Histology-Female Reproductive System Flashcards
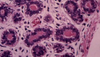
What structures are indicated in the image below?

What structures are indicated in the image below? T= tunica albuguinea connective tissue. F = follicles in cortex. M = medulla with lots of blood vessels and cells that make estrogen and progesterone.
What cells are the origin of the majority of ovarian cancers?
Surface epithelial cells account for 70% of all ovarian tumors and 90% of malignant ovarian tumors.

What cells are indicated below?

Surface epithelial (germinal epithelium) layers of the ovary. Note the simple cuboidal epithelium lying on top of the tunica albuginea connective tissue. Finally, you know you are in the ovary because you see follicles at all stages of development embedded in a stroma (note the dying follicle indicated by the black arrow).
How do follicles form during embryogenesis?
Primordial germ cells migrate from the yolk sac to the genital ridge in the embryo. The mesodermal cells from the genital ridge divide and surround the germ cells. This forms follicles.
Oocyte stem cells, what are they doing around 4 months gestation?
Oogonia. They divide by mitosis and form germ cell clusters, bridges and sync up to the same stage of mitosis.

What is happening to the female germ cells around the 7th month of gestation?
Oogonia stem cells have entered meiosis and become an oocyte. At this point they are surrounded by follicular cells.

What is happening to the female germ cells around birth?
Nothing, they are in dictyotene stage (arrested in metaphase I of meiosis I). If the oocyte is not in a primordial follicle at birth, it dies. Early in life the pool of oocytes in the ovary is fixed.

What makes up a follicle?
Oocyte + surrounding follicular cells.
When do the majority of oocytes die? Why do we lose so many between birth and puberty?
In utero. Also note that you decrease from 700,000 follicles at birth to 400,000 at puberty because primordial follicles are continually recruited for growth, but die due to lack of FSH secretion.

What is responsible for the different maturity levels of follicles shown in the ovarian cortex below?

Kisspeptin release from the hypothalamus stimulates GnRH secretion to initiate puberty. FSH is released and stimulates follicles to mature into a Graafian follicle. One follicle will have lots of FSH receptors, grow to a large size, secrete lots of estrogen and feedback inhibit FSH release from the pituitary. This causes atresia of the other follicles.

What follicles are you responsible for knowing?
Primordial follicle -> Growing follicle -> Vesicular follicle -> Mature (Graffian follicle)

What type of follicle is this?

Note the oocyte in the center and simple squamous covering. This is a primordial follicle and is quiescent until it gets hormonal signaling to divide.

What type of follicle is this?

Note the taller epithelial cells and increasing layers of granulosa cells (follicular epithelium). This indicates a growing follicle.

How do oocytes communicate with the follicle cells surrounding it?
There are gap junctions

What do glycoproteins form around the oocyte in the growing ovarian follicle? What cells transport oxygen and nutrients from the basement membrane of the oocyte and through the zona pellucida?
Zona pellucida = glycoprotein layer that induces acrosome reaction. Granulosa layer: rests on BM and transports nutrients to oocyte through zona pellucida, note that these also secrete estrogen.

How does the oocyte of a growing follicle differ from that of a primordial follicle?
The growing follicle is larger, has a thicker zona pellucida and the granulosa layer (follicular layer) is more organized.

What structures pierce the zona pellucida?
Oocyte cytoplasm and follicular cell cytoplasm. They communicate via gap junctions.

Other names for a vesicular follicle?
Secondary or antral follicle
What type of follicle is shown below?

Note that the fluid secreted by the granulosa cells forms and empty space (antrum). Also note the theca interna and theca externa. This is a vesicular ovarian follicle.

What substance secreted by the granulosa cells is key in maintaining the quiescent status of an oocyte?
Oocyte maturation inhibitor, it is contained within the antrum.
What substance is secreted by the theca interna?
Androgen. It is converted to estrogen by the aromatase of the granulosa cells.
What type of follicle is indicated in the image below?

Note that all of the antra have coalesced to from one giant antrum. Note that mural granulosa cells are covering the wall of the follicle and cumulus oophorus granulosa cells are covering the wall of the oocyte, forming the corona radiata. This is a mature/Graafian follicle.

What interchange is going on between the cumulus oophorus and the mural granulosa cells?
Mural granulosa cells are producing the oocyte maturation inhibitor and the cumuli oophorus have the receptors for the inhibiting factor.
What structures are indicated in the image below from an ovarian ultrasound?

This is a Graafian follicle: 1) Ovarian tissue 2) Follicle about to rupture 3) Remains of pedicle 4) Follicular diameter > 10mm.
What structures are indicated in the image below?

