Lecture 13: Iron homeostasis Flashcards
What is the function of iron in the body?
Important in the formation of:
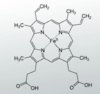
- the haem part of heamoglobin (See picture)
- Other essential elements of the body including myoglobin, cytochromes, peroxidase, catalase etc
What is the total quantity of iron in the body?
Averages 4-5 grams of iron
Which part of the body has the biggest iron stores?
Bone marrow and haemoglobin (approx 3g)
2nd is the reticulo-endothelial system (200-500mg)
3rd myoglobin (200-300mg)
4th enzymes (100mg)
List some of the essential enzymes that have an iron component?
Cytochromes
Cytochrome oxidase
Peroxidases
Xanthine oxidase
Catalases
RNA reductase
Which cells of the body take up iron?
All cells of the body
Describe haemosiderin?
- Iron-storage complex
- When the body has enough iron, when haemoglobins are broken down, and the iron is released, the body stores the excess iron in haemosiderins
- Most commonly found in macrophages
- Occurs when storage of iron in ferritin is exceeded
What is the difference between the level of iron in the serum ferritin vs iron stores?
Tiny amount of iron in serum
Large amount of iron in stores in the body
Where is the GI tract is iron absorbed?
In the small intestine from ingested foods
Describe the recycling of iron by the body?
Iron is essential in the formation of haemoglobins
RBCs have a lifespan of 120 days, after which they must get broken down by the reticulo-endothelium system.
The iron released from the break down of RBC is recycled back into the body (not lost).
What happens to iron once its absorbed by the small intestine?
Iron is immediately combined in the blood with transferrin
This complex is then transported in the plasma.
Describe transferrin?
- Glycoprotein
- Synthesised in hepatocytes i.e. the liver
- Has two iron binding domains
- Iron is loosely bound and consequently can be released to any tissue cell in the body
How is iron transported in the plasma?
Bound to transferrin
What percentage of transferrin is:
A) saturated with iron
B) free from iron
A) 30% are saturated with iron (either with 1 or 2 irons)
*remember transferrin has 2 iron binding domains so can bind to a maximum of 2*
B) 70% are free from iron
Therefore, the majority of transferrin is free from iron
What is the serum ferritin level (Therefore ferritin production) in the following situations:
A) Iron deficiency anemia
B) when levels of iron is in excess
C) Tissue inflammation
A) Decrease in iron deficiency anemia (because less iron is taken up, therefore less ferritin needed to transport it)
B) Rise when levels of iron is in excess (because you want to transport the excess iron and store in)
C) Rise in tissue inflammation
Describe ferritin production and how it gets to the small intestine to bind to iron?
** apotransferritin + iron = ferritin **
- The hepatocytes in the liver synthesis apotransferritin.
- The liver secretes the apotransferrin into the bile
- The bile flows through the bile duct into the duodenum.
- In the duodenum, the apotransferritin binds to free iron and other iron compounds, forming transferritin.
Describe how the body excretes excess iron?
No mechanism to excrete excess iron. Hence, why iron homeostasis is so important.
Little amounts of iron (1-2mg per day) are lost from the body via urine, faeces, sweat and cells sloughed from the skin and GI tract.
The amount of iron lost for males is 1mg per day while for females is 2mg per day.
Why is this?
Women lose an additional amount via menstrual blood.
*REMEMBER ERYTHROCYTES CONTAIN THE IRON IN THE HAEM COMPONENT*
The western diet is ___ in iron
Rich
around 15-20mg per day
The daily requirement is only 1-2mg per day
Not all of the iron from the diet is absorbed
Where does the majority of iron required by the body come from?
Majority comes from the body stores
Little comes from dietary sources
Give examples of rich sources of iron?
- Meat (red meat particularly)
- Liver
- Shellfish
- Egg yolk
- Beans
- Nuts
- Cereals
- Lots more
The body has a considerable store of iron. One of these stores is in the liver. Here, the excess iron is bound to___?
Ferritin
What is the rate of iron absorption in the intestines?
Extremely slow
Maximum rate of 1 or 2 mg of iron absorbed per day.
What are the two types of iron in meat?
Haem and non-haem
Compare heam and non haem iron in the diet:
Giving examples of the types of food these types of iron are found in.
