Hand trauma Flashcards
What do the thumb collateral injuries include?
- Radial collateral ligament- Rare
-
Ulnar collateral ligament- most common
- aka Gamekeepers thumb- chronic injury
- Skiers thumb- acute injury
-
Steiner Lesion= avulsed ligament w/wout bony attachment is displaced ABOVE ADDUCTOR APONEUROSIS
- won’t heal without surgical repair
What is the epidemiology of thumb collateral injuries?
- Ulnar more common than radial
What is the aetiology of ulnar collateral injury?
- Hyperabduction or extension at MCPJ
Describe the anatomy of the UCL?
-
Proper collater ligament
- Runs MC head to volar aspect of prox phalanx
- resist valgus load w thumb in Flexion
- primary contraint in flexion
-
Accessory collateral ligament & volar plate
- Runs palmar to proper ligament inserts into volar plate
- resist valgus load w thumb in EXTENSION
- Primary contrainst w volar plate in extension
- __Valgus laxity in both flexion and extension = complete UCL rupture
What are the signs and symptoms of collateral thumb injury?
HX
- Hyperabduction injury to thumb
Symptoms
- Pain at ulnar aspect of Thumb at MCPJ
Signs
- Mass from torn ligament & possible bony avulsio may be present
- Stress joint w radial deviation both at NEUTRAL/30o
- Instability in 30o flexion = injury PROPER UCL
- Instability in neutral - ACCESSORY UCL injury
- compare to uninjured thumb!

What investigations are useful to dx thumb collateral damage?
- xrays- AP , lateral and oblique of thumb
- Valgus stress view may aid diagnosis if bony avulsionhas been ruled out
- MRI - aid dx

What is a stener lesion?
- Displacement of the distal end of the completely ruptured UCL such that it comes to lie SUPERFICIAL and PROXIMAL to ADDUCTOR APONEUROSIS
- Must be operated on!!

What is the TX of thumb collateral damage?
Non operative
-
Immobilisation 4-6/52
- partial tears with <20o side to side variation
Operative
-
Ligament repair
- In acute injury >20o side to side variation
- >35o of opening
-
Stener lesion
- can use suture/ suture anchor/ small screw to repair ligament
-
Reconstruction of ligament w tendon graft, MCP fusion, adductor advancement
- chronic injury

What is the tx of radial collateral ligmanet injuries?
- rare
- tx is non operative= **Immobilisation **
- indicated in most cases
- Stener lesion - doesn’t occur
Describe a repair of UCL?
- Vertical Lazy S shaped incision in direction of UCL on ulnar border of MCPJ thumb
- Protect dorsal sensory nerve- retract palmar
- thru aponeurois
- UCL proximal and superficial to this normally
- Capsulotomy
- Drill hole base of Proximal Phalanx- suture anchor
- repair UCL
- Close capsule and aponeurosis
- then skin
- POP 5 weeks
- http://www.youtube.com/watch?v=Kx5CR2MmhB8
- https://www2.aofoundation.org/wps/portal/!ut/p/c1/04_SB8K8xLLM9MSSzPy8xBz9CP0os3hng7BARydDRwN3Q1dDA08XN59Qz8AAQwMDA6B8JJK8haGFgYFnqKezn7GTH1DahIBuP4_83FT9gtyIcgBttnJy/dl2/d1/L2dJQSEvUUt3QS9ZQnB3LzZfQzBWUUFCMUEwRzFFMTBJREZMVUlRUDEwMDA!/?contentUrl=%2fsrg%2f76%2f04-Approaches%2f12-Dorsoulnar-MCP-JoinThumb.jsp&bone=Hand&segment=Thumb&showPage=approach&classification=&treatment=&method=&implantstype=&redfix_url=&approach=Dorsoulnar%20approach%20to%20the%20MCP%20joint%20of%20the%20thumb

