Mental Health Flashcards
How prevelant is depression in primary care?
Discuss some important aspects of history to explore in patient presenting with suspected depression
- Assess suicide risk
- Consider any factors which may affect development, course or severity of depression e.g. history of depression, living coniditons, employment etc….
- Identify any safeguarding issues
- Assess for any comorbid conditions associated with depression
- Use a validated tool to assess depression
Discuss some risk factors for depression
- Personal or family history of depressive disorder
- Co-existing medical conditions
- Age >65yrs
- Oral contraceptives
- Corticosteroids
- Recent childbirth
- Adverse childhood experiences
*
Discuss typical presentation of depression; hightlight two/three core symptoms
*NOTEL these are symptoms used in DSM-5 criteria
Core Symptoms
- Feeling down, depressed or hopeless
- Little interest or pleasure in doing things
- Reduced energy (only core symptom on ICD10)
Associated Symptoms
- Disturbed sleep (decreased or increased compared to usual).
- Decreased or increased appetite and/or weight.
- Fatigue/loss of energy.
- Agitation or slowing of movements.
- Poor concentration or indecisiveness.
- Feelings of worthlessness or excessive or inappropriate guilt.
- Suicidal thoughts or acts.
What criteria do we use to diagnose depression? Describe this criteria
DSM-5 criteria:
- Have at least one of the two core symptoms of depression (feeling low & lack of interest) for most days for over 2 weeks
- Explore to see if have any other symptoms of depression to help classify severity into:
- Subthreshold depression
- Mild depression
- Moderate depression
- Severe depression
For each of the following categories of depression, discuss DSM-5 criteria for each:
- Subthreshold depression
- Mild depression
- Moderate depression
- Severe depression
FOR ALL, must have at least one of two core symptoms aswell as:
- Subthreshold depression: total of 2-4 symptoms
- Mild depression: few, if any, symptoms in excess of five symptoms and they only result in minor functional impairment.
- Moderate depression: is diagnosed if symptoms or functional impairment are between mild and severe.
- Severe depression: has most symptoms and they markedly interfere with functioning – they can occur with or without psychotic symptoms.
What is dysthmia?
Peristent subthreshold depression: subthreshold symptoms for more days than not for at least 2 years, which is not the consequence of a partially resolved ‘major’ depression.
What is seasonal affective disorder?
Episodes of depression which recur annually at the same time each year with remission in between (usually appearing in winter and remitting in spring).
Discuss what investigations you might do, if any, for someone presenting with suspected depression
Largely a clinical diagnosis however may consider investigations to rule out other pathology e.g.:
- FBC: rule out anaemia as cause for fatigue
- TFTs: rule out thyroid pathology
- Glucose: rule out diabetes as cause for fatigue
- U&Es:
- LFTs:
- Calcium:
May do a ‘metabolic panel’ tests for most of aboive

What is PHQ-9 questionnaire?
Depression questionnaire that reflects the DSM-5 criteria. It classifies current symptoms on a scale of 0 (no symptoms) to 4 (daily symptoms). It has been validated for use in primary care settings. Repeating the PHQ-9 during treatment allows the clinician to objectively monitor response to therapy.
State some of the questions on the PHQ 9 questionnaire
Remember, patient answers each question on scale of 0 (no symptoms) to 4 (daily symptoms) and a total score is produced. Over the last 2 weeks how often have you been bothered by any of the following:
- Little interest/pleasure in doing things
- Feeling down, hopeless, depressed
- Trouble falling alseep or staying asleep
- Feeling tired or having little energy
- Poor appetite or overeating
- Feeling bad about yourself- like you are a failure or have let your family or yourself down
- Trouble concentrating on things
- Moving or speaking so slowly that other people have noticed (or the opposite- being figety and unable to keep still)
- Thoughts of hurting yourself or that you would be better off dead
*NOTE: 10th question not included in score that asks how difficult these symptoms/feelings have made everyday life e.g. work, take care of things at home, get along with other people etc..
