalence of HPV?
▪ Ever had sex (7.6%) vs never had sex (0.9%)
▪ Male
▪ Increased number of sexual partners (vaginal or oral sex)
▪ Tobacco smoking
▪ HIV infection
Most prevelant HPV TYPE?
HPV 16 = most prevalent
What is the Prevalence in
HIV + ?
Ppl w/ HIV+ and low CD4 T‐cells lvl = higher risk of
HPV
HPV 16+ higher if CD4 <200
Compare between SCC in Squamous Cell Carcinoma caused by HPV vs Tobacco and Alcohol
▪ HPV associated SCCa
‐ Wild type TP53
‐ Low pRb
‐ Increased p16
▪ Tobacco and Alcohol associated SCCa
‐ *Mutated TP53 – mutated by carcinogens in tobacco and alcohol► cancer
‐ pRB overexpression
‐ Decrease p16
BENIGN ORAL LOW RISK HPV LESIONS
(WARTS)
How do they appear?
Color?
Size?
Histologic?
§Appear as single or multiple exophytic papules, either sessile and flat
or pedunculated and papillary.
§Color depends upon degree of keratinization, ranging from white to
pink.
§Size of papules generally <10mm in diameter.
§Histologically, lesions may have koilocytes.
What are the types of Benign Oral Low Risk HPV
Lesion ?
(5)
▪ Squamous papilloma
▪ Verruca vulgaris
▪ Condyloma acuminatum
▪ Focal epithelial hyperplasia
▪ Oral florid papillomatosis
SQUAMOUS PAPILLOMA
What is it?
Gender?
Age?
Location?
Apperance ?
Treatment?
▪ Benign proliferation of stratified squamous
epithelium resulting ► papillary, verruciform, rugose (ridged or wrinkled) mass
▪ HPV types 6 + 11 – Low risk
▪ M = F
▪ Any age (more common in 30‐50s)
▪ Any oral mucosal surface (palate most common)
▪ Soft, painless, usually pedunculated, exophytic lesion w/ numerous finger‐like projections
▪ HPV DNA detected in only ~50%
▪ **should remove from mouth – but WOULD NOT submit for HPV typing
What is this infectious diease?

SQUAMOUS PAPILLOMA
Benign Oral Low Risk HPV
Lesion
HPV 6+11
“finger‐like projections
What is this infectious diease?

SQUAMOUS PAPILLOMA
Benign Oral Low Risk HPV
Lesion
HPV 6+11
“finger‐like projections
- The projections are almost feathery
- exophytic lesion
Oral Verruca Vulgaris
What is it?
Contagious?
Age?
Location?
Apperance ?
▪ HPV 2, and others (1,4,6,7,11,26,27,29,41,57,65,75‐77)
▪ Benign, HPV‐induced focal hyperplasia of stratified squamous epithelium
▪ Contagious – transmitted by direct contact
▪ Any age – frequently seen in children
▪ More common Anterior > Posterior part of mouth
▪ Soft, painless, usually pedunculated, exophytic lesions w/ numerous fingerlike projections (similar to squamous papilloma)
‐ How to tell the difference? Under microscope
What is this infectious disease?

Oral Verruca Vulgaris
HPV 2,4,6
Also “finger‐like
projections”
remember it’s contagious
Condyloma Acuminatum
(Venereal Wart)
What is it?
Contagious?
Transmission?
Age?
Location?
Apperance ?
HPV Types 6, 11 – condyloma can turn cancerous
▪ Virually induced proliferation of stratified squamous epithelium – usually genital or anal mucosa
▪ Contagious – transmitted by direct contact
▪ Incubation period: 1‐3mo
▪ Considered sexually transmitted disease (if corroborated by history)
▪ Oral lesions – usually anterior part of mouth
▪ Sessile, pink, well‐demarcated, non‐tender exophytic mass
▪ Short, blunted surface projections
▪ Larger than papilloma or verruca vulgar
▪ Characteristic clustering of multiple lesions
What is this infectious disease?

Condyloma Acuminatum
(Venereal Wart)
HPV 6,11 – can be
cancerous
Genital warts
“short, blunt, clusters”
Characteristic clustering of multiple lesions

If you see Condyloma Acuminatum in a child, what is the next step?
-Since this is a sexually transmitted disease, we need to suspect sexcual child abuse and investigate further!
(Multifocal) Epithelial
Hyperplasia/Heck’s
Disease
What is it?
Appearance?
Which communities or environment?
Demographics age and gender?
Histology?
▪ HPV Types 13, 32 and others (1,6,11,16,18,55)
▪ HPV‐induced localized proliferation of oral squamous epithelium
▪ “Flat‐top papules”
▪ Endemic in some Inuit/Alaskan native + Native American communities, Puerto Rican communities
▪ Crowded situations, malnutrition
▪ Usually seen in children
▪ May be seen in HIV + individuals
▪ M = F
▪ Histology: focal epithelial acanthos
What is this infectious disease?

(Multifocal) Epithelial
Hyperplasia/Heck’s
Disease
HPV 13,32
“Flat‐top papules”
What is this infectious disease?

(Multifocal) Epithelial
Hyperplasia/Heck’s
Disease
HPV 13,32
“Flat‐top papules”
Oral Florid Papillomatosis
What is it?
What are its types?
What is clinical appearance?
IIt’s benign HPV disease
▪ HIV infection
‐ Increased prevalence since advent of HAART therapy
‐ Multiple HPV types
▪ Down syndrome
Oral Florid
Characteristics:
‐ Diffuse, multiple locations
‐ Papillary
‐ Bumpy and tall
What is this infectious disease?

Oral Florid Papillomatosis
Very characteristic appearance
- diffused, in multiple locations
- papillary
“Multifocal, papillary lesions”
-if we biopsied these or had these removed for aesthetic regions, we’d
see that the epithelium have become white, long, taller, and bumpy
Benign
Oral HPV Lesions
HISTOPATHOLOGY
§Acanthosis
§Koilocytosis
§Binucleatedandmultinucleated keratinocytes
§Dyskeratosis
§Mitosoid figures
§Basilar hyperplasia
HPV is thought to cause –% of
oropharyngeal cancers in the US
HPV is thought to cause 70% of
oropharyngeal cancers in the US
That’s why we want to know if high risk
HPV– better prognosis
HPV Testing
▪ Pathologists order it
▪ Only do testing if pathologist sees cancer
No HPV testing on low‐risk HPV lesions (warts)
▪ No medical indication for low‐risk HPV testing b/c
‐ infection NOT associated w/ disease progression
‐ no treatment or therapy change indicated when low‐risk HPV is ID’ed
▪ HPV testing using p16 surrogate on oropharyngeal squamous cell carcinoma (SCC)
Management of Oral HPV
Lesions
Solitary Lesions
‐ Usually appear exophytic and papillary
‐ Excision is warranted
‐ Consider possible recurrence
Management of Oral HPV
Lesions
Multiple Lesions
‐ Use high power evacuation to prevent transmission
‐ Treatment = controversial
‐ Excision/ablation vs Topical vs Intralesional therapy (or combo)
‐ Consider higher rate of recurrence
HPV multiple lesions
Excision/Ablation
Excision/Ablation
▪ Scalpel
▪ Carbon dioxide laser – be cautious, don’t know what is burned away
▪ Electrosurgery
HPV multiple lesions
Topical Therapy
▪ Podophyllin resin
▪ Imiquimod (extra‐oral use only)
▪ Cidofovir
▪ Interferon
Topical Podophyllin
for what is it used
Is it FDA approved
Safe or not Durging pregnancy?
▪ Topical cytotoxic agent which arrests mitosis
▪ Genital warts and other papillomas
▪ Not FDA approved for oral warts
▪ Serious adverse reaction if absorbed systemically
▪ Pregnancy category X
Topical Imiquimod
▪ Induces cytokines + chemokines w/ resutlant anti‐virl (HPV) effects
Not FDA approved for oral warts
HPV vaccine
Newest is Gardsail 9
against many types
for both men and women
▪ 2 doses recommended for boys/girls age 11‐12 and 6mo later
▪ Recommended for everyone <26yo (MAX)
▪ NOT recommended for 26+yo unless risk for new infections (less benefit since most already exposed)
▪ Virus like particles (VLP) of L1 capsid protein present in vaccine
Results of Vaccination ▪ Drops in infections w/ HPV types that cause most HPV cancers + genital warts in
teen girls, young adult women
▪ Among vaccinated women – cervical precancers dropped by 40%
What precentge of people will be infected with HPV in their lifetime?
▪ 80% ppl will be infected in lifetime
so better take the vaccine early!
Oral Molluscum
Contagiosum
Which viruse causes it?
Clinical Appaerance?
Who get affected?
Histopathology?
Treatment?
▪ Poxvirus
▪ Presents as:
‐ pink, dome‐shaped, smooth‐surfaced or umbilicated (like belly‐button) papules ‐ with caseous plug involving skin, lips, buccal mucosa, and palate
▪ Florid cases seen in immunocompromised persons
▪ Children, young adults
▪ Histopathology characterized by:
‐ Large intracytoplasmic inclusion bodies – “Henderson‐Paterson bodies”
‐ Kids can have 6‐9mo and will go away

