Eye and Extraocular Muscles Flashcards

Testing cranial nerves IIIO, Iv, and VI can be done by asking patient to trace an H in front of each eye
Three Tunics of Eyeball

Three layers of the eye
Outer layer (Fibrous Tunic) Middle layer (Vascular tunic) Internal layer (Retina)
Three layers of the eye
Outer layer (Fibrous Tunic) Middle layer (Vascular tunic) Internal layer (Retina)
Trochlear Nerve Injury (CN IV)
Affected eye will drift upward compated to normal eye when asked to look straight ahead
Fn of occulomotor nerve and abducens nerve intact.
Some loss of depression of eye
Normal abduction and adduction of eye

Abducens nerve injury (CN VI)
Affected eye drifts medially compared to normal eye when asked to look straight ahead
Abductens nerve innervates lateral rectus, the strong ABductor of the eye
Medial rectus, strong ADDuctor of eye, intact

Outer Layer
AKA Fibrous Tunic Sclera: Dense irregular connective tissue. Supports and maintains shape of the eye. Protects internal structures, attachment site for extraocular muscles. Cornea: Two layers of epithelium and connective tissue in between. Protects anterior surface of the eye, refracts incoming light
Middle Layer
AKA Vascular Tunic Choroid: highly vascularized connective tissue. Supplies nourishment to retina, pigment absorbs extraneous light Ciliary body: smooth muscle covered with a secretory epithelium. Holds suspensory ligaments that attach to the lens and change lens shape for far and near vision, epithelium secretes aqueous humor Iris: Two layers of smooth muscle (sphincter pupillae, dilator pupillae) and connective tissue with a central pupil. Controls pupil diameter and thus the amount of light entering the eye.
Outer Layer
AKA Fibrous Tunic Sclera: Dense irregular connective tissue. Supports and maintains shape of the eye. Protects internal structures, attachment site for extraocular muscles. Cornea: Two layers of epithelium and connective tissue in between. Protects anterior surface of the eye, refracts incoming light
Middle Layer
AKA Vascular Tunic Choroid: highly vascularized connective tissue. Supplies nourishment to retina, pigment absorbs extraneous light Ciliary body: smooth muscle covered with a secretory epithelium. Holds suspensory ligaments that attach to the lens and change lens shape for far and near vision, epithelium secretes aqueous humor Iris: Two layers of smooth muscle (sphincter pupillae, dilator pupillae) and connective tissue with a central pupil. Controls pupil diameter and thus the amount of light entering the eye.
Oculomotor nerve injury (CN III))
Affected eye drifts down and out when trying to look forward
Will also have ptosis and pupil dilation (mydriasis)
Superior oblique (trochlear n) which depresses and abducts eye and lateral rectus (abducens nerve) which abducts eye in tact

Nerve injury
Muscles with opposing actions and different nerves will take over and move the eye to a specific location
Internal Layer
AKA Retina Pigmented layer: pigmented epithelial cells. Absorbs extraneous light, provides vitamin A for photoreceptors, recycles photoreceptor products Neural layer: neurons and glial cells. Detects incoming light, converts light rays to nerve signals and transmits signals to brain
Chambers of the eye
Anterior Chamber
Posterior Chamber
Vitreous Cavity
Anterior Chamber
Between Cornea and Iris, filled with aquesous humor- a liquid that resembles blood plasma with less protein and glucose and more lactate and ascorbate
Posterior Chamber
Between iris and lens. Posterior chamber is also filled with aquesous humor. Aqueous humor is produced by secretory epithelium lining the ciliary body, fills the posterior chamber and flows into the anterior chamber through the pupil
Vitreous Cavity
Surrounded by the retina and is posterior to the lens. Contains a large transparent gelitanous mass called the vitreous body composed of hyalauranic acid.
Horizontal axis of the eye
produces elevation and depression
Vertical axis of the eye
through middle of the eyeball produces abduction (away from nose) and adduction (towards nose)