Interpret the following scores on PHQ 9:
- 0-4
- 5-9
- 10-14
- 15-19
- 20-27
- 0-4: minimal depression
- 5-9: mild depression
- 10-14: moderate depression
- 15-19: moderately severe
- 20-27: severe depression
State some other depression screening tools (other than PHA-9)
- Edinburgh Potnatal Depression Scale
- HADS-10
- BDI-II
Discuss how you would manage someone with subthreshold depression or someone with mild depression who does not want intervention
- Dicuss problems & concerns
- Provide information about nature & course of depression
-
Offer advice to help boost mood:
- Talking to family & friends
- Enough sleep
- Nutrition
- Relaxation techniques
- Arrange follow up in 2 weeks (contact if they don’t turn up)
Discuss the management of someone with persistent subthreshold depressive symptoms or mild to moderate depression
- Consider low intensity psychosocial intervention
- Offer group CBT if decline low intensity psychosocial intervention
-
Consider antidepressants if:
- History of moderate or severe depression
- Subthreshold depressive symptoms >2yrs
- Other interventions not worked
- Depression is complicating care of a chronic physical health problem
Discuss the management of moderate or severe depression
- Antidepressant
- High intensity psychological intervention
- Counselling if decline both of above
- Offer sleep hygience advice for those who have difficulty sleeping
- Provide information & advice about depression & it’s treatment
The Mental Health Act allows compulsory admision of people who…. (2)
- Have a mental disorder of a nature or degree that warrants assessment or treatment in hospital
- Needs to be admitted in the interests of their own health or safety, or for protectin of other people
Discuss the difference betwen low and high intensity pyshcological interventions
- Low intensity: individual does a lot of work themselves with less support from professionals e.g. individual guided self-help based on principles of CBT (e.g. via workbooks, websites etc..) with a few short face to face or telphone consultaitons
- High intensity: professionals more heavily involved, mainly based around sessions and healthcare professional and pt doing work together e.g. indiviudal CBT, couples therpay etc…
*NOTE: may see group CBT as an inbetween
Alongside management already discussed for different categories of depression, what should you offer all pts with depression?
- Verbal & written information
- Advice about self-help groups
- Advice about organisations e.g. MIND, Samaritans
What should you explain to someone who is starting antidepressants?
- Explain suicide risk (increased risk of suicide when first start taking)
- Symptoms of anxiety may initially worsen
- Take time to work
- Need to continue for at least 6 months after symptoms have resolved to reduce risk of relapse
- Do not suddenly stop taking them
- Antidepressant drugs are not addictive but 1/3 peole experience discontinuation symptoms
- Some antidepressants have sedating effects and may affect a person’s ability to drive; effect likely to be greates in first month. Don’t drive if affected
What antidepressants should be prescribed in patients with depression?
*Include first line, second line etc…
- First line= SSRI (NOTE: if pt has had good response to antidepressant previously can go with sam one)
- Second line= increase dose or switch to different SSRI or try TCA
- Third line= consider other antidepressants e.g. Mertazepine
Describe the mechanism of action of the following drugs:
- SSRIs
- SNRIs
- TCAs
- SSRIs: inhibit reuptake of serotonin to increase serotonin in synaptic cleft and therefore increase binding to post-synaptic receptor
- SNRIs: inhibit reuptake of noradrenaline to increase noradrenaline in synaptic cleft and therefore increase binding to post-synaptic receptor
- TCAs: block reuptake of serotonin and noradrenaline to increase concentrations in synaptic cleft and increase bindng to post-synaptic receptor
Which SSRI is preferred in patients with chronic physical health problems?
Sertraline as it has lower risk of drug interactions
State some examples of:
- SSRIs
- SNRIs
- TCAs
- SSRIs: citalopram, fluoxetine, paroxetine, sertraline
- SNRIs: desvenlafaxine, duloxetine, levomilnacipran, venlafaxine
- TCAs: amytriptyline, nortriptyline, doxepine
For each of the following conditions/situations, state which antidepressants should not be offered:
- NSAIDs
- Warfarin
- Heparin
- Aspirin
- Anti-epileptic drugs
- Triptans
- MAO-B
- Flecainide
- NSAIDs: avoid SSRIs and SNRIs (but if not suitable alternative found offer GI protection)
- Warfarin: avoid SSRIs, SNRIs, TCAs
- Heparin: SSRI and SNRIs
- Aspirin: SSRIs and SNRIs
- Anti-epileptic: seek specialist advice as all antidepressants lower seizure threshold
- Triptans: SSRIs
- MAO-B: SSRIs
- Flecanaide: do not offer citalopram or escitalopram
State some ADRs of SNRIs and SSRIs
- feeling agitated, shaky or anxious
- feeling and being sick
- indigestion and stomach aches
- diarrhoea or constipation
- loss of appetite
- dizziness
- not sleeping well (insomnia), or feeling very sleepy
- headaches
- low sex drive
- difficulties achieving orgasm during sex or masturbation
- in men, difficulties obtaining or maintaining an erection (erectile dysfunction)
These side effects should improve within a few weeks, although some can occasionally persist.