What is this infectious disease?

Oral Molluscum
Contagiosum
multiple pink, dome‐shaped, smooth‐surfaced or umbilicated (like belly‐button) papules ‐ with caseous plug
Measles
Which viruse causes it?
How does it spread?
Symptoms?
Clinical charcterstics?
location?
▪ Paramyxovirus
▪ Spread through respiratory droplets
▪ Symptoms: runny nose, red/watery eyes, cough, fever, rash, desquamation of skin
▪ *Characterized by Koplik’s spots
‐ Pathognomonic for measles
‐ Discrete, bluish white punctate mucosal
macules
‐ Surrounded by rim of erythema
‐ Represent foci of epithelial necrosis
‐ Often precedes skin manifestations
▪ Most common location for Koplok’s spots:
Buccal mucosa
‐ Lesions may resemble “grains of salt sprinkled
on erythematous background”
What is this infectious disease?

Measles
*Characterized by Koplik’s spots
salts/grains
Enterovirus‐Coxsackie
Virus
What diseases can it cause ?
(3)
Who do they effect?
How they are treated?
-Herpangina‐soft palate, red macules ► fragile vesicles (back of throat)
‐ Hand, foot, and mouth disease – oral lesions more in anterior regions (aphthous‐like), hand/foot (vesicles)
‐ Acute lymphonodular pharyngitis – nodules on the soft palate
▪ Usually seen in children
▪ Self‐limiting
What is this infectious disease?

Hand, foot, and mouth disease
caused by
Coxsackie
Virus
affect children
contagious
The condition is spread by direct contact with saliva or mucus.
What is this infectious disease?

Herpangina
casued by
Coxsackie
Virus
red macules and vesciles on the soft palate
a sudden viral illness in children.
It causes small blisterlike bumps or sores (ulcers) in the mouth
What is this infectious disease

Acute lymphonodular pharyngitis
Caused by
Coxsackie
Virus
Affects children
Nodules on the soft palate.
-distinctive, raised, micronodular lesions occur primarily in the pharynx and related structures and regressed without ulceration.
Rubella
(German Measles)
Which viruse causes it?
How does it spread?
Symptoms?
Clinical signs?
Assosited with what syndrome?
Is there a vaccine?
How it is diagnosed?
▪ Family: Togavirus; Genus: Rubivirus
▪ Respiratory droplets
Symptoms:
‐ Fever, headache, malaise, coryza (runny nose), anorexia, pharyngitis,
lymphadenopathy
▪ Rash – maculopapular w/ desquamation
- *▪ Forchheimer sign**
- *▪ Palatal petechiae**
▪ Congenital rubella syndrome – pandemics in past
▪ Vaccine: MMR – so we barely see this anymore
▪ Diagnosis: by serology
What is this infectious disease?

Rubella
caused by
Family: Togavirus; Genus: Rubivirus
Forchheimer sign (left) Palatal petechiae (right)
(German Measles)
What is the Most common opportunistic fungal pathogen/ infection?
Candida Species
● Over 200 species exist
● At least 15 distinct Candida species cause human disease
Mucosal/Oral infections, which are generally non‐invasive are
caused primarily by ——–
Candida albicans
>90% of invasive disease is caused by 5 most common species, which are?
‐ C. albicans
‐ C. glabrata
‐ C. tropicalis
‐ C. parapsilosis
‐ C. krusei
Candida Species
have what kind of symbiosis with humans?
● Commensalism:
‐ “long‐term biological interaction (symbiosis) in which members of
one species gain benefits while those of the other species neither
benefit nor are harmed”
● >50% of humans carry candida without harmful effects
What is Candida Species‐
Disease State
- Becomes an “infection” called candidiasis when environment changes and encourages growth
- ● Defect in cell‐mediated immune response
- ‐ Ranges from mild superficial mucosal infection ►(can be) fatal disseminated disease (usually with people with HIV and transplants)
What causes Candida
Infection?
● A disrupted balance of the normal mucosal flora
● Impaired barrier functions
● Immunosuppression
such as:
‐ Use of broad‐spectrum antibiotic
‐ Leukemia
‐ HIV
‐ Cancer chemotherapy
‐ Diabetes
‐ Xerostomia (what we deal with, candidiasis can persist here)
Normally Candida is in the commensal state and once you reach a certain level where the fungal burden has increased, you increase the c‐FOS pathway
‐ This is when the organism forms —–; once these are formed,
you see invasion into the——- cells.
Normally it is in the commensal state and once you reach a certain
level where the fungal burden has increased, you increase the c‐FOS
pathway
‐ This is when the organism forms hyphae; once these are formed,
you see invasion into the epithelial cells.
Pathogenesis‐ Key
Features
● Commensalism
- Fungus is tolerated (threshold not reached)
- Immune cells are not activated
● Pathogenicity
- Fungal burden is increased and hyphae form
- Immune cells are recruited by cytokines, chemokines
- Neutrophils are recruited and kill fungus
- Dendritic cells present antigen to T‐cells
- T‐cells also decrease fungal burden (IL‐22, IL‐17)
- Innate and acquired clear fungus to levels below threshold
How does Candida
overcome host
defenses?
6
- Dimorphism (can be spore and a hyphae‐ 2 forms)
- Phenotypic switching (change shape)
- Adhesins/Invasins (aid in attachment)
- Molecular mimicry of mammalian integrins (helps to be avoided by the immune system)
- Secretion of hydrolytic enzymes (aids in invasion)
- Phospholipase B contributes to degradation of host tissue (aids in degradation to gain entry)
Dimorphism
of
Candida
Two forms?
SPORES‐ when they are in this form, they do NOT invade
HYPHAE‐ when they begin their invasion
Crosstalk: Candida ——- play an important role in the continuous
interchange that regulates the balance between saprophytism and
parasitism
Crosstalk: Candida glycans play an important role in the continuous
interchange that regulates the balance between saprophytism and
parasitism
TYPES OF
CANDIDIASIS
INFECTION
● Superficial and localized‐more common (mild disease)
‐ Intertrigo §Paronychia/Onychomycosis
‐ “Diaper Rash”
‐ Vulvovaginitis
‐ Esophageal Candidiasis §Oral Candidiasis (Candidosis)
● Invasive, disseminated and deep infection‐rare (moderate‐severe)
‐ Affects blood (candidemia‐hospitalized), heart, brain, eyes, bones)
What is this infectious disease?

