Kolbe: Respiratory Pathophysiology 2 Flashcards
Scenario. A 74 year old year woman presents to the Emergency Department with worsening shortness of breath. She is well known to the Department , needing hospital admissions on 2 to 3 occasions per year. She says that she is always short of breath and has difficulty getting to the shops but things are currently much worse than usual. There has been an increase in her daily sputum production.She had smoked 20cigs/d for 40 years. Her daughter called the ambulance because of worsening shortness of breath; she is breathless at rest. (When you see her in the ED she is wearing an oxygen mask and is drowsy and confused.)
What will the arterial blood gases show?
What patho-physiologic mechanisms were involved?
Describe what COPD is
Chronic Obstructive Pulmonary disease (COPD) is a disease state characterized by airflow limitation that is not fully reversible. The airflow limitation is usually both progressive and associated with an abnormal inflammatory response of the lungs to noxious particles or gases.
- Cigarette smoking is the primary cause (also burning of biomass)
- 4th leading cause of death in USA
- 2.74 mill worldwide
- Has a huge burden of disease
- Our FEV (lung function) starts to decline at 25 yrs
- People are impacted by smoking differently
- If you stop smoking this decline eases but doesn’t get better

COPD can be thought of as three different components. What are these are how does this vary?
- Chronic mucus hypersecretion
- hyperplasia of goblet cells and hypertrophy of mucus glands → more mucus → a productive chronic cough (not airflow obstruction)
- Emphysema
- destruction of alveolar walls by proteases in response to a toxic agent (smoking) -causes airflow obstruction
- Small airway inflammation (and obstruction)
- along with emphysema, causes airflow obstruction!
These components vary in different patients
Explain the 3 compartment model of the Lungs
in reality there are 1000’s of compartments that all lie between 00-1
V/Q = 00 infinity (dead space)
- Ventilated but not perfused
V/Q = 1 ( ‘Ideal’)
- Ventilated and perfused
V/Q = 0 (Shunt)
- Perfused and not ventilated: a venous mixture, where venous blood is being mixed with oxygenated blood to form a mixture
- Shunt is an anatomical abnormality when the blood doesn’t get into the alveolus

COPD is a major cause is V/Q mismatch.
This is a major cause of hypoxaemia, explain how using the 3 compartment model of the Lungs

- Until the age of 25, we can assume they had a perfect (V/Q= 1 ‘I’) middle compartment lung
- As they smoked they began to get more and more between the right-sided (V/Q = 0 ‘II’) lungs and the perfect lungs (between 0-100% function)
- They are also getting more left-sided (V/Q = 00) dead saces but these do not contribute to the arteriole blood gases = wasted ventilation. We are only interested in compartments with a V/Q between 0-1.
- If we look at the content of blood in compartment ‘I’ (vent and perf.) in comparison to compartment ‘II’ (Perf. but not vent) and then mix them….
- in response to hypercapnia, we will increase our alveolar ventilation, as our resp center is very sensitive (also very sensitive to the H+ ions from the resulting acidosis). We will only respond to hypoxemia when we are severely hypoxemic (<80%). SO we hyperventilate and normalise our CO2 and our O2 will remain low, because the only compartment you can HV is the normal ‘I’ one!!

use the CO2 and PO2 content curves to describe how hyperventilation doesn’t always improve hypoxemia, but it can improve hypercapnia

In a normal (V/Q = 1) compartment, we are already at a high point of out PAO2 sigmoidal curve. By hyperventilating, we don’t improve the saturation of blood being perfused very much.
The PCO2 curve is a very different shape. By hyperventilating and decreasing our P ACO2 we can produce a big difference in CO2 content.
Eventually through hyperventilation and metabolic compensation you have
- Decreased PaO2
- Normal PaCO2
- Normal pH
H2O + CO2 >< H+ + HCO3-

Although you are able to compensate for temporary hypercapnia, what happens if the patient continues to smoke
Even though you blow off the CO2 for a period of time, if she continues to smoke, she will have a worse V/Q to the point where she can no longer maintain the level of hyperventilation and her CO2 will climb, (and she’ll reset her chemoreceptors!)
Although the body can handle temporary hypercapnia and adjust, it cannot handle acidosis! The H+ is excreted in the kidneys and the elevated CO2 is reflected in the raised blood HCO3- (compensated chronic respiratory acidosis, her respiratory center is now not very response to CO2 , and you are dependent on your hypoxic drive. This is susceptible to being turned off from high inspired O2 (ventilated O2)
Now ‘acute onchronic respiratory acidodic’

How can we know from these levels that the woman is breathing supplemental O2
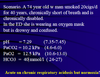
A-a gradient of someone breathing room air = 20 - PaCO2/0.8 - PaO2
and has to be >0 (otherwise O2 would be going reverse)
so PaCO2 / 0.8 + PaO2 < 20
if its not, then we know she’s been breathing supplemented O2
10.2 / 0.8 + 12.5 = 25.25 (way over 20!)
- Her PaO2 has been returned to normal with the mask and so we have stopped her hypoxic drive letting her PaCO2 rise
- Leaving her with acute on chronic respiratory acidosis

Describe Shunts
- Can occur at the cardiac level and go R-L instead of L-R!!
- Can occur within the lung due to abnormal vessels: arteriovenous malformations
Why does she have a ‘high’ red colouring

Excessive production of Erythropoietin from the kidneys due to hypoxemia.
Leads to an excessive of RBC and Hb.
She is Polycythemic.
A shunt is suspected
How do you distinguish a shunt from a V/Q mismatch?
- Administer 100% O2 if it’s an isolated drop of PaO2
- If you increase inspired O2 to 100%, then there will be an increase to around 600/650mmHg = 80/86 kPa
- Even if there’s worsening V/Q mismatch, they will still eventually be able to reach 600mmHg
- HOWEVER in a R→L shunt, as the anatomical shunt worsens you don’t get anywhere near 600mmHg.
- Note that even though they may only get up to 200mmHg, at this level the blood will still be saturated. THis is why we should test the Pa O2 not just the oxygen saturation (finger clips, give an undefined measure of color)



