Le Grice: Regulation of Cardiac Function 2 Flashcards
You don’t need nerves to make the heart beat, but you do need them to ________.
You don’t need nerves to make the heart beat , but you do need them to control that beating.
Sympathetic: Top 3 cervical ganglion; Superior, middle and stellate (inferior and T1) cervical ganglion’
PS: Vagal nerve
Homogeneous distribution of SNS to the AV node, SA node and ventricles.
Overview of SNS impacting on heart rate
- Increased Heart rate: takes around 30 seconds to respond to a change in SNS stimulation (w a latency of 1-3s)
- Duration of the cardiac AP is reduced by both PSNS and SNS
- Acceleration of impulse propagation through the AV node
- May also facilitate pacemaker ability of cells in the AV node
Effect of SNS of contractility
Causes an increased inotropic state and the heart beats much more vigorously

Where is there a differing of effect between the left and right sides of the heart?
- Stimulating the left stellate ganglion has no effect of HR whereas stimulating the right stellate ganglion does.
- The right side of the SNS has an effect on the SA node. However, when looking at blood pressure (and therefore inotropic state), it is the left side that has more of an effect
Therefore we would conclude that on the left most of the Sympathetic nerves head to the Ventricles where as on the right they head to the Atria.
Parasympathetic activation, and where it acts in the heart.
Mainly the vagus nerve (CN X) acting mainly on the base of the left atrium. Here there is a large plexus of nerves that spread out, these fibers talk to and inhibit each other.
Ablation therapy is often in the post-LA, and some believe by burning this area, you are not only removing the fibrosis developing but the ANS involvement that can cause atrial fibrillation
Effect of Parasympathetic activity (via M1 acting to stimulate Gi)
- Reduced HR: the response is rapid in comparison to the SNS
- AP duration in the atrium is reduced
- Deceleration of impulse propagation through the AV node
- Cardiac Vagus stimulation decreases the inotropic state of the atria
- effects on ventricular inotropic state much less, reflecting sparse PNS innervation of the ventricles
In the short term, what determines a change of HR?
The parasympathetic nervous system
- Sympathetic blocker: propanolol
- Parasympathetic blocker: atropine
- Our normal heart rate without the ANS would be sitting at 100 bpm, but as we sit at 60 bpm, at tonic levels we are being regulated by SNS/PNS to keep the HR at a certain level
- The main controller of this is the PNS (diagram shows that blocking of PNS with atropine shows the largest change)

What happens if we increase vagal input to the heart?
As we increase vagal input to the heart there is very little SNS input acting as a control/. HR drops dramatically with increased PNS input in the short term

How is the cardiac HR reaction time different for PNS and SNS
PNS: vagal stimulation and then removal leads to a rapid drop and then increase in HR
- breathing
SNS: stimulation leads to a slow increase over 30s that then is maintained over some time even upon stimulus removal, slowing dropping back to the norm. Therefore it cannot change HR quick enough to have an effect on breathing

Why is it that the PNS and the SNS stimulate HR at different times
SNS: the release of adrenaline leads to many complex downstream processes that eventually leads to increased HR. ALSO To switch off the SNS, the adrenaline needs to be re-uptaken into neurons, which is a very slow process. Important for intermediate effects
PNS: switches on the Muscarinic receptor, activates Gi protein and immediately open a K+ channel. There is no 2nd or 3rd messengers, but there’s a straight response. AChE mops up the ACh straight away.
Oxygen demand is determined by….

- Basal metabolism: things keeping cells alive
- Wall force development: during contraction, development of wall force is dependent on stress/pressure (pressure x time) and geometry (LaPlace)
- Inotropic state
- Heart Rate
Oxygen supply is determined by
- Perfusion pressure determined by aortic pressure and extravascular compression
- impedance (resistance)
- MVO2 = Q* (CaO2-CvO2)
- Flow rate x delivery
- Increase O2 conc hard to do
- increase O2 extraction: not much there (normally 75%)
- Increase blood flow ***

There is one capillary per cardiac muscle cell, which means…
ALL the oxygen pretty much gets extracted in cardiac cells.
Why it can’t extract more when under ischaemic stress
Flow in the L/R coronary artery changes
Why does most of the blood flow occurs during diastole??
Most of the blood flow occurs during diastole because when the muscle cells contract the blood vessels they surround get fucked up and resistance gets really high. During systole, blood flow drops right down. Normally think driving pressure (at aortic root) minus pressure at the other end (potentially coronary sinus). But actually due to this compression, the coronary sinus pressure is irrelevant, and its the pressure in the Ventricular lumen. in systole these are equal.
Therefore higher HR causes a problem as a this means there more work done BUT smaller diastolic time, and why people get angina during exercise

Local control of coronary resistance is?
Always lots of cardiac local regulation.
Flow = pressure gradient / resistance
if we change resistance we can alter flow. These changes eg; vasodilators can be produced in the heart. Will work great unless there’s an upstream blockage eg; athrosclerosis
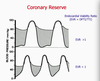
What does this diagram represent?

Shaded area: the difference in pressure between L.ventricular vs aortic / time = SUPPLY
Not-shaded: how much demand there is DEMAND
- Want these areas to be similar!! In a healthy* heart the supply is greater than demand.
- If there is not enough supply or increased demand (as shown below) you can get ischaemic and infarction)*