FDN2_SM_ReceptorFamilies&Signaling Flashcards
Ion channels, transport proteins, membrane potential, action potential, receptor families and signaling, drug transport, absorption and distribution, includes week 3 signal transduction
What kind of antagonist binds reversibly to the agonist-binding site?
Competitive antagonist
Note: when both ligands are present, partial agonists act as competitive inhibitors of the full agonist
Where might a noncompetitive antagonist bind?
Irreversibly to an orthosteric site or irreversibly to an allosteric site. This prevents receptor activation.
Where does an uncompetitive inhibitor bind?
The agonist-receptor complex
How does a competitive inhibitor affect potency and efficacy?
A competitive inhibitor decreases potency (increases EC50), and has no effect on efficacy
How does a noncompetitive inhibitor affect potency and efficacy?
A noncompetitive inhibitor lowers efficacy and has no effect on EC50
How does an uncompetitive inhibitor affect potency and efficacy?
An uncompetitive inhibitor lowers efficacy, but actually increases potency (decreases EC50)
In this image, what evidence supports the conclusion that Zolpidam is a postive allosteric activator?

Zolpidam has no effect on its own, but increases the efficacy of GABA when they are applied together
What is the mechanism of action of P4S? How do you know?

Partial agonist: in the presence of GABA and P4S, there is a right shift; potency is decreased and efficacy is unaffected (remember, that partial agonists can act as competitive inhibitors).
P4S alone results in some receptor activity, indicating that it isn’t just a competitive antagonist
What is the mechanism of action of Penicillin? How do you know?

Uncompetitive inhibitor. There is little effect at low agonist concentration, the efficacy is lowered, and the potency is increased (EC50 is lowered)
Which ligand is a partial inverse agonist? How do you know?

Beta Carboline is a partial inverse agonist. When it is present, the response is lower than the basal activity without the agonist
What is the effect of an inverse agonist in constitutively active system?
The inverse agonist reduces contitutive signaling.
Note: in a constitutively active system, an antagonist would have no effect. Antagonists interfere with the “on switch” of an agonist, but there is no “switch” in a constitutive system
Which ligands bind to the orthosteric site of a receptor?
Full agonists, partial agonists, inverse agonists, competitive antagonists
What is the effect of an inverse agonist in a quiescent system?
The inverse agonist acts as a competitive antagonist
Under what conditions does constitutive receptor activity occur?
- Tumor growth
- Research experiments where researchers artificially overexpress receptors
In the image, which ligand might be a competitive antagonist?
Which might be a partial agonist?
How do you know?

Ligand A could be a partial agonist, because it is able to cause a response on its own, without the agonist present
Ligand B could be a competitive antagonist. Actually, it coudl be any kind of antagonist, because it doesn’t produce any response in the absence of an agonist
What kind of antagonist only binds to the ligand-receptor complex?
Uncompetitive
Is biological response in a cell proportional to the number of receptors bound to the agonist? Why or why not?
No! Maximal biologial response even when only a small % of receptors are bound to the full agonist. Most of the receptors are spares!
The maximal response is produced because there are many chemical intermediates that amplify the initial signal within the cell.
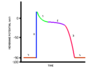
This image shows the effect on biological response to Drug A when Drug M is also applied in increasing doses. Why doesn’t efficacy fall after the first two increases in Drug M dose?

Initially, spare receptors compensate for the increased concentration of the antagonist. As the dose of Drug M increases, the spare receptors are “used up,” and efficacy begins to fall.
This image shows the effect on biological response to Drug A when Drug M is also applied in increasing doses. Is Drug M a competitive antagonist? How do you know?

Drug M is not a competitive antagonist. At increasing doses of Drug M, efficacy falls. Competitive antagonists do not affect efficacy.
Describe the constrained model of coopertivity
In the constrained model, all subunits must take the same acive conformation.
- In the “stressed” conformation, all of the subunits are inactive
- In the “unstressed” conformation, all of the subunits are active
Describe the sequential model of cooperativity
Subunits can be sequentially activated and exist in different conformations at the same time
For example, a channel opening may increase in size as each subsequent subunit is activated.
If all four subunits of hemoglobin must exist in either the T-state (stressed) or R-state (unstressed), what type of coopertivity does it exhibit?
Constrained aka concerted coopertivity
If each oxygen molecule binding to hemoglobin further increases the protein’s affinity for oxygen, what type of coopertivity does hemoglobin exhibit?
Sequential coopertivity
How do you calcualte the Therapeutic Index of a drug?
Toxic ED50/Beneficial ED50
OR
LD50/Beneficial ED50
(Use the latter if the adverse event measured is death)