Microbiology 5 - CNS infections and meningitis Flashcards
Which antibiotic should be used first line in meningitis?
Ceftriaxone
Is listeria meningitis is suspected, what antibiotic therapy should be used?
Ceftriaxone plus amoxicillin
Which pathogen is most likely to be the cause in myelitis?
Poliovirus
What is myelitis?
Inflammation of the spinal cord
Recall the 3 most likely causative organisms in acute meningitis, and the most susceptible demographic of patient to each
N. meningitidis = young
S. pneumoniae = elderly (so vaccine at 65 years)
H. influenzae = those who haven’t had HiB vaccine
What is the most commonn cause of meningitis in neonates?
Group B strep
What is the most likely causative organism in chronic meningitis?
TB
(or cryptococcus according to path guide)
What is the most likely causative organism in aseptic meningitis?
Coxsackie virus
Describe the rash produced by meningococcal meningitis
Non-blanching purpuric rash
What is the most likely viral cause of encephalitis in the UK and worldwide?
UK: HSV 1
Worldwide: WNV
Recall 3 possible routes of infection that may cause a brain abscess
Direct expansion from
- otitis media
- mastoiditis
- paranasal sinusitis
What is the most common type of spinal vertebral infection?
Pyogenic vertebral osteomyelitis
What is the most common cause of pyogenic vertebral osteomyelitis?
Infective endocarditis - staph/ strep can be ‘flicked off’ the valve
What is the first investigation to do in suspected meningitis?
Blood cultures
Recall the stains used in CSF analysis to look for a) bacteria b) TB and c) fungi
a) gram stain
b) auramine stain
c) India ink
If “alpha haemolytic diplococci” are found in CSF, what is the pathogen causing meningitis?
Streptococcus pneumoniae
What is the normal range for CSF protein?
0.15-0.4
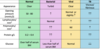
What is the appearance of CSF in purulent vs aseptic vs TB meningitis?
Purulent: turbid
Aseptic/ TB: slightly turbid or clear
What type of cell is elevated in the CSF in purulent vs aseptic vs TB meningitis?
Purulent: polymorphs
Aseptic/ TB: lymphocytes
In which type of meningitis will gram stain antigen tests be positive?
Purulent meningitis
Which type of meningitis produces the most protein in CSF?
TB meningitis
What is the empirical therapy for meningitis?
Ceftriaxone 2g IV bd
Add amoxicillin if >50 or immunocompromised
ALSO GIVE STEROIDS (DEXAMETHASONE) (as long as >1 month old and NOT MENINCOCCOCAL)
What are the routes of infection into the CNS and which is the most common?
Haematogenous spread (e.g. pneumococcus, meningococcus, herpes)
Direct implantation (e.g. trauma)
Local extension (e.g. from the ear)
PNS to CNS (e.g. rabies)
*haematogenous is the most common
Which organisms cause aspetic meningitis?
Herpes
Enteroviruses
3 big causes of acute meningitis
Neisseria
Haemophilus
Strep Pneumoniea
Incidence of rash with N. Meningitidis
A nonblanching rash develops in 80% of children
A maculopapular rash remain in 13% of children and no rash in 7%
How quickly do you need to give antibiotics for N. Meningitidis infection?
Within 1 hour