Comparing the efficiency of absorption in the body?
Haem group:
- Found in red meat, chicken and fish
- Easily absorbed by the body
Non-haem group:
- Found in plant foods such as vegetables, cereals, beans and lentils.
- Not absorbed well by the body
The non-heam iron is not easily absorbed by the body.
Describe the body’s mechanism of action of non-haem iron so the iron can be abosrbed?
- Non-haem must be reduced from the ferric to the ferrous form by duodenal cytochrome B1.
- Fe3+ -> Fe2+
- The process is influenced by vitamin C
- Duodenal cytochrome B1 activity increases when vitamin C is present
Give a basic step by step approach to iron absorption?
- Once iron is reduced into Fe2+ it is taken into enterocytes via divalent metal transporter 1 (DMT1).
- Once in the enterocyte, it joins the labile iron pool.
- The labile iron pool serves the processes ofthe cell itself e.g. mitochondria.
- However the labile iron pool is small therefore the majority of the iron is incorporated into ferritin, which functions as an intracellular iron store.
- The iron from the labile iron pool can also be released to the plasma bound to transferrin.

Most of the iron is incorporated into ___, a protein-iron complex that functions as an intracellular iron store
Ferritin
Iron circulates throughout the body bound to ____, a plasma protein?
transferrin
Describe what happens to the iron when erythrocytes are broken down?
Erythrocytes are broken down by macrophages in the reticulo-endothelial system.
If the body has plenty of iron then these macrophages store the iron as ferritin.
The iron gets released from these reticulo-endothelial system macropages to the plasma in response to ferroportin and hepcidin.
How much iron is stored by the reticulo-endothelial system?
Around 500mg of iron is stored by the RE system macrophages
Which cells of the body have ferritin receptors?
All cells of the body
Therefore all cells can store iron
Ferritin binds to iron where?
Transferrin binds to iron where?
Ferritin: in the cell as an intracellular iron store.
Transferrin: bound in the circulation
Transferrin is synthesised in the?
Liver
Iron released from the __ and ___ is transported in the circulation by the plasma protein ___?
- Enterocyte
- Reticulo-endothelial system macrophages
- Transferrin
How many iron atoms can each transferrin molecule bind?
2
How is iron delivered to tissues?
The transferrin-iron complex binds to transferrin receptors on the cell surface.
The higher the concentration of transferrin receptors the more iron it takes up. Found particularly on red blood cell precursors
Describe the process of iron being turned into haem?
- Iron is in plasma bound to transferrin.
- Transferrin receptors on the erythroblast surface takes the iron from the iron-transferrin complex.
- The iron is transported to the mitochondria where it is used to produce haem.
- Excess iron is stored in ferritin as an intracellular iron store
- Process is complete within minutes
Describe the following image?

- Iron is absorbed in enterocytes in the GI
- The iron is excreted by enterocytes into the circulating plasma.
- The iron is bound to transferrin.
- The iron is taken to be stored and/or used in other tissues
- e.g. Bone marrow, myoglobin, enzymes.
- In tissues such as joints, heart etc.
- The bone marrow forms erythrocytes (which has an iron component)
- The erythrocytes after 120 days are degraded by the reticulo-endothelial system.
- The iron is released and stored by the RE system macrophages.
- The iron can be released by these macrophages back into the plasma bound to transferrin.
- Iron is lost by the loss of cells in the GI and by menstrual loss.
Define ferroportin and what is its function?
- Transmembrane protein
- Function is to transport iron from the cell to the plasma.
- The only iron exporter.
Ferroportin is regulated by?
Hepcidin
The interaction between ___ and ___ controls systemic iron homeostasis?
Hepcidin and Ferroportin
Where is ferroportin located?
Ferroportin is found on the basolateral membranes of intestinal epithelia
I.e. in the cell surface of enterocytes, macrophages and hepatocytes
Define hepcidin and its function in iron homeostasis?
- Hepcidin is a peptide hormone produced by the liver and secreted into the circulation.
- It is a regulator of the iron metabolism.
- Hepcidin directly binds to ferroportin
- After binding, ferroportin was internalized and degraded
- Therefore reducing its functional activity
- Leading to a decrease in iron cellular export in the enterocytes and macrophages
Describe iron deficiency anaemia?