State some ADRs of TCAs
- dry mouth
- slight blurring of vision
- constipation
- problems passing urine
- drowsiness
- dizziness
- weight gain
- excessive sweating (especially at night)
- heart rhythm problems, such as noticeable palpitations or a fast heartbeat (tachycardia)
The side effects should ease after a couple of weeks as your body begins to get used to the medicine.
What is serotonin syndrome?
- Adverse drug reaction caused by excessive central and peripheral serotonin
- Can occur hours-days after initiation of new drug, dose escalation or overdose
- Symptoms vary from mild to life-threatening & can be classifed into three main categories:
- Neuromuscular hyperactivity (tremor, hypereflexia, rigidity)
- Autonomic dysfunction (tachycardia, hyperthermia, diaphoresis, nausea & vomiting)
- Altered mental state (agitation, confusion, mania)
Can someone take St John’s wort with depression tablets?
NO
What monitoring needs to be done for patients on antidepressants?
Depends on drug and pt but consider:
- U&E’s to monitor sodium
- BP
- ECGs
- Mood
Which patients are at increased risk of devlopoing hypontraemia whilst taking SSRIs?
- Older age
- History of hyponatraemia or low baseline sodium
- Co-therapy with drugs known to cause hypokalaemia
- Low body weight
- Medical comorbidity
What follow up is required for someone who has been diagnosed with depression?
- Arrange initial follow up 2 weeks later **NOTE: if suicidal or <30yrs this should be done in 1 week
- Review regularly (e.g. every 2-4 weeks) next 3 months
- If response is good consider longer intervals
State some potential complications of depression
- ADRs from treatment e.g. weight gain, decreased sexual desire, serotonin syndrome
- Recurrence
- Suicide
Discuss the prognosis of depression
- Depression recurs in about one third of patients within 1 year of discontinuing treatment and in more than 50% of patients during their lifetime.
- After 15 years, 87% will experience a recurrence.
- For patients with 3 recurrent depressive episodes, many experts advocate long-term maintenance therapy.
What’s the difference between low mood and depression?
- Low mood: tends to last few days to few weeks. Often after distressing event or major life change
- Depression: lasts longer and may have feelings of hopelessness
What do we mean by generalised anxiety disorder?
State some other anxiety disorders
- Chronic, excesive worry for at least 6 months about everyday issues that is disproprtionate to inheret risk that causes distress or impairment
- Other anxiety disorders:
- Social phobia
- Specific phobias
- Panic disorder
- Obsessive compulsive disorder
- PTSD
Describe typical presenting features of generalised anxiety disorder in adults
- Restlessness or nervousness
- Easily fatigued
- Poor concentration
- Irritability
- Muscle tension
- Sleep disturbance
NOTE: these are the DSM-5 criteria for GAD
In primay care GAD can present soley with physical symptoms such as headaches, muscle tenson, GI symptoms, back pain, insomnia and may not readily report worry or psychological stress; true or false?
True
How do we diagnose GAD according to DSM-5 criteria (3 main criteria)
- At least 6 months of excessive, difficult to control worry about everyday issues disproportionatte to inherent risk and causes distress or impairment
- The worry is not confined to features of another mental disorder or as a result of substance abuse or a general medical condition
- Must have 3 out of the possible 6 key symptoms:
- Restlessness or nervousness
- Easily fatigued
- Poor concentration
- Irritability
- Muscle tension
- Sleep disturbance
State some risk factors for developing generalised anxiety disorder
- Family history
- Female
- Increased stress
- History of physical or emotional trauma
- Comorbid depression
- Substance abuse/dependence
- Other anxiety disorder
Who does generalised anxiety order commonly affect?
- Females > men
- Ages 35-59 most common
What questionnaire can be used to screen for generalised anxiety disrorder?
