Dawes: Alpha Blockers and Calcium Channel Blockers Flashcards
(32 cards)
What are the function of alpha blockers and calcium channel blockers?
- A receptor blockers: antagonize post-synaptic alpha receptors to mediate the BP lowering effect
- Ca 2+ Channel Blockers: block voltage-operated Ca channels throughout the CV tree with a number of indications
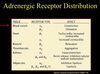
What is the function of alpha-1 receptors?
These are all post-synaptic and result in vasoconstriction of the veins and arterioles, thus producing an increase in blood pressure.
Where are alpha-1 receptors found?
- Alpha-1 a = Prostate smooth muscles
- Alpha-1 b = Vascular Smooth Muscle (These increase with age)
What is the function of Alpha-2 receptors?
These are both pre and post-synaptic receptors that inhibit the release of norepinephrine and insulin.
What are the effects of alpha 1 antagonism?
This results in vasodilation and hypotension. These include drugs such as…
- Doxazosin, Prazosin, Terazosin
- Tamulosin is an alpha-1 A specific blocker and therefore targets those receptors found in the prostate (but no BP lowering)
What are the effects of alpha 2 antagonism?
Increased norepinephrine release this is caused by yohimbine. (not used clinically)
What is an example of a combine alpha-1 and aplha-2 antagonist?
Phenoxybenzamine
When is an alpha blocker used?
- 3rd line if the patient is suffering from essential hypertension - used in combination with an ACEi and diuretic.
- May be used in the treatment of pheochromocytoma which is a tumour of the SNS classically in the adrenal glands (rare)
- Used in the treatment of prostatism - people have poor stream, dribbling, hard to start
What are the effects of doxazosin?
This is a reversible alpha blocker that has a far greater affinity for alpha-1 receptors. It blocks all alpha-1 receptors and therefore is a vasodilator that blocks the tonic sympathetic activity on resistance vessels and is used in the treatment of prostatism.
How is doxazosin administered?
Doxazosin is taken orally once daily. At first, a low dose needs to be taken and slowly increased with titration.
What are the pharmacokinetics and pharmacodynamics of doxazosin?
It has a peak plasma concentration 2-3 hours after administration. It displays linear kinetics and has first-pass hepatic metabolism which greatly reduces its bioavailability.
It is eliminated mainly by the faecal route and has a high protein binding percentage and therefore is eliminated with a half-life of 22 hours.
What are the pharmacokinetics of prazosin?
It is taken orally and undergoes first pass metabolism. As a result, it has a half-life of 3-4 hours and needs to be given twice daily.
What are the pharmacokinetics of terazosin?
It is taken orally and undergoes little first pass metabolism. As a result, it only needs to be taken once daily and has a half-life of 12 hours.
What are the adverse effects of alpha blockers?
- They cause (orthostatic) hypotension which manifests as dizziness and therefore can give the first dose at night to manage prostate symptoms.
- Lassitude
- Nasal Stuffiness
- Dry Mouth
- Urinary Incontinence (in Women)
Why is phenoxybenzamine rarely used?
It is irreversible and causes postural hypotension, tachycardia, nasal stuffiness and CNS problems.
It is used pre-operatively or to treat phaeochromocytoma as it also acts as H1, ACh and 5HT antagonist.
Why is phentolamine rarely used?
It is poorly absorbed and needs to be given via iv. It caused cardiac and GI side effects and it acts to increase norepinephrine release as it has competitive antagonism with both alpha-1 and alpha-2 receptors. It also acts as a 5HT antagonist and a muscarinic, H1 and H2 agonist.
When is labetalol used?
Labetalol is a combined alpha and beta blocker used in the treatment of hypertension in pregnancy as it is a reversible antagonist that has a greater affinity for beta receptors than alpha receptors.
When is carvedilol used?
Carvedilol has a greater affinity for beta receptors than alpha receptors and as a result, is used in the treatment of congestive heart failure. It also has anti-oxidant properties.
When is tamsulosin used?
Tamsulosin is specific for alpha-1 a and alpha-1 d receptors and as a result, is used to treat prostatism. This is because it acts to relax the bladder and prostate smooth muscle and has NO effect on BP.
This orally administered drug has a long half-life and functions as a competitive antagonist.
When is a calcium channel blocker used?
- Hypertension -(vasodilation)
- Angina -(dec. cardiac work, vasodilation)
- Arrhythmias -(supraventricular tachycyarrhythmias eg. AF)
- Vasospasm -
What is the mechanism of a calcium channel blocker?
Calcium channel blockers act by blocking voltage-operated L-type Ca2+ channels with some selectivity: present in the resistance vessels, myocardium and conducting tissue.

What is the effect of a L-type calcium channel clocker on vascular smooth muscle?
- Decreased Arteriolar Smooth Muscle Tone
- Decreased Peripheral Vascular Resistance
- Decreased Blood Pressure and Afterload
- also: other smooth muscle eg. biliary tree, uterus, bowel
What is the effect of a L-type calcium channel blocker on cardiac cells?
- Decreased contractility
- Decreased Sinus Node Rate and AV Node Transmission
What drugs fall under the dihydropyridine classification? What do they target?
- Nifedipine
- Felodipine
- Amlodipine
These target resistance vessels with almost no heart effect so lowering BP is its function for Hypertension or combatting vasospasm and therefore cause flushing, headaches and peripheral oedema (that is resistant to diuretics).