Axes of the eye
Lateral Rectus
Anatomical fn:
To test:
Innervation:

Anatomical fn: ABduction
To test: Look lateral
Innervation: CN VI
Medial Rectus

Anatomical fn:
To test:
Innervation:
Anatomical fn: ADDuction
To test: look medial
Innervation: CN III

What muscle you test looking where
Superior Rectus

Anatomical fn:
To test:
Innervation:
Anatomical fn: elevation and ADDuction
To test: Look lateral and up
Innervation: CN III
Inferior rectus

Anatomical fn:
To test:
Innervation:
Anatomical fn: Depression and ADDuction
To test: look lateral and down
Innervation: CN III
Inferior Oblique

Anatomical fn:
To test:
Innervation:
Anatomical fn: Elevation and ABduction
To test: look medial and up
Innervation: CN III
Superior Oblique

Anatomical fn:
To test:
Innervation:
Anatomical fn: Depression and Abduction
To test: look medial and down
Innervation: CN IV
Lateral Rectus
Abduction (away from nose)
Abducens (CNVI)
Medial Rectus
ADDuction (towards the nose)
Occulomotor (CNIII)
Superior Rectus
Elevation and ADDuction
Occulomotor (CN III)
Inferior Rectus
Depression and ADDuction
Occulomotor (CNIII)
Superior Oblique
Depression and ABduction
Trochlear (CN IV)
Inferior Oblique
Elevation and Abduction
Occulomotor (CNIII)
Eye view

Anterior view eye
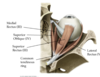
Extra occular muscles
Innervated by CN III, IV, and VI
Lateral rectus
Medial rectus
Superior rectus
Inferior rectus
Superior oblique
Inferior oblique
Retinal detachment is a separation between
the pigmented epithelium and the neurosensory portion of retina

Retinal detachment
If the detatched portion of the retina is not repositioned
it will lose metabolic support from the RPE and choroid and die
Signs and symptoms of retinal detachment include:
- The sudden appearance of many floaters
- Flashes of light in one or both eyes
- Blurred vision
- Gradually reduced side (peripheral) vision
- A curtain like shadow over the visual field

Non-proliferative diabetic retinopathy

Proliferative diabetic retinopathy
Nonproliferative diabetic retinopathy
characterized by presence of hard exudates, micro hemorrhages, and edema of the macula
Non proliferative diabetic retinopathy
can progress to proliferative form that is characterized by growth of abnormal new blood vessels, hemorrhages, retinal detachment, and blindness
The retina is
a layer of tissue lining the inner surface of the eye

Layers of the retina
Retinal pigmented epithelium (RPE)
layer of cuboidal epithelial cells in close association with photoreceptors of retina
Fns: conversion and storage of retinoid, phagocytosis of shed photoreceptor outer segments, absorption of scattered light, and ion and fluid transport
Dysfunction of RPE can result in
photoreceptor death and blindness
Outer nuclear layer of the retina
contians cell bodies and nuclei of the photoreceptors (rods and cones)
these cells gonerate a signal in response to a photon of light and transmit a signal to the neurons of the inner nucler layer
Rods
contain rhodopsin
responsible for vision in low light environment
Cones
responsible for color vision
What is the site of color blindness
cones
What is the cornea
- A colorless, transparent, highly innervated and completely avascular structure composed of cells and connective tissue. It contains 5 layers.
- Acts as eye’s outermost lens and controls and focuses the entry of light into the eye
- bends or refracts incoming light onto the lens that further refocuses light onto retina
- 65-75% of total eye focusing power
5 layers of cornea
- corneal epithelium
- bowmans layer
- corneal stroma
- descemets
- corneal endothelium
Corneal epithelium
- non keratinized stratified squamous with 5-7 layers of cells
- provide a barrier to the outside world
- contain numerous sensory nerve endings involved in blink reflex
- undergo continuous renewal from stem cells at the corneal scleral junction or limbus
Bowman’s layer
- 6-9 um thick layer of connective tissue
- supports overlying corneal epithelium and represents additional protective barrier to trauma/bacterial invasion
*
Corneal Stroma
- highly transparent layer-90% of the corneas thickness
- consists of collagen fibers
- forms a lattice that is highly resistant to deformations/trauma
- stromal cells are called keratocytes which produce and maintain collagen matrix
Descemets membrane
one of the thickest basement membranes in the body
Corneal endothelium
- lines posterior surface of Descemet’s membrane and faces anterior chamber of eye
- single layer of squamous epithelial cells with impermeable intercellular junctions that regulate influx of aqueous humor to corneal stroma
- structural and functional integrity is vital to the maintenance of a proper hydration state of the stroma and corneal transparency
What may result when the cornea fails to focus light rays precisely on the retina?
Myopia or hyperopia