Intertrigo
a type of candidiasis
What is this infectious disease?

“Diaper Rash”
a type of candidiasis
What is this infectious disease?

Vulvovaginitis
a type of candidiasis
What is this infectious disease?

Esophageal Candidiasis
a type of candidiasis
What is this infectious disease?

Oral candidiasis
a type of candidiasis
What is this infectious disease?

Onychomycosis
a type of candidiasis
Which Candida is the most common species with what kind of Candidal Sepsis and
Disseminated Candidiasis ?
C. albicans
- Candidal sepsis means that you have the fungal moving around in your body
- Life‐threatening event in individual with severely deficient cell
- mediated immunity
- Most commonly involves urinary tract infection (women/men 4:1)
- Very rare
Oral Candidiasis
facts
● 30‐50% of people carry organism without infection (called candida
carriage)
● Rate of carriage increases with age and risk factors
● 70‐80% of oral isolates are Candida albicans
What are the Predisposing
Factors for Oral Candidiasis ?
Local and general
Local
- denture wearing
- smoking
- atopic consitituion
- steroid inhalation
- hyperkeratosis
- imblance of the oral microflora
- quality and qunatity of saliva\
General
- immunosupressive disease
- impaired health status
- immunosupressive drugs
- endocrine disorders
- hematinic deficiencies
Pseudomembranous Candidiasis
Also known as?
Key feature?
Symptoms?
In which patients it is seen?
● “Thrush”
● KEY FEATURE: Wipeable white plaques that resemble curdled milk
● Underlying mucosa is erythematous
● Asymptomatic usually
● Mild symptoms: burning, dysgeusia
● Seen in patients with: HIV, broad‐spectrum antibiotics, leukemia,
infants
What is this infectious disease?

PSEUDOMEMBRANOUS CANDIDIASIS
UNCONTROLLED
DIABETIC
When you wipe away these plaques, you might
see some Erythematous areas that causes
some of the symptoms that the patient feels
-This is MILD DISEASE

What is this infectious disease?

- *Pseudomembranous Candidiasis‐**
- Uncontrolled HIV*
● This can be mistaken with materia alba (this is just food)
‐ Should ask patient if they just ate
● This is MODERATE DISEASE
What is this infectious disease?

Pseudomembranous Candidiasis
Topical
Corticosteroid Use
Can be brought about from steroid use (steroid inhaler example)
‐ If you don’t rinse your mouth after using steroids, this can happen
■ A proliferation of hyphae
What is this infectious disease?

PSEUDOMEMBRANOUS CANDIDIASIS
Severe dry mouth
This is severe disease
we would want to use systemic treatments/
intervention
Erythematous
Candidiasis
what are its
Clinical finding?
Subtypes?
● Clinical Findings:
- Red macules or patches
- Can be due to multiple things
● Subtypes:
‐ Atrophic Candidiasis (acute‐feels like mouth has been scalded)
‐ Median Rhomboid Glossitis (asymptomatic)
‐ Denture Stomatitis (asymptomatic)
■ HAS THE SHAPE OF THE DENTURE
‐ Chronic multifocal (asymptomatic)
■ THIS HAS BEEN THERE FOR A LONG TIME
What is this infectious disease?

ATROPHIC CANDIDIASIS
● Erythematous on any mucosal
surface
● “Bald Tongue”
● Typically, painful
● (Chronic multifocal, looks
familiar)
a subtype of Erythematous
Candidiasis
What is this infectious disease?

Median Rhomboid Glossitis
a subtype of Erythematous
Candidiasis
● “Central Papillary Atrophy”
● Well‐demarcated erythematous zone
● Loss of papillae on midline posterior dorsal tongue
● Usually, asymptomatic
● “Kissing” palatal lesion
‐ Because the tongue and the palate are in contact
with each other
● Can have a diamond shape
What is this infectious disease

Denture Stomatitis
● Chronic atrophic candidiasis
● Erythema in denture bearing areas of maxilla
● Petechiae may be noted
● Usually, asymptomatic
● Consider denture care/fit/allergy/inadequate curing of acrylic
● This can occur if the patient NEVER takes off their denture
● Inflammatory papillary hyperplasia is associated with condition
● Treatment‐Nystatin applied to intaglio surface of denture and wear denture and patient to remove denture at night
a subtype of Erythematous
Candidiasis

What is this infectious disease?
a subtype of Erythematous
Candidiasis
What is this infectious disease

Angular Cheilitis
● Erythema, fissuring and scaling at angles of mouth
and commissures of mouth
● Loss of vertical dimension
● Pooling of saliva
● May be mixed bacterial/fungal infection
● Differential diagnosis can be Vit B Deficiency
a subtype of Erythematous
Candidiasis
What is Hyperplastic
Candidiasis?
● a Rare and controversial form of candidiasis
● Candidiasis superimposed on pre‐existing
leukoplakic lesion
● White plaque which cannot be removed by
scraping (NOT WIPEABLE)
● Increased frequency of epithelial dysplasia
● MUST BIOPSY then diagnose as hyperplastic
candidiasis if you see fungi post biopsy
What is this infectious disease?

HYPERPLASTIC CANDIDIASIS
What is Chronic
Mucocutaneous
Candidiasis?
● Group of rare disorders with immunologic pathogenesis
● Clinical: Severe infection of mucosal surfaces, nails and skin
● Oral‐ lesions‐thick white plaques that do not rub off but may see other
forms
Chronic Mucocutaneous Candidiasis May be associated with endocrine abnormalities (APECED);
what does APECED stands with?
‐ A: autoimmune
‐ PE: polyendocrinopathy
‐ C: candidiasis
‐ E: ectodermal
‐ D: dystrophy
Chronic Mucocutaneous Candidiasis is also genetic
associted with AIRE gene
Chronic
Mucocutaneous
Candidiasis
is
at
increased
risk of what?
● Increased risk of squamous cell carcinoma
What is this infectious disease?

Chronic
Mucocutaneous
Candidiasis
Severe infection of mucosal surfaces, nails, and skin
What is this infectious disease?

Mucocutaneous
Candidiasis
APECED
Autoimmune
Polyendocrinopathy
Candidiasis
Ectodermal
Dystrophy
Syndrome
Biopsy of the tonuge revealed SCC
How is Oral
Candidiasis Diagnosed?
● Clinical signs
● Therapeutic diagnosis
● Cytologic smear: scrape cells and look at them under the microscope
and stained with PAS stain
● Periodic Acid Schiff Stain (PAS stain)
● KOH float §Biopsy (esp. hyperplastic candidiasis)
● Culture
What are Antifungal Drug
Classes?
3
● Polyene‐Nystatin, Amphotericin B (not absorbed; used for deep fungal infections)
● Imidazole‐Clotrimazole, Ketoconazole (GI absorption)
● Triazole‐Fluconazole, Itraconazole, Posaconazole, Echinocandins
What is the treatment of
mild
Candiadisis Disease?
- Clotrimazole troches, 10 mg 5 times daily
or
- miconazole mucoadhesive buccal 50 mg tablet applied to the mucosal surface over the canine fossa once daily for 7–14 days
- Alternatives for mild disease include nystatin suspension (100 000 u/mL) 4–6 mL swished for >1min then swallow 4 times daily.