GAD 7 questionnaire
State some of the question and answer options onthe GAD 7 questionnaire
Over the last 2 weeks how often have you been bothered by any of the following problems; score from 0 (never) to 3 (everyday):
- Feeling nervous, anxious or on edge
- Not being able to stop or control worrying
- Worrying too much about different things
- Trouble relaxing
- Being so restless that it is hard to sit still
- Becoming easily annoyed or irritable
- Feelinga afraid as if something awful might happen
Interpret the following results of the GAD-7 questionnaire:
- 0-4
- 5-9
- 10-14
- 15-21
- 0-4: minimal anxiety
- 5-9: mild anxiety
- 10-14: moderate anxiety
- 15-21: severe anxiety
Other than the DSM-5 criteria, what other criteria can we use to screen for GAD
ICD-10 for GAD. Diagnostic criteria includes:
- Anxiety is generalised and persistent but not restricted to or even strongly predominating in any particular environmental circumstance
- Variable dominant symptoms including: persistent nervousness, trembling, muscle tension, sweating, light-headedness, palpitations, dizziness and epigastric discomfort
- Expression of fears such as that the person or a relative will shortly become ill or have an accident
Discuss what, if any, investigations are required for generalised anxiety disorder
Largely a clinical diagnoses; defined by DSM-5 criteria. Investigations to consider to rule out other pathology includes:
- TFTs
- Urine drug screen
- 24hr urinary metaneprhines
- ECG
Discuss the ‘stepped management’ of generalised anxiety disorder
Step 1: ALL PATIENTS
- If comorbidities present e.g. depression clinician should decided which is most significant (in terms of severity and likely response to treatment) and treat that first
- Discuss practical solutions to stressors contributing to GAD
- Provide verbal & written information about GAD and it’s treatment
- If anxiety symptoms are mild= period of active monitoring
Step 2: if symptoms not resolved after step 1
- Offer low intensity psychological intervention (e.g. self help or CBT group therapy)
Step 3: if there is marked functional impairment or symptoms not resolved after step 2
-
High intensity psychological intervention or drug therapy
- First line drug= SSRIs
- Second line drug= SNRIs
- Thrid line drug= pregabalin
Step 4:
- Refer to specialist if GAD is complex & there is risk of inadequete response to treatment, very marked functional impairment, risk of self harm and/or self neglect, suicide or significant co-morvidity e.g. subtance misuse, complex physical health problems
What advice/lifestyle changes may you suggest to someone with GAD in step 1 of management?
- Sleep hygiene
- Regular exercise
- Health diet
- Mindfulness
- Self help resources e.g. websites, books
If a women who is pregnant presents with GAD, what step in the the ‘management ladder’ should we start at?
Start at step 3 management (ideally offer high intesntiy psychological intervention then offer drug treatment at lowest effective dose if HIPI not successful)
Use of SSRIs or SNRIs after around 20 weeks of pregnancy can cause what 2 complications
- Persistent pulmonary hypertension of the newborn (PHHN)
- Neonatal withdrawal
Discuss what monitoring is required for GAD
- It is a chronic, fluctuating, remitting & relapsing disorder that generally requires long term treatment.
- After trial of pharmacotherapy for over 12 weeks effective treatment should be continued for at least 12 months
- A trial taper from the medication may be trialled in that time with treatment reinstated if relapse occurs
State some potential complications of GAD
- Comorbid depression (occurs in 50% of pts- have a more severe & prolonged course)
- Comorbid substance abuse or dependence
- Other comorbid anxiety disorders
Discuss the difference between stress & generalised anxiety disorder
- Stress due to external origin and stops when stressor removed
- Anxiety is internal origin and does not stop when stressor removed

What antidepressants are safe in pregnancy?
Category C= animal studies show risk, caution is advised, benefits should outweigh risks
Category D= evidence of risk to human fetus, benefits may outweigh risks in serious conditions

What antidepressant is most commonly used in children?
Fluoxetine
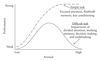
Describe the Yerkes & Dodson curve
What is a mental state assessment?
Describe what is involved/how to do a mental state assessment
MSE is a way of observing and describing a patient’s current state of mind based on domains such as appearance, attitude, behaviour, mood, speech, thought process, thought contenet, cognition, insight, judgement… When combined with biographical and historical information it allows clinician to make accurate diagnosis and formulation.