1) Uterine tube 2) Fimbriae 3) Ovary 4) Follicle 5) Stigma
400,000 oocytes remain in ovaries at puberty, but only 400 are ovulated in lifetime, what happens to all the others that aren’t ovulated?
Most of the others die by atresia and apoptosis.

What pushes the oocyte through ovulation?
A surge of LH and FSH induces an increase in volume and pressure of the follicular fluid, enzymatic proteolysis of follicular wall/stroma, deposition of glycosaminoglycans between the oocyte-cumulus complex and granulosa cells and prostaglandins trigger contraction of smooth muscle fibers in the theca externa. Note that at this time the oocyte has completed meiosis I and entered meiosis II.
What is left behind after ovulation?
Mural granulosa cells and theca interna cells. LH secretion induces follicular collapse. Blood and fibrin invade the follicular cavity. These remaining cells become the granulosa letein and theca lutein which form the corpus luteum. They begin secreting progesterone and small amounts of estrogen. Finally, a rich vascular network forms within the corpus luteum and lasts for 14 days if no implantation occurs. After 14 days it degenerates and forms the corpus albicans. Levels of estrogen/progesterone decline, the pituitary is released from negative feedback and FSH secretion begins follicular maturation again.

What are these large, blood-filled spaces?

Corpa hemorrhagica. This is the very beginning of the formation of a corpus luteum.
What hormones are responsible for the growth and proliferation of the uterus?
Early on = estrogen, later on = progesterone.
What would you expect to see on a higher power image of the structure taking up the entire ovarian cortex?

This is the corpus luteum. You would see the granulosa lutein (large cells, round nucleus, foamy cytoplasm) and surrounding theca luteal cells.

What would you expect to see on EM of a granulosa luteal cells?
Lots of mitochondria w/tubular cristae, smooth ER and lipid droplets. These are all present in all cells that make steroid hormones.

What happens to the corpus luteum on fertilization and implantation?
It grows in size, produces high levels of estrogen and progesterone (inhibits follicular development), steroid secretion declines after 8 weeks as placenta becomes major source of estrogen and progesterone and persists throughout pregnancy.
What path does the egg follow after it is ovulated and where is it typically fertilized?
Infundibulum -> Ampulla (site of fertilization) -> Isthmus -> Uterine part of oviduct

What part of the female reproductive tract is shown below?

Note the mucosal infoldings on top of a lamina propria, muscularis and serosal layer. This is the fallopian tube.
How does the uterine tube change as you get closer to the uterues?
Decreased mucosal infoldings, increased muscularis thickness, increased secretory epithelial cells and change in temperature.

What cells would you likely see on higher power of this image from the oviduct?

Note the simple columnar epithelium. There are ciliated cells and peg cells between the ciliated cells. The peg cells secrete fluid with nutrients, factors that aid in sperm capacitation and antimicrobial factors into the uterine tube. The ciliated cells sweep the oocyte towards the uterus.

Where are most ciliated cells found in the oviduct?
Infundibulum and ampulla. Note that ciliated cells increase as estrogen increases.
What increases numbers of peg cells in the oviduct?
Increased progesterone secretion.
How does the oviduct help transport the sperm up the tube?
Muscularis peristaltic contractions.
How long does the conceptus remain in the uterine tube for?
About 4 days. At 4 days increased progesterone levels causes muscle relaxation of the isthmus so the conceptus can undergo cleavage in the uterine tube and pass to the uterus.

Abnormal regions of implantation
Ovarian, tubal, intramural, abdominal and cervical pregnancies are all irregular.

Hormonal control of the menstrual cycle
*

3 phases of the uterine menstrual cycle
Proliferative phase (estrogen driven), Secretory phase (progesterone driven), and Menstruation (absence of estrogen/progesterone)
What layers of the uterus are shown below?

*

What are the layers of the endometrium?
Basal layer (repopulates functional layer) and functional layer (shed during menstruation).

What is the function of the glands shown below?

The uterine tubular glands secrete nutrients that maximize the environment for conceptus implantation.
How do you know this uterine section is in the proliferative phase?

During the proliferative phase of the menstrual cycle the epithelium reconstitutes the uterine glands lost after menses. The stromal arteries lengthen and collagen/ground substance is secreted.

How can you tell that your are in the late proliferative phase on a histological section of the uterus?
The uterine tubes begin to coil.

How can you tell you are in the secretory phase by looking at a histological section of the uterus?
Increased thickness from hypertrophy, edema and increased vascularity. You also see content in the widened lumen of the uterine tubes.

