Le Grice: Cardiac Rhythm Flashcards
What are the steps of ‘Normal’ sinus rhythm of the heart that allows for efficient contraction?
- Activation begins with spontaneous depolarization of cells in the SA node
- suppresses other slower pacemakers
- spreads across atrial chambers
- enters the AV node (slows a → v activation)
- Propagates rapidly along interventricular septum and across ventricular surface vis HIs-Purkinje system
- allows for coordinated wave from endo →epicardial surface from apex to base of the ventricles
- existence of a prolonged refractory period in the myocardium, allow synchronous contraction

What three things maintain sinus rhythm
- Entrainment and suppression of lower pacemakers
- SA drives other pacemakers (AV node) because it has the fastest spontaneous rate. this entrainment suppresses the others inherent automaticity.
- Due to overdrive suppression, the AV node pacemaker may not take over
immediately is SA node is blocked suddenly ‘sick sinus syndrome’
- Coordinated excitation via specialised conduction system
- Existence of a prolonged refractory period in the myocardium
- this is a big area of drug therapy
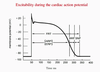
- ARP: time where cannot stimulate the cell (ERP cannot restimulate groups of cells)
- RRP -relative (need larger) and SNP -supranormal (can be smaller): can stimulate AP but they are never normal, are always smaller, slower upstroke and propagate slower.
How would you describe arrhythmia? (two distinct ways)
any deviation from sinus rhythm
- Disorders of impulse formation: early discharge of a pacemaker (abnormal automaticity) or activity triggered by an unstable resting membrane potential (not SA node) in working myocardial cells (DAD, EAD). These give rise to extrasystoles. (ectopic beats require a region of cells to be abnormal not just one)
- Disorders of impulse conduction: conduction abnormalities such as a partial or complete AV block, left or right bundle branch block and re-entry. The first gives rise to slowed HR/bradycardia. the others alter the time-course of the ventricular activation sequence. Conduction abnormalities may arise bc of spatial or temporal dispersion of repolarisation - very dangerous
what would happen if you stimulated the heart here?

Some cells will be completely repolarised, some cells won’t, and you’ll get a big mismatch of some activated and some not in this RRP.
As this is where the T wave is, which is called the ‘Vulnerable window” as you are at high risk of developing an arrhythmia.
A stimulus in the T wave can initiate ventricular tachycardia which can then → Ventricular fibrillation.
activation is reentering around the ventricles disregarding the SA node

Types of reentrant arrhyhmia?
- Atrial flutter: fast regular atrial rate (250-300 b/m) heart block may develop)
- Atrial fibrillation: rapid disorganised atrial activation (350-600b/m) not all impulses conducted to ventricles. rapid disorganised ventricular rhythm. Risk of embolization.
- Ventricular tachycardia: rapid ventricular activation (110-250 b/m) impaired mechanical function and risk of VF
- Ventricular Fibrillation: chaotic ventricular rhythm leads to circulatory arrest and death
Describe atrial flutter
Fast regular atrial rate (250-300 b/m) . Heart block may develop.

independent of SA node.
Bump = flutter wave (not normal p wave)
Every now again you get enough to get through to the ventricles, then another 3 ‘atrial flutters’
Describe atrial Fibrillation
rapid disorganised atrial activation (350-600b/m) not all impulses conducted to ventricles. rapid disorganised ventricular rhythm. Risk of embolization.
- very disorganised baseline and then every now and then an irregular pulse from ventricles.
- and “irregularly irregular’ pulse
- this is often not diagnosed by practitioners and can lead to stroke or death if untreated.

Describe Ventricular Tachycardia
rapid ventricular activation (110-250 b/m) impaired mechanical function and risk of VF.
coordinated contraction and coordinated activation, people collapse because the pumping may not be as good.
Very rapid, wide QRS.

describe ventricular fibrillation
chaotic ventricular rhythm leads to circulatory arrest and death
in order to understand drug therapy you need to understand ionic cardiac currents.
- Upstroke: fast Na+ current and some Ca current
- a 3Na/Ca exchange pulls calcium into the cell early on (an outward going current as 3Na are leaving), then later it is used to push them out, is electrogenic
- K+ turns on/off throughout the AP
- Remember repol is due to the delayed rectifier currents IKr and IKs which take a while to switch on after upstroke
drug treatment deals with these currents and either blocks**/stimulates to conduct differently, what may affect a cell one way will affect another cell completely differently

Describe the fast working sodium current?
Switches on and switches off vw

Describe the fast Na channel
activates an inactivates really quickly.
@rest: inactivation gate open, activation gate closed
@AP: swaps over rapidly
small but enough to give us the depolarization. In order to do this again, the gates need time to get back to the levels at rest.
You can have gates at different levels of getting back to normal (this is what determines the RRP and SRP)