Myopia
AKA Nearsightedness
- Eyeball that is too long or a cornea that is too curved
- Light rays fall short of the retina and objects in the distance appear blurred
Hyperopia
AKA Farsightedness
- eyeball that is too short or cornea that is too flat
- light rays are focused behind the retina and objects close up are blurred
Presbyopia
- objects close up blurred
- due to an age related change in elasticity of the lens
How do you correct the conditions of the cornea? (Myopia, hyperopia, presbyopia)
With eyeglasses or a surgical procedure to alter the shape of the cornea called radial keratotomy
What is the Conjuctiva?
A think, transparent mucosa that covers the exposed, anterior portion of the sclera and continues as the lining on the inner surface of the eyelids.
Functions of the conjunctiva
- keep anterior surface of the eye moist and lubricated
- keep inner surface of eyelids moist and lubricated so they open and close without friction or irritation
- protect eye from dust, debris, infection causing microorganisms
What does the conjunctiva consist of?
- stratified columnar epithelium with numerous small cells resembling goblet cells.
- Mucous secretions of the goblet cells are added to the tear film that coats the corna and prevents the occurence of dry eye syndrome
What is conjunctivitis?
AKA Pink Eye
- conjunctiva inflamed due to bacterial or viral infections/allergies
- Inflammation increases discharge of mucus and enlarges the microvasculature of the sclera –> reddish appearance
- Contagious but little effect on vision
Layers of the choroid
Choriocapillaris and Bruch’s membrane
Choriocapillaris
- vascularized connective tissue containing numerous pigment cells important for nutrition of the outer retinal layers aand absorbing scattered light rays
Bruch’s membrane
- Thin sheet of connective tissue between the choriocapillaris and pigmented layer of retina
What is the site of Age Related Macular Degeneration (AMD)?
Choroid
Damage to what structure results in AMD?
Macula
Two Forms of AMD
Dry (nonexudative, >80%)
vs.
Wet (exudative, 10-15%)
*
Wet (exudative, 10-15%)
*
- presence of angiogenic new vessels originating from choriocapillaris and penetrating Bruch’s membrane and RPE
- Vessels leak and cause scarring
- Treatment with injection of VEGF antagonists into the vitreous cavity to inhibit the formation of new vessels and stop leaking or laser treatment

Dry (nonexudative, >80%)
- diffuse or discrete deposits of lipid and protein (drusen) in Bruch’s membane of the choroid and atrophy and degeneration of the pigmented epithelium and associated photoreceptors of the retina leading to vision loss
- no effective treatment
- Diet, multivitamin, antioxidants might slow progression

