Fiser.10.Nutrition Flashcards
What is your daily caloric need (kg/day)
20-25 calories/kg/day
How many calories per gram in fat?
9 calories / gram
How many calories per gram in protein?
4 calories / gram
How many calories per gram in PO carbohydrates?
4 calories per gram
How many calories per gram in dextrose?
3.4 calories per gram
What percent of calories should come from protein / fat /carbohydrates for a healthy adult male?
20% protein, 30% fat, 50% carbohydrates
How many g protein / kg / day?
1g protein / kg/day
What percent of protein intake should be essential amino acids?
20%
What molecule is provided by fat intake?
Essential fatty acids
How much can trauma increase your caloric requirement?
20-40%
How much can surgery increase your caloric requirement?
20-40%
How much can sepsis increase your caloric requirement?
20-40%
How much can pregnancy increase your caloric requirement?
300 kcal per day
How much can lactation increase your caloric requirement?
500 kcal per day
Which of the following increase your protein requirement: trauma, surgery, sepsis, pregnancy, lactation?
All of the above – trauma, surgery, sepsis, pregnancy, lactation `
What is the formula to calculate caloric requirements with burns
25 kcal/kg/day + (30 kcal/day * % burn)
What is the formula to calculate protein requirement for burn patients?
1-1.5 g/kg/day + (3g x % burn)
What is the majority of energy expenditure for burn patients?
Heat production
What percent of basal metabolic rate increases with each degree of fever?
10% for each degree above 38.0 degrees celsius
How do you calculate caloric need for overweight patients?
Weight =[(actual weight – IBW) * 0.25] + IBW
What does the Harris-Benedict equation calculate?
Calculates basal energy expenditure based on weight, height, age, and gender
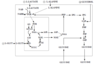
What is the nutritional basis of central line based TPN?
Glucose based
What is the maximal rate of glucose administration for central line TPN?
3 g / kg/hr
What is the nutritional basis of PPN?
Fat-based