Histology of Male Reproductive System Flashcards
Which ducts move sperm from the testes out of the body?
- Efferent ductules
- Epididymis
- Vas deferens
- Ejaculatory duct
- Urethra
Which exocrine glands secrete fluids into the ducts and add to the sperm to make semen?
- Seminal vesicles
- Prostate gland
- Bulbourethral (Cowper’s) gland
What type of epithelium makes up the seminiferous tubules?
Simple columnar epithelium of Sertoli cells
Testes are derived from __________.
Intermediate mesoderm
NOTE: This occurs via the surface gonadal ridge. Testes then descend into the scrotum
The epididymis is derived from the ________.
Mesonephric duct

Primordial germ cells migrate into the testis from the _______.
Yolk sac
__________ (warmer/cooler) blood in testicular artery. ________ (warmer/cooler) blood in pampiniform plexus.
Warmer; cooler
NOTE: The pampiniform plexus also plays a role in the temperature regulation of the testes. It acts as a countercurrent heat exchanger, cooling blood in adjacent arteries.
Label


Label


The functional unit of spermatogenesis is the __________.
Seminiferous tubule
Label


Blood-testes barrier
Weismann Barrier
The strict distinction between the “immortal” germ cell lineages producing gametes and “disposable” somatic cells

Label


Label


Spermatogonia divide via _________ (mitosis/meoisis). Spermatocytes divide via _________ (mitosis/meoisis).
Mitosis; meoisis
NOTE: Gwem cells remain conencted via intracellular bridges as they complete cell division and migrate upwards
Cell type summary

Label


Label

- The primary spermatocytes undergo Meiosis I and divide into two daughter cells, known as secondary spermatocytes, a process which takes 24 days to complete.
- Each secondary spermatocyte will form two spermatids after Meiosis II.

Spermatogenesis

In spermiogenesis, hapoid spermatids become converted into _________.
Mature Spermatozoa

Acrosome formation
Vesicles move from the Golgi stack and adhere to one pole of the nucleus to fuse into a large acrosomal vesicle
NOTE: Acrosome contains hydrolytic enzymes that will later aid in fertilation of an oocyte

What happens to the nucleus of the sperm as it becomes more developed? How is this achieved
The nucleus becomes very small. It is achieved by removing histone proteins from nucleosomes and replacing them with a smaller peptide, protamine

Aside from the removal of histone, how else is change in the nucleus of sperm changed?
The nucleus passes through a narrow perinuclear ring. The perinuclear ring moves along parallel rows o microtubules comprising the “manchette”
_____________ form the center of the flagellum.
Centrioles
Which cell is the main structural cell of the semineferous tubule?
Sertoli cell
Components of sertoli cells
- Irregular eucromatic nuclei with prominent nucleoli
- Numerous tight junctions
Functions of sertoli cells
- Tight junctions maintain a blood-testis barrier
- Secrete sulfated glycoproteins (clusterin) that transport lipids to germ cells
- Secrete androgen binding protein
- Secrete transferrin
- Secrete inhibin, a TGF-b molecule that inhibits FSH secretion
- Take up glucose from the bloodstream, metabolize it to lactate, and export lactate to germ cells as a nutrient fuel
- Respond to FSH by stimulating the development of germ cells

Structure of Leydig cells
- Mitochondria with tubular cristae
- Abundant sER
- Round, eucromatic nuclei
NOTE: Leydig cells may also possess cytoplasmic crystals of Reinke, composed of an uncharacterized protein aggregate

Function of leydig cells
Myoid cells (image)

What epithelium makes up the rete testis?
Simple cuboidal epithelium

What accounts for the irregular lumen of efferent ductules?
- Non-ciliated cells
- Tall ciliated cells
The _________ is an anastomosing network of channels located in the testicular hilum, that receives the luminal contents of seminiferous tubules and empties them into the efferent ductules.
Rete testis

Label


Components of epididymis
- Tall principial cells
- Long microvilli (stereocilia)
- Basal cells
Label


Functions of epididymis
- Absorb water from seminal fluid and secrete chloride
- Stores spermatozoa
- Secretes proteins that block the receptors on the plasma membrane of sperm head which renders sperm infertile inside the male tract
NOTE: In cystic fibrosis, epididymis becomes blocked or fails to develop, causing sterility
The _____ propels ehaculated sperm from the epididymis toward the urethra.
Vas deferens
NOTE: Large amounts of smooth muscle are present in the wall of the vas deferens

Sperm and seminal fluid mix in the __________and move towards the urethra.
ejaculatory duct
Label


What type of epithelium is found in secretory acini of the prostate gland?
Pseudostratified columnar epithelium
NOTE: The secretory acini also contain loose connective tissue and smooth muscle.
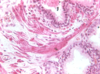
Label


Label

NOTE: Condensed, calcified secretory material is defining feature of histology of the prostate gland

Label


Epithelium of prostate gland
- Transitional epithelium in upper part
- Stratified columnar in the lower parts
Functions of prostate gland
- Secretes proteins that help maintain fluidity of semen
*
Bulbourethral gland

Label


Indictor of prostate carcinoma
- Prostate specific antigen (a serine protease
Which component of the penis is being described below?
Paired erectile bodies dorsal to the urethra which are responsible for erection.
Corpora cavernosa
Which component of the penis is being described below?
Surrounds the urethra and prevents the collapse of the urethra during erection.
Corpus spongiosum
The propulsion of semen from the male duct system is coordinated by a __________ nervous system reflex causing the smooth muscle surrounding the reproductive ducts and acessory glans to contract.
Sympathetic
What factors control penile erection?
- Parasympathetic nerve active releases nitric oxide
- NO causes cGMP formation in smooth muscle
- cGMP causes relaxation and dilation of venous channels
NOTE: Viagrea blocks cGMP degradation by PDE5
Viagra is an inhibitor of ________, an enzyme that degrades cGMP.
Phosphodiesterase
NOTE: By elevating cGMP, erectile dystfunction can be corrected in spite of sub-optimal levels of circulating testoterone
How is prostatic hypertrophy treated?
- Prostatectomy
- Trans-urethral resection
- Radiation


