Lecture 8 and 9 Flashcards
1
Q
Host for cooperia
A
Cattle, sheep, goats
2
Q
Location of cooperia
A
Small intestines
3
Q
Morphology of cooperia
A
- Small worms
- The cuticle of the anterior end forms a small cephalic swelling
- Bursa is large, the dorsal ray is divided into two branches which may be parallel or curved
4
Q
cooperia eggs
A
- Think shelled
- Many cells
5
Q
PPT of cooperia
A
12-17 days
6
Q
Infection of the host with cooperia
A
- Ingestion of L3 with pasture
7
Q
Where does cooperia located environmentally
A
- Cattle
- Tropical
- Subtropical costal regions
8
Q
When are eggs of cooperia detected
A
- As young as 3-4 weeks and at 8 weeks high eggs can be seen
9
Q
When is the number of cooperia large
A
- Largest number of larvae on pasture are in late summer and early autumn
10
Q
When do animals develop resistance to cooperia
A
- Calves: 6-8 months
- There is ususlaly no problem after 12 months
11
Q
Pathology of cooperia
A
- Inflammation of the mucosa and destruction of the tips of the villi; errosion of the epithelium -> seepage of fluid and albumin into the intestinal lumen -> ascities and submandibular oedema
- Profuse mucous/fibrino-nectotic exudate covers the intestinal wall becomes thick
12
Q
Clinical signs of cooperia
A
- Common in dairy and beef 2- 12 months of age
- Late summer and autumn
- Clinical signs start within 3 seeks after infestation
- Anorexia, intermitted, drofuse diarrhoea, dehydration, rapid weight loss, emaciation
13
Q

A
cooperia
14
Q

A
cooperia
15
Q

A
cooperia
16
Q
Location of bunostomum
A
Small intestine
17
Q

A
bunostomum
18
Q
A
bunostomum
19
Q
Morphology of bunostomum
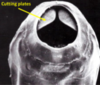
A
- Anterior end is bent dorsally
- The buccal capsule is big and bears
- Ont the dorsal margin a dorsal cone
- On the ventral margin margin a pair of cutting plates
20
Q
What do the eggs of bunostomum look like
A
- Thin shelled, morula stage
- Infestion of the host with L3
- Skin penetration
- Ingestion of pastures
21
Q

A
bunostomum
22
Q
Epidemiology of bunostomum in cattle
- Distribution
- Season
- Animal
- Calveds
A
- Distribution: summer rainfall areas of coastal QLD and northern NSW
- Season: larvae common during the warm wet season
- High prevelance in dairy cows, associated with high stocking rate and poor hygiene
- Calves develop strong resistance to reinfection -> infections are eliminated in animals older than a year
23
Q
Pathology of bunostomum
A
- Feeding: blood and plugs of the intestinal mucosa
- Intestinal mucosa becomes inflammed and thickened, with punctiform haemorrhages -> haemorrhagic enteritis
24
Q
Clinical signs of bunostomum
A
- Dairy claves 5-12 months
- Seen in autumn and winter and winter and spring
- Anaemia, weakness, anorexia, black diarrhoea, weight loss, submandibular oedema ect