What is treatment of
moderate to severe
Candiadisis Disease?
- Oral fluconazole, 100–200mg daily for 7–14 days
● For fluconazole‐refractory disease:
‐ Itraconazole suspension 200 mg once daily OR posaconazole
suspension 400 mg twice daily for 3 days then 400 mg once daily,
for up to 28 days, are recommended
Alternatives for fluconazole‐refractory disease include:
‐ Voriconazole, 200 mg twice daily, OR AmB deoxycholate oral
suspension, 100 mg/mL 4 times daily(strong recommendation;
moderate‐quality evidence).
‐ Intravenous echinocandin (caspofungin: 70‐mg loading dose, then 50 mg daily; micafungin: 100 mg daily; or anidulafungin: 200‐mg loading dose, then 100 mg daily) (weak recommendation;
moderate‐quality evidence). §
Intravenous Amphotericin B deoxycholate, 0.3 mg/kg daily, are
other alternatives for refractory disease (weak recommendation;
moderate‐quality evidence).

What is Chronic Suppressive
Therapy?
this is when you keep the fungal infection under control for a
long time
Usually unnecessary in immunocompetent patients
● For patients who have recurrent infections:
‐ For HIV‐infected patients, antiretroviral therapy is strongly
recommended to reduce the incidence of recurrent infections
(strong recommendation; high‐quality evidence).
‐ Fluconazole, 100 mg 3 times weekly, is recommended (strong
recommendation; high‐quality evidence).
● Clotrimazole 10mg troches 1 week out of every month? (no evidence
What is Denture Stomatitis
Treatment?
YOU APPLY THE MEDICATION TO THE INTAGLIO PORTION
antifungal medication
(1) Topical Antifungal Agents
‐ Rx. Clotrimazole cream 1% vs OR
‐ Rx. Nystatin‐Triamcinolone Acetonide ointment or cream (why?
To keep the inflammation down)
■ Disp: 15g tube
■ Label: apply to angles of mouth after meals and before
bedtime
(2) Denture adjustment, reline, remake
YOU APPLY THE MEDICATION TO THE INTAGLIO PORTION
What are other ways to manage denture stomoatitis ?
● Bleach‐1 part bleach to 10 parts water (not for dentures with metallic
clasps)
● Polident (NYU Carries Polident)
● Microwave? ( could be risky, careful not to ruin the denture)
CLEANSERS FOR REMOVABLE PROSTHESIS- you have to use this everynight to avoid denture stomoatits
NYU Carries Polident
Formulation: sodium bicarbonate, citric acid, potassium
monopersulfate, sodium carbonate, sodium carbonate peroxide,
TAED, sodium benzoate, PEG‐180, sodium lauryl sulfate, VP/VA
copolymer, flavor, cellulose gum, FD&C blue 2, blue 1 lake, yellow 5, yellow 5

What is the Most common systemic fungal infection in US?
Histoplasmosis
What causes Histoplasmosis?
what is its mode of pathogensis ?
● Histoplasma capsulatum
● Dimorphic (yeast at body temperature and mold in soil)
Histoplasmosis
is endemic where
who can get infected by it?
How does is spread?
● Endemic in fertile river valleys
‐ Seen in people who spend a lot of time outside; near Ohio and Mississippi rivers
● Bird and bat excrement
● Airborne spores enter lungs through inhalation
● Macrophage ingests fungusàT‐lymphocyte immunity
● Antibodies develop several weeks later
● Macrophages may confine fungus (express disease later)
Histoplasmosis‐ Clinical
Features
● Most cases produce no symptoms or only mild symptoms
● Acute‐Self‐limited lung infection (similar to influenza; the flu)
● Chronic‐Lung infection similar to tuberculosis
● Disseminated‐Extrapulmonary spread in immunocompromised (spreads from the lungs)
● Tongue, palate, buccal mucosa
● Solitary ulcer with firm rolled borders
● Clinically appear indistinguishable from malignancy (squamous cell carcinoma)
How is Histoplasmosis Diagnosed?
How about its histology?
● Histopathology (H&E and special stain‐GMS)
● Culture
● Serology
as for histology
● Epithelioid macrophages containing histoplasma capsulatum (white arrows)
● Lymphocytes
● Plasma cells

What is the infectious disease?

Histoplasmosis
● This can be squamous cell carcinoma, shanker, ulcers
‐ Differentials for non healing ulcerations on the lateral tongue
● The white area is called the pseudomembrane
what is the treatment for Histoplasmosis?
acute
chronic
Disseminated
● Acute‐Supportive (analgesics and antipyretics)
● Chronic‐IV lipid preparation of amphotericin B or itraconazole
● Disseminated‐Lipid preparation of amphotericin B (2 weeks or more) followed by daily itraconazole for 6‐18 months
Blastomycosis
What is it?
What causes it?
What is its mode of pathogenesis?
● Uncommon fungal infection
● Blastomyces dermatitidis
● Dimorphic
Which regions can Blastomycosis happen?
● Eastern half of US which extends farther north
● Seen in the wild

How does Blastomycosis spread?
Is there any gender prediclation?
● Airborne spores enter lungs through inhalation
● M>F
Acute Blastomycosis resembles ———-
● Acute‐ Resembles pneumonia
ChronicBlastomycosis resembles ———-
Chronic Resembles tuberculosis
What are the clinical features of Blastomycosis?
● Skin lesions‐extrapulmonary dissemination from lungs
● Oral lesions‐extrapulmonary dissemination or local inoculation
● Skin lesions
● Granular(rough looking) erythematous plaques which may become verrucous(wart‐like) or ulcerated
● Oral lesions
‐ Erythematous or white ‐ Intact surface or ulceration with rolled borders
‐ Painful ‐ Ddx‐Squamous cell carcinoma
What is this infectious disease?

Blastomycosis
How to diagonse Blastomycosis?
● Histopathology (Granulomatous inflammation , Broad based budding , Double refractile cell wall)
● Cytology
● KOH
● Culture from sputum (3‐4 weeks)
● DNA probe (where you actively look for the DNA of the blastomycosis)

How to treat Blastomycosis?
● Most cases asymptomatic
● Itraconazole (mild to moderate disease)
● Systemic amphotericin B (severe cases)
● There is a connection with people taking TNF‐alpha inhibitors
Paracoccidio Mycosis
What is it?
What causes it?
A deep fungal infecion
causes by:
Paracoccidioidomycosis brasiliensis
Which regions Paracoccidio Mycosis happen?
● South American blastomycosis
Paracoccidio Mycosis is seen in the soil around ——- (name of an animal)
nine‐ringed armadillos
Paracoccidio Mycosis
what gender is more common ?
which workers are more affected?
● More common in males
● Agriculture workers
Paracoccidio Mycosis presents intially as which infection?
Pulmonary infection
What is infectious disease?

Paracoccidio Mycosis
looks like the three tail in Naruto lol

what are the clinical presentation of Paracoccidioidomycosis?
●affects the Alveolar mucosa, gingiva and palate lesions with “Mulberry‐like” ulceration (little bumps around it)
● Looks like strawberry gingivitis (differential diagnosis)
what is this infection disease ?