Perfroming the assessment
- Appearance: scars, signs drug use, tattoos, weight, stigmata of disease, hygience, clothing, objects they brought with them
- Behaviour: engagement & rapport, distrated, eye contact, facial expression, body language, psychomotor ativity, restlessness, abnormal movements or postures
- Speech: rate of speech, quantity, tone, volume, fluency of speech
- Mood & affect: mood= predominant subjective internal state, affect= immediately expressed & observed emoion (mood is what pt tells you, affect is what you see). Look at range and mobility of affect, intensity of affect, congruency of affect
- Thoughts: speed of thought processing, flow and coherence of thoughts, thought content, though posession
- Perception: hallucinations, illusions, depersonalisation, derealisation
- Cognition
- Insight: do they have ability to understand they have mental health problem and it is abnormal
- Judgement: can ask questions to see if make sensibile decisions when presented with information. e.g. if house was on fire what would you do?
**SEE GEEKYMEDICS FOR FULL- really useful.
It is common in primary care to perform an assessment of a patient’s level of cognition (often because a family member is concerned about their memory); state two tools we can use to assess cognitive function
- MMSE
- GPCOG
Describe how to perfrome a MMSE (mini mental state examination)

Interpret the MMSE score

Describe how to perform a GPCOG (General practioner assessment of cognition)
Has two parts: patient examination & informant interview (which is conducted if the results from patient examination inconclusive/score 5-8)
Patient Examination
- Give them an address (name, number and street, town) and ask them to repeat it back to you. Then tel them you want them to remember it as you will ask again later.
- What is the date?
- Ask them to put all numbers on a blank clock template
- Ask them to mark a time e.g. 11:10am
- Can you tell me something that happend in the news recently (i.e. last week)- require specific details/answers
- What was the name and adress I asked you to remember?
Informant interview (ask how pt is compared to when they were well- say 5 to 10 yrs ago. Answer yes, no, don’t know, N/A)
- Does patient have more trouble remembering things that have happened recently then they used to?
- Does he or she have trouble recalling conversations a few days later?
- When speaking, does the patient have difficulty in finding the right word or tend to use the wrong words more often?
- Is the patient less able to manage money & financial affairs?
- Is the patient less about to manage their medication independently?
- Does the patient need more assistance with transport (if difficulties due to only physical problems tick no)
Interpret the GPCOG score
Patient examination
- 9/9= no significant impairment
- 5-8= more information required, proceed with step 2/informant section
- 0-4= cognitive impairment indicated; conduct standard investigations
Informant section (to get total score add number of items added no, don’t know or N/A)
- Score 0-3= congitive impairment indicated
State some factors associated with an increased risk of a person committing suicide
*Lots of factors, just name a few
- Previous suicide attempt
- Family history of suicide
- Mental illness e.g. depression
- Social isolation
- Criminal problems
- Financial problems
- Job problems or loss
- Legal problems
- Serious illness
- Substance use disorder
- Adverse childhood experiences
- Bullying
- Relationship problems
- Barriers to healthcare
Describe the factors that might offer a person some protection against comitting suicide
- Connections to friends, family and community support
- Cultural and religious beliefs that discourage suicide
- Supportive relationships with care providers
- Limited access to lethal means
- Availability of physical & mental health care
- Coping & problem solving skills
Which groups of people at at high risk of suicide?
- Young and middle-aged men.
- People in contact with the criminal justice system.
- Specific occupational groups, for example, doctors, nurses, veterinary workers, farmers, agricultural workers
What is a suicide risk assessment?
Explain how to conduct a suicide risk assessment
Assessment, via asking numerous questions, to determine whether person is likely to attempt suicide. Questions are shown in image… general topica areas include:
- Whether they have thought about suicide or death?
- Personal or FH of suicide attempts or suicide. If there is personal history must explore in depth: before, during, after
- If they have thought about suicide, have they considered a method and/or made any preparations?
- Protective factors
- Risk factors
- PMH
- Social history- take extensively!!!