Define digital collateral ligament injury?
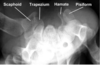
What is the epidemiology of scaphoid fractures?
- Most frequently fractured carpal bone
- Accounts for up to 15% acute wrist injuries
- location
- waist -65%
- Proximal third- 25%
- Distal third 10%
- distal pole is most common location in kids due to ossification sequence
Describe the pathoanatomy of scaphoid fractures?
- Axial load across hyper-extended and radially deviated wrist
- Common in contact sports
- transverse fractures more stable than vertical/oblique fractures
What is the prognosis of Scaphoid fractures?
- Incidence of AVN with fracture location
- Proximal 5th AVN rate = 100%
- Proximal 3rd AVN rate= 33%
Describe the anatomy of the scaphoid?
- 75% scaphoid covered in CARTILAGE
- Blood supply
- major supply- DORSAL CARPAL Branch of radial artery- enters scaphoid in a nonarticular ridge on dorsal surface and supplies proximal 80% scaphoid via a RETROGRADE blood flow
- minor via SUPERFICIAL PALMAR Arch branch of volar radial artery- enters DIstal TUBERCLE and supplies 20% DISTAL SCAPHOID
- Both intrinsic/extrinisic ligaments attach
- Scaphoid flexes w wirst flexion & radial deviation adn extends during wrist extension& ulnar deviation

Describe the signs and symptoms of scaphoid fracture?
O/E
- Anatomic snuffbox tenderness dorsally
- Scaphoid tubercle tenderness volarly
- Pain w reisted pronation

What investigations are useful in DDx scaphoid fracture?
-
Xrays
- AP and lateral
- Scaphoid view- 30o wrist extension, 20o ulnar deviation
- 45o pronation view
- no fracture but suspicion rpt 7-14 days
-
Bone scan
- diagnose occult fracture at 72 hrs
- specificity 98%, sensitivity 100%, PPV 85-93% within 72hrs
- MRI
- Most sensitive method within 24hrs
- also vasularity of prox pole
- CT Scan
- less effective than bone scan/ MRI
- Useful for location of ffracture and progression of nonunion/union post surgery
Describe the tx of scaphoid fracture?
Non operative
- stable non displaced fractures
- normal xray- cast then immobilise 12-21 days and reexam/rpt xrays
- Start immobilisation early- non union rates increase w delay of immobilisation > 4 wks post injury
- no concensus on casting- can use volar cast
- duration of casting
- distal fracture- 3/12
- mid waist- 4/12
- proximal third -5 /12
- outcomes fractures with <1mm displacment union 90%
Operative
ORIF vs Percutaneous screw fixation
what are the indications for surgery for scaphoid fractures?
- Unstable fractures
- Proximal pole fractures
- Displacment >1mm
- 15 o humpback deformoty
- radiolunate angle >15o= DISI
- Scaphoid frac ass with perilunate disslocation
- comminuted fractures
- in undisplaced fractures- to allow decreased time to union, faster return to work/sport, cheaper costs to casting- McQueen et al JBJS Br 2008
What are the outcomes of surgery for scaphoid fracture?
- Union rates of 90-95%
CAn you describe the technique for fixation of scaphoid fracture?
Approach
- Dorsal approach for Proximal Pole fractures
- Preserve blood supply when entering dorsal rige by limiting exposure to proximal half of scaphoid
- Percutaneous higher risk of unrecongnised screw pentetration of sunchondral bone
- Volar approach- for waist and distal pole fractures w humpback flexion
- allows exposure of whole scaphoid
- uses interval between FCR and radial artery
- Arthroscopic assisted also described
- Fixation is optimised by long screw down CENTRAL AXIS of SCAPHOID
- Radial stylectomy preformed if impaction between radial styloid adn scaphoid
Describe the complications of scaphoid fixation?
- Non union->
- SNAC wrist- degenerative changes first in radioscaphoid area followed by pancarpal /midcarpal arthritis
- Tx with
- **Interposition (Fisk) bone graft- **open wedge graft, 72-95% unon rates
- Inlay (Russe) bone graft- minimal deformity, 92% union rates
- Vascular bone graft from radius- 1-2 intercompartmental supraretinaculuar artery ( branch of radial artery) harvested to provide vascular bone graft from dorsal aspect wrist
- Outcomes:
- Punctate bleeding during surgery good prognostic indicator of union
- 92% w obvious bleeding, 71% questionable bleeding, 0% no bleeding
- Pt w scaphoid nonuions>5 yrs or proximal pole necrosis have less favourable outcomes
What do hamate fractures include?
- Hook of hamate- most common
- Hamate body fractures- v rare

What is the hx of hamate fractures?
- Hx of blunt trauma to palm of hand
- often seen racquet sports
- hockey
- golf- miss ball hit ground
- tennis
- Must distinguish from BIPARTITE HAMATE- Smooth cortical surfaces