Paracoccidioidomycosis
looks like strawberry gingiva but it is not
How is Paracoccidioidomycosis diagnosed?
● Histopathology (- Granulomatous inflammation, Epithelioid macrophages and multinucleated giant cells,GMS or PAS, Multiple daughter buds)
● Culture
● KOH

How is Paracoccidioidomycosis treated?
● Trimethoprim/ sulfamethoxazole (mild‐moderate)
● IV Amphotericin B (severe disease)
What is Coccidiomycosis?
deep fungal infection that present as Pulmonary infection
Coccidiomycosis is known as ——-
Valley Fever
What are the two types of Coccidiomycosis ?
- Coccidioides immitis
- Coccidioides posadasii
What is the mode of pathogenesis of Coccidiomycosis?
Dimorphic organism (spores and hyphae)
Coccidioidomycosis
symptoms?
What is the Clinical Features?
how does the oral and skin lesions appear?
● Most cases are asymptomatic ~60%
● Flulike
● Fatigue, cough, chest pain, myalgia, headache
● May see a hypersensitivity reaction (valley fever) ‐ When you are over responding; immune system is over reacting
● Chronic‐mimics tuberculosis
● Disseminated‐ <1% of cases
Coccidioidomycosis
What is the Clinical Features?
how does the oral and skin lesions appear?
● Oral lesions
ulcerated granulomatous nodules
● Skin lesions: papules(slightly raised), abscesses, verrucous(patchy), plaques, granulomatous nodules
What is this infectious disease?

Coccidioidomycosis
How is Coccidioidomycosis diagnosed?
● Histopathology ( Round spherules with numerous endospores , Granulomatous inflammation, Suppurative neutrophils infiltrate, Special Stains used: GMS, PAS)
● Culture
● In situ hybridization (ISH)
● Cytology‐ scraping ulcers then stained with GMS
● Serology‐ check for antibodies
● Skin testing (limited value)

How is Coccidioidomycosis treated?
● Mild symptoms‐ no treatment usually
● Amphotericin B (‐ Immunosuppressed ‐ Severe pulmonary infection ‐ Disseminated disease ‐ Pregnant patients ‐ Life‐threatening situation )
● Itraconazole or fluconazole (fewer side effects and complications)
Cryptococcus
How common is it?
What causes it?
●Uncommon
● Cryptococcus neoformans
● Incidence increased due to AIDS epidemic in 1990s
● Pulmonary infection
● Meningitis
Cryptococcus is seen in ————–
pigeon excrement (poo)
Cryptococcus can cause what kind of infections?
● Pulmonary infection
● Meningitis ( after it spreads from the lungs to the brain. )
What are the Clinical Features of Cryptococcus?
Lung infection often asymptomatic
● Flulike illness
● Dissemination
‐ Meninges ‐ Skin ‐ Bone ‐ Prostate ‐ Oral‐papillary/granular erythematous plaques
How is Cryptococcus diagnosed?
● Biopsy ● Culture ● Serology
Note: Histopathologically they appear as Granulomatous inflammation (epithelioid histiocytes trying to confide the infection)
● Yeast are surrounded by a clear halo (capsule)

How is Cryptococcus treated?
● Mild case: Fluconazole or Itraconazole
● Cryptococcal meningitis: amphotericin B + other antifungals
Mucormycosis is caused by what?
- Infections caused by molds belonging to the order Mucorales
- Grow in natural state on decaying organic materials (saprobic‐ recycling)
- Spores may be liberated into air and inhaled by humans
Mucormycosis can affect people with what underlying conditions?
‐ Insulin dependent diabetics
‐ Bone marrow transplant recipients
‐ AIDS
‐ Patients receiving systemic corticosteroids
‐ Neutropenic patients (no white blood cells)
What are the Clinical Features of Mucormycosis?
● Rhinocerebral form
● Nasal obstruction
● Bloody nasal discharge
● Facial pain
● Facial paralysis
● Facial swelling/cellulitis
● Visual disturbances
● Into cranial vault‐blindness, lethargy, seizures
● Oral swelling/ulceration of the maxillary alveolar process/palate as a result of sinus involvement
● Black and necrotic ulcer (eschar)
● Massive tissue destruction
What is this infectious disease?

Mucormycosis‐
arrow refers to ESCHAR‐ always look for this and extreme-Black and necrotic ulcer (
we can see massive tissues destruction
What is this infectious disease?

Mucormycosis‐ CT
Sinus opacificatio
● First thing to do is to find out more about this lesion, how did this patient get this lesion?
Mucormycosis‐ Histopathology has a sepcial shape?
● Non‐septate hyphae with 90degrees branching
● You see necrosis of tissue in the area because this attacks the blood vessels

How is Mucormycosis diagnosed?
● Histopathology
● Culture
How is Mucormycosis treated?
● Surgical debridement (massive tissue destruction)
● High doses of lipid formation of amphotericin B
● Control underlying disease (main one)
● Prosthetic obturation of palatal defects
What is Aspergillosis and what causes it?
- Saprobic (in an environment rich of oxygen)
- it caused by Aspergillus flavus and Aspergillus fumigatus
Where is Aspergillosis typically seen?
how it is spread?
● Seen in hospitals and construction sights
●caused by Aspergillus flavus and Aspergillus fumigatus
● Spores are inhaled
Aspergillosis‐ Clinical Features
Two types
noninvasive
and invasive
● Noninvasive
‐ Allergic fungal sinusitis
‐ Aspergilloma (fungus ball, mycetoma [‐oma: like a tumour made of aspergillus])
● Invasive
‐ Localized (possibly after tissue damage in oral cavity)
‐ Disseminated ‐immunocompromised
Which infectious disease has fruting body in its histopathology?
Aspergillosis
Histopathology includes:
●Branching septate hyphae
● Acute angle branching
● “Fruiting body

How is Aspergillosis diagnosed?
● Histopathology
● Culture
what is this infectious disease?

Aspergillosis
arrow points toward a violaceous‐ purple colour
How is Aspergillosis treated?
● Aspergilloma‐debridement
● Allergic fungal sinusitis‐debridement and corticosteroid drugs
● Localized invasive‐debridement & voriconazole and amphotericin B
● Disseminated invasive‐consider poor prognosis even with treatment
What are Oral Manifestations of Bacterial Infections?
Caries (streptococcus mutans)
‐ Gingivitis/Periodontitis
‐ Necrotizing Periodontal Diseases
‐ Noma (Cancrum Oris)
Impetigo
‐ Erysipelas ‐
Streptococcal Tonsillitis and Pharyngitis
Scarlet Fever
‐ Diphtheria
‐ Syphilis
‐ Gonorrhea
‐ Tuberculosis
Leprosy Actinomycosis
‐ Cat Scratch Disease
‐ Bacillary Angioma
What is Necrotizing Periodontal Diseases?
Bacterial infection which presents with a spectrum of lesions
‐ Vary depending upon the localization of lesion and predisposing factors
Necrotizing Periodontal Diseases
include 4 types,what are they? What do they mean?
‐ Includes:
o Necrotizing gingivitis (NG):rapidly destructive, non-communicable microbial disease of the gingiva
o Necrotizing periodontitis (NP):apidly progressing disease process that results in the destruction of the periodontium
o Necrotizing stomatitis (NS):When the bacterial infection extends further to OTHER parts of the mouth
o NOMA (extension to skin of face) ▪ Extreme disfigurement due to bacterial infection extending onto the skin of the face
Necrotizing Periodontal Diseases
name has changed
how?
‐ The term “acute” has not been included since 1999 (ANUG=old name) o As the infections are ALWAYS acute
‐ The term “ulcerative” removed in 2017 World Workshop proposed classification “Necrotizing Periodontal Disease (NPD)” is term proposed in 2017 World Workshop for NG, NP and NS o There is ALWAYS ulceration as a result of necrosis
what are the Clinical Features of Necrotizing Periodontal Diseases?
‐ Ulceration with necrosis of interdental papillae
o Results in a “punched out” crater‐like appearance of the papilla
‐ Gray pseudomembrane
o Dead tissue ‐ EXTREMELY Painful
‐ Fetid odor
‐ Spontaneous hemorrhage Fever, lymphadenopathy, malaise
Which population affected by Necrotizing Periodontal Diseases?
Young and middle‐aged adults
Prevalence <0.1%
What is this infectious disease?