- Drug history
***See geeky medics for comprehensive guidance

Following a suicide risk assessment, discuss what you would do if you determine a patient is:
- Low risk
- High risk
- Low risk: discuss and/or create a safety plan with them detailing steps they should take if situations deteriorates. Management of precipitating factors, CBT, antidepressants etc…
- Moderate risk: not immediate risk of suicide but made plans for suicide. Refer to mental health crisis team
- High risk: if considerable immediate threat to themselves or other refer them urgently to specialist mental health services (may detain under mental health act)
Explain the similarities and differences between suicide and self harm
Similarities
- Both demonstrate that person is in personal distress and needs some help
Differences
- Self harm is a means of coping with distress in attempt to try and avoid escalation e.g. to suicide
- Suicide is an attempt to escape distress
State some resources that you can suggest to patients to use when they are experiencing suicidal ideation
Alongside family, GP, 111, mental health crisis team (if have one) other example resources include:
- Samaritans
- CALM (campaign against living miserably)
- Childline
- SOS suicide silence
- SHOUT crisis text line
- YoungMinds crisis text line
Stat some resources that you can suggest to patients to use when they are dealing with the conseqeunces of attempted suicide
Same resources as before e.g:
- Samaritans
- CALM
- SOS suicide line etc…
*NOTE: these resources are also available for those who are affected by suicide of someone close to them
Also encourage use of the following in the future:
- ReMinder app
- Encourage them to write a safety plan (prupose is to remind you of reasons to live, connecting you with people and services that can help. giving you prespective. ReMinder app does the same thing)
Define self harm
Intentional act of self-poisoning or self-injury, irrespective of the motivation or apparent purpose of the act, and is an expression of emotional distress.
*NOTE: suicide attempt is classed as self-harm
State some factors which are associated with self harm
- Age (16-24yrs in women, 25-35 in men)
- Stressful life event
- Social isolation
- Mental health problems
- Chronic physical health problems
- Alcohol or drug misuse
- In criminal injustice system
- Socio-economic disadvantage
Discuss the relationship of self-harm to suicide
Discuss the acute management of self-harm in primary care
- Examine any physical injuries
- Assess emotional & mental state and for presence of features that may increase risk e.g. depression, suicide risk, substance misuse
- Assess presence of protective factors
- Assess for any safeguarding concerns
- Consult with TOXBASE if self-poisoned
- If physical injuries and/or acute mental state thought to pose significant risk offer urgent referral to nearest A&E
- If physical injuries and/or acute mental state not thought to be necessitate further referral to A&E then:
- Wound care
- Urgent referral to secondary metal health servcies
- Provide emotional support & help if necessary to relatives/carers of people who have self harmed
Discuss the long term management following an act of self harm
- Assess risk of self -harm and suicide at encounters
- Identify and managiing any identified psychosocial needs e.g. offering advice and support to facilitate goals such as education, employment etc…
- Management of any other mental health problems e.g. depression
- Educating patients family
- Preventing access to means of any self harm where possible e.g. considering what drugs are prescribed to them and other members of their household- consider short prescriptions
- Signposting to support services
- Referral to community mental health services or CAMHs (for children); mental health services are usually responsible for longer term management of self-harm
If a person has been admitted to hospital due to self harm, within what time frame should they have a follow up with GP?
Follow up within 48hrs
State some potential complications of self-harm
- Complications can depend on method of self harm e.g. acute liver failure if paracetamol overdose, wound infection if cutting, scarring of skin, damage to tendons & nerves
- Increased risk of suicide
Briefly discuss the Mental Capacity Act (2005), include:
- What it is
- What it allows us to do
- 5 main principles
- How we assess capacity
- Metal capacity refers to ability of a person to make a decision at a time when it is needed
- Under the mental capacity act, we are able to assess somones capacity (using a mental capacity assessment) and then, if approriate, make decisions in their best interests
- 5 main principles:
- Must assume capacity until proven otherwise
- Maximise a person’s decision making capacity
- People are free to make seemingly unwise decisions
- Any decision must be in best interests of person
- Must chose the least restrictive alternative
- To asssess capacity perform mental capacity assessment and see if pt can:
- Understand info
- Retain info
- Weigh up info
- Communicate decision
Briefly discuss the mental health act, include:
- What it allows us to do
- Criteria requierd for us to enforce mental health act
- What it allows us to do
- Mental health act allows compulsory admission of people who:
- Have a mental disorder of a nature and degree that warrants treatment in hospital AND
- Needs to be admitted in the interests of their own health or safety or for the protection of other people
- Allows us to keep people in hospital and give treatment for their mental health against their will
Mental health services are usually responsible for the longer term management and treatment of self-harm; discuss what the mangement may include
- Harm minimisation techniques (less destructive or harmful methods of self-injury e.g. rubber bands, ice cubes, marker pens, pinching etc…)
- Coping strategies e.g. relaxation techniques
- Psychological intervention e.g. CBT
- Making a crisis plan
- Keeping primary care up to date with any episodes of self-harm, info in crisis plan treatment etc…
What is a crisis plan?
Crisis plan outlines self-management strategies, contact numbes and information about what to do and whom to contact in a crisis if self-management strategies are not working