When can a heart block become a problem?
Usually if there is a ‘block’ or a region of tissue that cannot be activated electrically, the current will go around, collide, and carry on to activate the ventricles.
- Issues occur when: for some reason, activation doesn’t spread down it is blocked in one direction ‘unidirectional block’. it has the potential to go around and around and around. In order for this to occur….
- enough time for cells to reset. If they go to rapidly they cannot establish reentrant circuit
- Length of the refractory period; if really long its unlikely it will have enough time to produce the circuit

Re-entrant activation requires

- a circuit
- slow conduction and/or short ERP (effective RF refers to group of cells)
- unidirectional block
- a trigger
Reentrant circuits can be anatomic or function.
Slow conduction and unidirectional block occur when repol is not spatially homogeneous. eg: wolf-Parkinson white syndrome, where theres extra tissue other then the AV node that can allow ventricular activation

Whats the issue of AF in those with WPW?

As the AV node usually protects us from Atrial flutter rapid stimulation by slowing down activation. The extra tissue in those with WPW syndrome doesn’t have those properties, so if they also have atrial flutter then there is no control mechanism.
Rate of propagation of electrical activation determined by?
- Electrical properties of myocytes
- increased electrical coupling between myocytes increases propagation rate
- propagation rate is greatest in larger diameter cells
- Inward current during excitation
- density and status of Na channels is important here- greater current = faster propagation (CF refractoriness)
- this is why SAN uses Ca channels as these are much slower than Na

If you have an ectopic beat, what is the potential for reentry?
If ectopic activation occurs during vulnerable period (T wave)
- Sodium channels not fully reset so reduced sodium current
- slower propagation → chance of reentry
- Repolarisation non-uniform
- greater probability of local conduction block
Myocardial Ischaemia is a potential for an arrhythmia because??
- It results in
- slow conduction
- reduced AP duration
- Non-uniform repolarisation
- Ectopic activations (DADs)
- When people have a heart attack and die on the spot it is due to VF.

SloSlow conduction in myocardial iscahemia is due to??
- Low ATP
- Na/K ATPase reduce
- Transmembrane Na, K gradients reduced
- partial membrane depolarization
- inactivation of sodium channels, inact. gate already partially closed
- reduced gap junction coupling (low pH due to regional metabolic acidosis)
- reduced Na current → reduced rate of spread

Actional potential changes in myocardial ischaemia are due to?
Na/K ATPase reduced - [Na]i and [k]o increased
Transmembrane K gradient reduced (external K increased)
INa reduced
- Hyperkalemia shortens AP duration (increased [K+]o increases IKr as it is [k]o dependent )
- Reduced [ATP]i activates IKATP channels, shortens AP duration
- In the ischaemic regions- inhomogenous electrical properties

DADs in Myocardial ischaemia
Because the pumps aren’t working well you cant pump Ca out as well as you should, excess Ca in SR, when it reaches a threshold it automatically releases calcium without electrical stimulation.
This causes Na/Ca exchanger starts working, forms a current and you’ll get a little depolarisation.
If this reaches threshold, you have an ectopic beat!

Why does VT turn into VF
If VT develops - eg. acute ischaemic event
- +ve feedback
- rapid rate, poor contraction
- Increased O2 demand, reduced O2 supply
- ischaemia more severe
Leads to VF!!
Why do you get more ectopics with a healed MI
- infarct “border zone” complex: a mess of good and bad tissue
- structural heterogeneity
- substrate for abnormal electrical activity and reentry
- Often monomorphic VT(looks the same every beat); stabilised by structure
- Some treatment is to burn this border zone
Why do you get more ectopics with Heart failure
- A/V become fibrosed over time; slower conduction
- Atria dilated > promotes larger path lengths for reentry
- Inc. atrial pressure; stimulates stretch-activated ion channels
- altered expression of ion channels
- ANS remodels; PS and S rebalances
- once you start getting AF it sets up properties to have more AF

Describe long QT syndrome

A prolonged AP.
- these prolonged APs can enable ICa(L) to reactivate → can lead to EAD (Early After Depolarisations)
- these Ca channels usually open/close and reset themselves for the next AP, but if the AP is long enough they can be reset within the AP and cause it to be even longer! but if you use drugs to lengthen AP that can lead to an arrhythmia!!
- Increased AP duration may be due to
- drugs; (amiodarone anti-arhythmic)
- Reduced ExC potassium concentration (hypokalaemia; decrease [K+]o → decreased IKr : LQT1 IKs and LQT2 IKr
- K ion channel mutations which lead to reduced effectiveness of delayed rectifier IK :LQT1 = [Iks] and LQT2 = [Ikr]
- sodium channel mutations that affect inactivation of INa =(LQT3)
EADs can result in ______
torsade de Pointes: twisting of the points
may resolve sponatneously
continuously varying polymorphic VT
Long QT syndrome that is drifting around in the heart