Necrotizing Gingivitis (NG)
o No periodontitis features
o SIMILAR APPEARANCE to gonorrhea
▪ Distinguishing characteristic of NG – Fetid Odor
What is this infectious disease?

Necrotizing Periodontitis (NP)
o Bone loss of the periodontium seen
What are the risk factors of Necrotizing Periodontal Diseases?
Many related factors (Multifactorial etiology):
o Psychological stress
o Immunosuppression
o Smoking
o Local trauma
o Poor nutritional status
o Poor oral hygiene
o Inadequate sleep
Which infectious diseases was known by Trench mouth?
Necrotizing Periodontal Diseases
o During WW1, soldiers that were fighting in the trenches were under extreme stress
o they commonly developed necrotizing periodontal diseases
What are the Constant bacterial species found in Necrotizing Periodontal Diseases?
Will we be able to use microbiological testing to form a diagnosis?
o Treponema spp.
o Selenomonas spp.
o Fusobacterium spp.
o Prevotella intermedia
o *Also always present in healthy gingiva ▪ so, No, Microbiological testing is NOT used to form a diagnosis
What is the Treatment of Necrotizing Periodontal Diseases?
o Removal of bacteria (scaling)
o Chlorhexidine rinse
o Antibiotics (fever or signs of systemic illness)
▪ Metronidazole ▪ Penicillin
o Oral hygiene instruction
o Supportive therapy
▪ Rest ▪ Fluids ▪ Soft nutritious diet
o Predisposing (Immunosuppressive)factors
▪ Smoking
▪ HIV?
NOMA is also called as ————
cancrum oris
What is NOMA?
Where it is seen?
‐ Rapidly progressive opportunistic infection caused by many bacteria
o More commonly seen in other parts of the world
o Seen in the US in immunocompromised patients ▪ HIV
‐ WHO estimates the global yearly incidence = 140,000
Which bacteria involved in NOMA?
‐ Polymicrobial etiology
‐ Normal flora become pathogenic during immunocompromised states
‐ Key bacteria:
o Fusobacterium necrophorum
o Prevotella intermedium ‐ Other common bacteria:
o Actinomyces pyogenes
o Bacillus cereus
o Bacteroides fragilis
o Fusobacterium nucleatum
o Prevotella melaninogenica
What are the Predisposing Factors of NOMA?
‐ Previous necrotizing periodontal disease Poverty
‐ Malnutrition or dehydration
‐ Poor oral hygiene
‐ Poor sanitation
‐ Unsafe drinking water
‐ Proximity to unkempt livestock
‐ Recent illness Malignancy
‐ Immunodeficiency disorder, including AIDS
What is this infectious disease?

NOMA
This is an aid patient
Figure 2: Extension of infection onto the face
‐ Figure 3: Lost bone and gingiva
‐ Figure 4 & 5 Bone destruction
NOMA can affect who?
Children
Adults with debilitating disease
What are the clinical features of NOMA?
Gingiva (NG) ► Adjacent tissue (necrotizing stomatitis)
+ Non‐ contiguous tissue (trauma)
► Blue black discoloration of skin
‐ Spreads through muscle, bone (osteomyelitis)
‐ Other features:
o Fetid odor
▪ Due to tissue necrosis
o Pain o Fever o Malaise
o Tachycardia o Increased respiratory rate
o Anemia o Leukocytosis o Regional lymphadenopat
What is this infectious disease?

NOMA
Development of NOMA from day 1 to day 15

What is the treatment of Noma?
o Antibiotics
▪ Penicillin ▪ Metronidazole
o Local wound care
▪ Conservative debridement to avoid iatrogenic tissue damage
o Consider nutrition, hydration and electrolyte imbalances
o May cause significant morbidity
What is this infectious disease?

Impetigo
‐ “Cornflakes glued to Surface” Appearance
o Little papules that can form little vesicles around the mouth
o Vesicles burst open and dry up around the skin of the mouth
‐ Bilateral
What causes Impetigo?
‐ Caused by:
o Staphylococcus aureus
o Streptococcal pyogenes
Damaged skin allows infection to enter
Usually affects kids
What is Impetigo Differential Diagnosis
o Recurrent Herpes Labialis
▪ Resemblance to initial impetigo stages when still unilateral
o Perioral Dermatitis
▪ Triggered by cosmetics and other substances on the skin
o Exfoliative Cheilitis (chapped lips)
How is Impetigo diagnosed and treated?
Diagnosis:
o Presumptive from clinical features
‐ Treatment:
o Topical mupirocin
o Systemic antibiotics
What is this infectious disease?

Erysipelas
Superficial skin infection in immunosuppressed adults
‐ Group A beta‐hemolytic streptococci
‐ Painful ‐ Bright‐red, well‐circumscribed, swollen, indurated (firm) ‐ Warm to touch
‐ Systemic manifestations: o High fever o Swollen lymph nodes
Diagnosis:
Cultures not useful ‐
Treatment: o Penicillin ‐ Complications without treatment
What is differential diagnosis for Erysipelas?
o Systemic Lupus Erythematosus (SLE)
▪ Due to sparing of nasolabial folds
▪ Butterfly rash in SLE resembles erysipelas
o Cellulitis (dental infection induced):
▪ Tooth infection burrowing through the tissues rather than forming an abscess
o Actinomycosis
What is Syphilis?
What causes it/
- Chronic infection
- caused by spirochete Treponema pallidum
What are the three stages of Syphillis?
Three stages
- o Primary (chancre)
- o Secondary (rash)
- o Tertiary (gumma)
What is this infectious disease?

Primary Syphilis
Chancre
at site of inoculation (3 – 90 days later)
‐ Papule ► Ulceration
‐ Most chancres occur in genital area (4% oral
What is this infectious disease?

Primary Syphilis
Chancre
at site of inoculation (3 – 90 days later)
‐ Papule ► Ulceration
‐ Most chancres occur in genital area (4% oral
What is Differential Diagnosis for Primary Syphilis (Chancre)?
3
- SCC
- Fungal Ulcer
- Trumatic Ulcer
What is this infectious disease?

Secondary Syphilis
‐ Disseminated lesions are discovered 4 ‐ 10 weeks after initial infection
‐ Resolve in 3‐12 weeks
‐ Diffuse maculopapular (flat, raised) rash
o May involve oral cavity ‐ Mucous patches
o Most common on tongue and lip
‐ Condylomata lata
o Resembles viral papillomas
‐ Systemic symptoms
What is this infectious disease?