- Common form of anaemia
- Caused by a lack of iron, usually when iron is getting lost or when iron demand is too much.
- Most common cause is blood loss or could be due to chronic PPI use.
- RBC configuration: microcystic hypochromic (pale and small)
- Hypochromic: the RBC appear paler due to low levels of haemoglobin (outside ring is thin- as this is the haem part)
- Microcystic: appears smaller

What is the golden rule in regards to iron deficiency anaemia in males and postmenopausal females?
The cause of the iron deficiency anaemia is due to GI blood loss until proven otherwise
What is the golden rule in regards to iron deficiency anaemia in young women?
Due to menstrual blood loss or/and pregnancy.
GI blood loss is only investigated if the patient has GI symptoms or blood in stool.
Complete opposite to males and post menopausal females
Where is iron absorbed in the gi tract?
The duodenum is the chief area where iron absorption takes place
Why is coeliac disease commonly associated with iron malabsorption?
In coeliac disease, the mucosa is characterised by villus atrophy, enlarged hyperplastic crypts and inflitration of inflammatory cells into the lumen.
This impairs the ability of the enterocytes to absorb iron
What are the most likely haematinic deficiency in coeliac disease?
Most likely: folate deficiency
2nd most likely: iron deficiency
Unlikely: Vitamin B12 deficiency
What happens to the incoming iron when the iron levels in the blood is plentiful?
- The increased concentration of free iron in the plasma and intestinal epithelial cells leads to an increased transcription of the gene encoding the ferritin protein
- Leads to an icnreased synthesis of ferritin.
- Leads to increased binding of iron in the intestinal epithelial cells
- Reduced amount of iron released into the blood
What happens to the incoming iron when the iron levels in the blood is scarce?
- The reduced concentration of free iron in the plasma and intestinal epithelial cells leads to a decrease in the trnascription of the gene encoding the ferritin protein.
- Reduction in synthesis of ferritin.
- Leads to a decrease in the amount of iron bound to ferritin
- Thereby, increasing the unbound iron released into the blood
The control mechanisms for iron absorption tend to maintain the iron content in a narrow haemostatic range. A very large ingestion of iron can overwhelm them. What does this lead to?
Leads to an increased deposition of iron in tissues
This can produce toxic effects such as changes to the skin pigmentation, diabetes mellitus, liver failure, heart failure etc
Describe the mechanism behind hereditary haemochromatosis?
- An autosomal recessive disorder of iron metabolism causing iron overload
- Caused majority of the time by abnormalities in the HFE gene
- HFE gene is required for the synthesis of hepcidin.
- Therefore in HH there is a reduction in hepcidin production.
- Therefore, there is no mechanism to limit ferroportin (a protein used for the export of iron from enterocytes and macrophages into the plasma)
- Results in iron overload
- The transferrin can bind to iron, but with a high concentration of iron there are high transferrin saturation and leading to some iron not being bound (non-transferrin bound iron). This free iron can cause tissue damage
Fill in the table for the labatory findings for iron deficiency anaemia and hereditary haemochromatosis?


Describe haemochromatosis?
Condition in which extra iron is absorbed by the GI, which increases the iron levels slowly builds up in the body over multiple years.
For example, extra intake of 3mg per day. Over 18 years that will be an excess of 20g of iron (remember the iron stores in the body at any time is 4g)
This excess iron is bound to transferrin.
Eventually the transferrin become saturated, leading to unbound iron, which can cause damage to tissues.
Excess iron can damage other tissues. What is the effect in the following tissues:
A) Liver
B) Pancreas
C) Skin
D) Joints
A) Can cause cirrhosis of the liver.
B) Damage to pancreas can lead to diabetes mellius
C) Bronzing of the skin (as iron stimulates melanin production)
D) Arthritis of the joints
Describe the epidemiology of haemochromatosis?
Haemochromatosis most often affects people of white northern European background and is particularly common in countries where lots of people have a Celtic background, such as Ireland, Scotland and Wales.
What are the possible treatments of haemochromatosis?
- phlebotomy – frequent blood if withdrawn, which removes iron contained in erythrocytes from the body.
- chelation therapy – medication to reduce the amount of iron in your body; this is only used if it’s not easy to regularly remove some of your blood