What structures are indicated in the image below?

Spiral artery in the functional layer of the uterus.
Why do women slough off the functional layer of the uterus as progesterone levels fall?
Loss of progesterone causes contraction of the spiral arteries and ischemia which causes sloughing off of the functional layer.

How do you know you are looking at a section of a uterus that is in the menstrual phase?
Less edema, shrunken uterine tubules and disruption of epithelium/blood vessels and absence of epithelial cells.

How does the myometrium grow during pregnancy?
Hypertrophy and hyperplasia
What are the two components of the placenta?
Fetal part (formed by chorionic villus) and maternal part (derived from stratum functionalis of endometrium, becomes deciduous basal is of placenta)
How does implantation occur?
The chorion (made of cytotrophoblasts with cell walls) invades the uterine wall with syncytiotrophoblasts (no cell walls) and penetrates the endometrial layer.

What structures of the endometrium are invaded by the syncytiotrophoblasts that allows for nutrient delivery to the fetus?
Uterine tubes full of glycogen and blood vessels.

How does blood flow become established to the implanting fetus?
Hypoxia drives proliferation of cytotrophoblasts. They infiltrate the spiral arteries and become endothelium, form in intervillous spaces. The maternal spiral arteries become large caliber low-resistance vessels that provide adequate placental perfusion.

What goes wrong with the cytotrophoblasts in pre-ecclampsia?
The cytotrophoblasts don’t become endothelial cells, requiring an increase in pressure to perfuse the placenta.
What are the different types of chorionic villi develop that house the pools of maternal blood for the embryo?
Primary villi: syncytiotrophoblast cells with a core cytotrophoblasts. Tertiary villi: core of mesoderm and blood vessels, this is where gas and nutrient exchange occurs between the mom and baby.

What are the different components of the maternal placenta?
Decidua basilis: chorionic villi. Decidua capsularis and decidua parietalis (these fuse).
What hormones are made by the placenta?
hCG, progesterone and estrogen.
What happens when the decidua basalis is located on the inferior side of the amniotic sac?
Placenta previa. There is no way for the baby to get through the cervix because of the blood supply and the child must be delivered via C-section.
Where does the needle have to go for chorionic villus sampling?
Decidua basalis layer where the chorionic villi are located.
What structures are indicated in the image below?

1) Amniotic epithelium 2) Baby blood vessel 3) Chorionic villi 4) Intervillous space
What makes it possible to sample maternal blood for fetal DNA?
Since the outside of the chorionic villi are lined by syncytiotrophoblasts, they form syncytial knots which break off and enter the mother’s circulation. These are composed of fetal DNA.

How does the epithelium change as you approach the cervix from the vagina?
Stratified squamous epithelium of the vagina changes to simple cuboidal epithelium of the uterus/cervix, the cervix will also have wide glands.

How do the secretion from these glands differ throughout the menstrual cycle?

Watery during menstruation, thicker mucus plug during implantation phase that prohibits sperm from messing with the conceptus.
What is this?

Nabothian cervical cysts from walling off of cervical glands. Self-limiting.
What area of the cervix is sampled in pap smears?
Zone of transition, it is most prone to cervical cancer.
What are the layers of the vaginal wall?
Mucosal layer (avascular), muscular layer w/large blood vessels and an adventitial layer.

What cyclic changes occur in the vaginal epithelium?
Estrogen promotes synthesis and accumulation of glycogen. Additionally the cells are continually desquamated.

What antiseptic properties does the vagina have?
Estrogen promotes glycogen formation. Lactobacilli vaginalis promotes glycogen conversion to lactic acid and lactic acid prevents growth of many other microbes in the vagina. This is why women are more prone to yeast infection when they take antibiotics.
What type of glands are in the mammary gland?
Modified apocrine sweat glands
What makes up the architecture of the mammary gland?
Branched alveoli, lobes with suspensory ligaments and lots of fat.

What cells make cholostrum and milk?
Cells of the alveoli
How does the mammary gland change in menstrual cycle?
Cell height increases and mild accumulation within alveoli, but is still inactive

How do you know this is an active mammary gland?

The secretory cells have proliferated in the acini and ducts. Note the intralobular duct (1) and interlobular duct (2). Additionally plasma cells are secreting antibodies in the milk.
How does milk get out of the acini?
Contraction of myoepithelial cells (pale cells surrounding acinar cells)

What type of duct is this?

Larger ducts are lactiferous ducts, note the stratified columnar epithelium.
What is the status of this mammary gland?

Post-menopausal mammary gland. Many of the elements apoptose and involute due to loss of estrogen.