Secondary Syphilis ( Rash)
here we see muscus patches (right) and Condylomata lata (left)
‐ Disseminated lesions are discovered 4 ‐ 10 weeks after initial infection
‐ Resolve in 3‐12 weeks
‐ Diffuse maculopapular (flat, raised) rash
o May involve oral cavity ‐ Mucous patches
o Most common on tongue and lip
‐ Condylomata lata
o Resembles viral papillomas
‐ Systemic symptoms
What is this infectious disease?

Tertiary Syphilis
Gumma
‐ Latent period for 1 ‐ 30 years
‐ 30% of patients develop tertiary syphilis
‐ Serious complications develop:
- Vascular system
- Central nervous system
- Ocular lesions
What is “Gumma”?
- o Granulomatous inflammation with tissue destruction
- o Common on palate and tongue
- o Causes a hole in the palate
Differential Diagnosis for teritiary syphillis “Gumma”
Differential Diagnosis:
- ▪ T‐cell Lymphoma
- ▪ Cocaine abuse
- ▪ Granulomatosis
- ▪ Polyangiitis
- ▪ Mucor
Congenital Syphilis is associated with what Triad?
‐ Pathognomonic features in Hutchinson triad:
o 1. Hutchinson teeth
o 2. Ocular interstitial keratitis
o 3. Eighth nerve deafness
‐ Other Features:
o High arched palate
o Saddle nose
o Frontal bossing
Clinical changes secondary to fetal infection
What is this infectious disease?

Congenital Syphilis
‐ Hutchinson Incisors (left image)
‐ Mulberry molars (right image) - not part of the triad
Syphilis
Histopathology
stage 1 and 2
Not specific ‐ Stage 1 and 2 similar
o Ulceration
o Hyperplasia (Stage 2)
o Exocytosis of neutrophils into epithelium
Intense Iymphoplasmacytic inflammatory infiltrate in superficial stroma and around deeper vascular channels (blood vessels)

Syphilis
Histopathology
Stage 3
Stage 3 o Granulomatous inflammation o Ulceration may be present ‐ Special stain “Warthin Starry”, highlights corkscrew spirochetes ‐ Immunohistochemical stain

How is Syphilis diagnosed?
o Biopsy with histopathology
o Dark field examination of a smear of active lesion
o Serologic screening lab tests
- ▪ Venereal Disease Research Lab (VDRL), RPR (non‐ specific and not highly sensitive)
- ▪ Fluorescent Treponemal Antibody Absorption (FTA‐ ABS), TPHA, TPPA, MHA‐TP (specific and sensitive)

How is Syphilis Treated?
o Single dose of parenteral long‐ acting benzathine penicillin G (primary, secondary, early latent)
o Intramuscular penicillin weekly for three weeks (late latent and tertiary
What is this infectious disease?

Secondary Syphilis
Mucous Patch
What is Gonorrhea?
What causes it?
‐ a Sexually transmitted (F>M)
caused by
‐ Neisseria gonorrhoeae
How Gonorrhea affects the body?
what complications can arrise?
‐ Genital area usually‐purulent discharge
‐ Systemic bacteremia (myalgia, arthralgia, polyarthritis, dermatitis)
‐ Pelvic inflammatory disease in women (affects pregnancies)
‐ Gonococcal ophthalmia neonatorum (infection of infant’s eyes)
What are the Clinical
Features of Gonorrhea?
‐ Oral lesions ‐ similar to aphthous
o Very rare
‐ Tonsils edematous and erythematous
‐ May simulate necrotizing gingivitis (NG) but fetor oris not present
What is this infectious disease?
Gonorrhea
looks like necrotizing gingivitis (NG) but fetor oris not present

How is Gonorrhea
diagnosed?
‐ Gram stain
‐ Culture of endocervical swab
‐ Nucleic acid amplification tests (NAATs)‐detect DNA, RNA
How is Gonorrhea
treated?
Many cases of resistance with antibiotics
§Cephalosporins
Adults with gonorrhea are treated with antibiotics. Due to emerging strains of drug-resistant Neisseria gonorrhoeae, the Centers for Disease Control and Prevention recommends that uncomplicated gonorrhea be treated with the antibiotic ceftriaxone — given as an injection — with oral azithromycin (Zithromax)
Gonorrhea can have coinfection
with what other infectious bacteria?
Chlamydia trachomatis
Chlamydia trachomatis can trigger which autoimmune disease
Reactive arthritis (reiter)
o Can’t see, Can’t Pee, Can’t Climb a Tree
▪ Causes:
● Conjunctivitis
● Urethritis
● Arthritis
Remember: Chlamydia trachomatis coininfect with Neisseria gonorrhoeae
What is Tuberculosis?
What causes it?
How does it spread?
- Chronic granulomatous infectious disease
- Caused by Mycobacterium tuberculosis
§Direct person-to-person spread through airborne droplets
Primary TB
affects previously unexposed, lungs - They breathe in the organisms that someone is coughing out
1st: C_hronic inflammatory reaction_ ► Next, a fibrocalcific nodule (Ghon focus) forms at initial site of infection
What are the chance
active disease if you get infected with Primary TB
Only 5%-10% infections lead to active disease i
“Secondary TB” reactivation
- Leads to disseminated TB (miliary TB)
- True, active TB
What is this infectious disease?

‐ Tuberculosis
What is this infectious disease?

‐ Tuberculosis
What are the causes of secondary Tuberculosis?
- Immunosuppressive medications
- Diabetes
- Old age
- Crowded living conditions
- AIDS
Tuberculosis
Clinical
Features
Primary TB
Usually asymptomatic
Tuberculosis
Clinical
Features
SecondaryTB
o Typically see lung lesions (productive cough)
o Fever, malaise, anorexia, night sweats
Tuberculosis
Clinical
Features
Extrapulmonary TB
- Lymphatics
- Skin
- Skeletal system
- CNS
- Kidney
- GI tract
- Oral cavity (uncommon)
Tuberculosis
CLINICAL FEATURES OF ORAL LESIONS
§Ulceration (tongue ulceration most common)
§Mucosal granularity
§Diffuse inflammation
§Non-healing extraction socket
What is this infectious disease?

Miliary TB
compared to miliary seeds

What is this infectious disease?

TB
Ulceration (tongue ulceration most common)
What is this infectious disease?

Primary Oral TB
tongue ulceration
What is this infectious disease?