Ciliary body
anterior expansion of the choroid in the posterior chamber that encircles the lens at the level of the limbus
Ciliary muscle
smooth muscle that makes up most of the stroma of the ciliary body
Ciliary Processes
ridges extending from the ciliary body and lined by a double layer of epithelium
- inner layer is highly pigmented
- outer layer of cells are highly specialized for secretion of aqueous humor
Flow of Aqueous humor
- Aqueous humor is produced continuously
Flows toward lens –> reaches anterior chamber through pupil –> flows into angle formed by the cornea with the basal part of the iris –> penetrated channels of trabecular meshwork at the corneoscleral junction (limbus) –> pumped into scleral venous sinus –> venous blood returning from the eye
What is normal intraocular pressure in adults, why is it important?
- 15-22 mmHg
- necessary for functioning optical system
- maintains smooth curvature of the corneal surface
- helps keep photoreceptor cells in contact with pigmented epithelium
What causes glaucoma? (general)
- elevated intraocular pressure –> optic nerve becomes constricted where it emerges from the eyeball through the sclera –> vision loss and blindness
- elevated pressure caused by obstruction that hampers the normal drainage of aqueous humor, which can no longer overcome the pupillary or trabecular resistance
*only glaucoma if there is optic nerve damage and associated vision loss, if not then it is ocular hypertension
Acute or closed angle glaucoma
- flow of aqueous fluid from the posterior chamber to the anterior chamber obstructed by iris tissue
- pressure builds up in posterior chamber and pushes portions of the iris upward, blocking the chamber angle

Chronic or open angle glaucoma
- chamber angle is open but drainage through the trabecular meshwork is impaired.
- most common type of glaucoma that becomes more pevalent after 40 yrs old

Treatment of Glaucoma
Primary goal is to improve drainage of aqueous humor or decrease aqueous humor production
- prostaglandin analogs
- beta blockers
- alpha agonists
- carbonic anhydrase inhibitors
*
Ciliary body
- important for lens accomodation
- system of radially oriented fibers called zonular fibers
- important for holding the lens in place and together with the ciliary body regulate the shape of the lens during the accomodation reflex
Accomodation reflex
- process by which the shape of the lens changes to maintain a clear image or focus on an object as its distance varies from the eye
- light rays from a distant object are focused on the retina by a flattened lens while light rays from a nearby object are focused on the retina by a more rounded lens
*
What happens when: ciliary muscle is relaxed and zonular fibers are put under increased tension
lens flattens
What happens when: ciliary muscle contracts and zonular fibers become lax
lens becomes more round
What innervates the ciliary body?
parasympathetic fibers of occulomotor nerve
What is the iris?
the most anterior extension of the middle vascular tunic that covers part of the lens, leaving a round central pupil that regulated the input of light into the eye
Posterior surface of iris
- has two-layered epithelium continuous with that covering the ciliary processes, but very heavily filled with melanin
- blocks all light from entering the eye except that passing through the pupil
Dilator pupillae muscle
- sympathetic fibers
- contraction causes increased pupillary aperture
Sphincter pupillae
- parasympathetic fibers of the oculomotor nerve
- contraction causes decreased pupillary aperture

The inner nuclear layer of the retina
consists of bipolar cells, amacrine cells, and horizontal cells
responsible for integrating the signals prodiced by the photoreceptors and transmitting signals to the ganglion cell layer
the ganglion cell layer of the retina
has neurons with very ling axons that make up the nerve fiber layer which come together to form the optic nerve
retinal neurons ae supported by
muller glial cells and microglial cells
Muller glial cells
extend full thickness of neurosensory retina
support retinal neurons
microglial cells
support retinal neurons
have phagocytic and other immune type functions
light rays pass through
full thickness of the retina in order to initiate the production of a visual image that is transmitted to the brain via the optic nerve

light rays passing through retina

view of retina
optic disc
location where axons from the ganglion cells of the retina exit the eye to form the optic nerve and retinal blood vessels enter and leave the eye
macula
6mm oval shaped highly pigmented spot near the center of the retina
fovea
Small pit in the center of the macula. Responsible for central, high resolution/ high acuity vision

Musles of the pupil
Sphincter pupillae
innervated by parasympathetic fibers of the oculomotor nerve
contraction causes decreased pipillary aperture
dilator pupillae
innervated by sympathetic fibers (of internal carotid plexus)
Contraction causes increased pupillary aperture


