HIGHLIGHTS Flashcards
(487 cards)
Diagnostic pathology
an AUTOPSY (syn: necropsy) may be performed to determine the cause of death in an individual or in a group of animals or to explain decreased production
Forensic pathology
the purpose of an autopsy is to determine the nature of death from a legal perspective
Surgical pathology
(histologic examination of surgically excised tissue specimens) not only facilitates diagnosis and prognosis for a living animal but also can be the basis for therapy
Experimental pathology
Contributes from the design to the endpoint of an investigation with the goal of correlating morphologic changes with clinical, functional, and biochemical parameters to elucidate the mechanisms of disease
Comparative pathology
compares specific human pathologies with those seen in natural animal models
(tuberculosis, anthrax, erysipelas etc.)
Disease - What do we examine in PATHOLOGY
2., Morphological changes
(→ Pathology)
→ Morphological examinations
Most important Method to recognize/investigate the disease:
1., Autopsy
In the vast majority of the cases complementary investigations are necessary!
What is Post-mortem and ante-mortem investigations
(excision, fine needle aspirate, biopsy samples from living animals)
What is Pathogenesis
(how does the disease proceed)
What is
General pathology:
Study of the reaction of cells or tissues to injury with a focus on the mechanisms of that response.
Basic changes:
– Circulatory disturbances – Regressive changes
– Proliferative changes
– Inflammations
– Tumors
– Developmental anomalies
What is Special pathology/systemic pathology:
Characteristic changes caused by well defined diseases, grouped according to organ systems
What are the Groups according to different characteristics
Localisation, extension
– general, organ and systemic diseases
Aetiology:
– Infectious (morbidity, mortality, lethality)
• Spreading: endemic, epidemic, pandemic
• Agent: bacterial, viral, fungal, parasitic – Noninfectious
Appearance: continous, periodic, paroxysmal
Duration: fulminant, peracute, acute, subacute, chronic

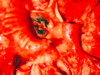
Rupture large intestines - Horse
Staining

Ziehl-Neelsen Staining
Staining

Perls Staining

Immunohistochemistry (IF, IPO), in situ hybridisation
Special staining

MAC-387
Type of lesion

Trichoblastoma, basalioma

Foot and mouth disease in Cattle, Pig and Human
Sanatio
Recovery/Healing
• Recreatio
Mild degree of functional changes, reversible morphological alterations → revivification (recreatio)
• Restitutio
– ad intergrum – cum defectu
Complete recovery following more profound tissue alterations, lost cells are replaced by corresponding tissues → regeneration (regeneratio, restitutio ad integrum/ cum defectu)
• Regeneratio
Complete recovery following more profound tissue alterations, lost cells are replaced by corresponding tissues → regeneration (regeneratio, restitutio ad integrum/ cum defectu)