Primary Oral TB
Oral Primary TB clinical manifestation is very rare
TB is directly in the epithelial cells.
Person coughs ⇒ organism enters broken skin somewhere in the
oral mucosa ⇒directly causing TB in the mouth
-this person would NOT have any issues in their lungs
-primary TB = infection went directly into their mucosa from another person
What is the Differential Diagnosis of non‐healing ulcer?
o TB
o Deep fungal infections
o Traumatic ulcer
o SCC
o Major Aphthous ulcer
What is the histological features of Tuberculosis
Granulomas
- o Epithelioid histiocytes
- o Multinucleated giant cells
- ▪ * Langhans giant cells
- ● Nuclei along the periphery
- ▪ * Langhans giant cells
- o Central caseous necrosis
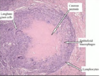
TB staining
Special stain Epithelioid
o Ziehl‐Neelson or AFB
o Consider scarcity of organisms
o MAY NOT VISUALIZE ORGANISMS WITH STAIN
▪ NEGATIVE RESULT DOES NOT RULE OUT TB INFECTION

How is Tuberculosis treated?
§Multiagent therapy for active infection to prevent mutation and resistance
§8 week course
§Pyrazinamide
§Isoniazid
§Rifampin
§Ethambutol
§Followed by 16 week course
§Isoniazid
§Rifampin
‐ Chemoprophylaxis
‐ For positive PPD but no active infection
‐ BCG vaccine
o Not used in US due to controversy regarding effectiveness
How is Tuberculosis
diagnosed ?
o TB‐Test
§Delayed type hypersensitivity (Type 4)
§Checks if developed an immune response to TB
§PPD (purified protein derivative) (what they inject under the skin)
§T cells are attracted by immune system to the skin site
§Lymphokines induce hard raised area with clear margins
§Need to check 48-72 hours later (measure area)

What is Non‐Tuberculosis
Mycobacterial
Infection
Scrofula
What causes scrofula?
Mycobacterium bovis
Infected milk leads to scrofula
RARE today as milk is pasteurized
What are the clinical features of scrofula?
o Enlargement of oropharyngeal lymphoid tissues and cervical
nodes
o Significant caseous necrosis may occur and cause sinus tracts
to skin
What is this infectious disease?

Scrofula
Leprosy is also known as ———
Hansen disease
What causes Leprosy?
Mycobacterium leprae
What are the two types of Leprosy?
1. Tuberculoid leprosy
▪ High immune reaction
▪ Oral manifestations are RARE
2. Lepromatous leprosy
▪ Reduced cell‐mediated response
Leporsy prevelance & in which regions it is usually found?
EXTREMELY RARE
o 80% of cases occur in:
▪ Brazil
▪ India
▪ Indonesia
▪ Madagascar
▪ Myanmar
▪ Nepal
▪ Nigeria
What are the clinical features of Leporsy ?
Clinical features:
o Leonine facies
▪ Appearance of a lion
● Loss of eyebrows
● Scarring (fibrosis) from infection prevents hair
growth
o * Oral Manifestations seen in areas of mouth with lower
temperatures:
▪ Hard/soft palate
▪ Maxillary gingiva
▪ Tongue
Oral‐enlarging papules ► ulcer ► necrosis
What is this infectious disease?

Leprosy
What is this infectious disease?

LEPROSY
Clinical features
- *§Bone destruction** ( hole in the palate)
- *§Nodular** will become nectortic and then destruction will follow
LEPROSY How is it diagnosed?
Diagnosis:
o Clinical presentation
o Acid fast stain
Histopahology
No well‐formed granulomas
o Lepromatous leprosy
diffuse presentation

How is Leprosy treated?
§Rifampicin, clofazimine, dapsone
What is Actinomycoses?
‐ Infection caused by filamentous branching gram positive anaerobic
bacteria
‐ Normal component of oral flora
What causes Actinomycoses?
‐ Associated Bacteria:
o Actinomyces israelii
o Actinomyces viscosus
‐ Normal component of oral flora -gram positive anaerobic
bacteria
What are the clinical features of Actinomycoses?
can be Acute or chronic
‐ Hard indurated swelling
o Result of injury / trauma
▪ Tooth extraction
o Erythematous
o Formation of external sinus
▪ Drains into the skin
‐ “Sulfur granules”
o May be present in suppuration
o Indurated area of fibrosis
Which locations Actinomycoses affect?
‐ 55% in cervicofacial area
‐ Hard indurated swelling
o Result of injury / trauma/tooth extraction
o Erythematous
‐ Area overlying angle of mandible
o Formation of external sinus
▪ Drains into the skin
‐ Other locations include:
o Abdomen
o Pelvis
o Lungs
What is this infectious disease?

Actinomycoses
it’s an external Sinus
How does Actinomycoses infection spread?
‐ Enters tissue through an area of prior trauma
o Soft tissue injury
o Periodontal pocket
o Non‐vital tooth
o Extraction socket
o Infected tonsil
‐ Direct extension through soft tissue to the surface
What is “Sulfur granules”
Where it is found?
In which infection?
color?
colonies of bacteria (o Actinomyces israelii
o Actinomyces viscosus)
found in suppuration (pus) which means Suppuration (pus) is dead tissue, bacteria, dead white blood cells, and other products of tissue breakdown..
Sulfur granules found in Actinomycoses
yellow in color
Differential Diagnosis to Actinomycoses
o Erysipelas
What are other presentations of Actinomycoses?
‐ Tongue
‐ Tonsillar crypts
‐ Salivary gland involvement
‐ Osteomyelitis
‐ Periapical inflammatory lesions
what is the histology of Actinomycoses and stain used?
‐ Colony of actinomycotic organisms surrounded by neutrophils
‐ Grocott‐Gomori methenamine silver stain (GMS)
In this histo slide, we see:
* Sulfur Granule
o 1. Collection of actinomycoses israelii organisms
o 2. MANY neutrophils surround the periphery
o BOTH are requirements for a TRUE diagnosis of actinomycoses

‐ Actinomycoses
o Diagnosis
-
Culture
- o < 50% of cases are positive
- ▪ Due to various types of bacteria in the culture
- o < 50% of cases are positive
- Presumptive diagnosis from biopsy
in this histology: GMS stain was used
o Correlates with top H&E histopathology
o Filamentous branches are the actinomycotic organisms

How is Actinomycoses treated?
- * Prolonged high dose antibiotics for cervicofacial actinomycosis
- Due to the fibrosis that occurs
- Early cases 5‐6 weeks
- Deep‐seated infections up to 12 months
- Abscess drainage
- Sinus tract excision
- Penicillin
What is Cat‐Scratch
Disease?
‐ Infectious disease which is seen in lymph nodes
What causes Cat‐Scratch
Disease ?
‐ Causative organism:
o Bartonella henselae
‐ Previous contact with a cat (scratch or saliva)
What are the age of the patients that usually get Cat‐Scratch
Disease ?
‐ 80% in patients younger than 21
—– is the most COMMON cause of regional lymphadenopathy in children
(22,000 cases annually)
Cat Scratch Disease
What are the clinical features of Cat Scratch Disease ?
‐ Initial scratch
‐ Papule at inoculation site (3‐14 days later)
‐ Papule ► erythematous ► vesicular ►crusted
‐ Healing (1‐3 weeks)
‐ Lymph node enlargement with fever and malaise
What are the Differential Diagnoses: of Cat Scratch Disease ?
‐
o Swellings in the lymph node
o Unilateral swellings of the neck
How is Cat‐Scratch Disease
diagnosed ?
‐ Clinical features:
o Presence of a cat
▪ Presumptive diagnosis can be made
‐ Serology (antibody detection)
‐ Histopathology (biopsy) (Stellate suppurative necrosis surrounded by a band of histiocytes and neutrophils) and the use of Immunohistochemistry and Warthin‐Starry silver stain to identify the organism
Left
o Histiocytes on the periphery
o Stellate necrosis in the center
‐ Middle Immunohistochemistry
o Antibodies allow for visualization of Bartonella henselae (red
little dots)
‐ Right : Warthin‐Starry silver stain
o Silver stain allows for visualization of Bartonella henselae
(black areas)

How is Cat‐Scratch Disease
treated?
o Self‐limiting (resolves within 4 months)
o Local heat
o Analgesics
o Mechanical removal of suppuration (aspiration)
o May use antibiotics for severe cases
▪ Azithromycin
What is this infectious disease?

Cat‐Scratch
Disease


