Cytology: Inflammation & Cancer Flashcards
what are the main differences between cytology and histopathology
cytology: relatively non invasive, rarely requires sedation or GA, minimal tissue disruption during sampling, rapidly performed, rapid results, cells only, cannot assess tumour grade, accurate assessment of tumour type may be impossible, cheap
histopathology: invasive, GA or sedation required, moderate tissue disruption during sampling, more time consuming, delay as sample is fixed/sectioned, larger more representative sample, tissue architechture interpreted, possible to assess tumour grade, immunohistochemical stains may allow accurate diagnosis, costly

what are the indications to perform cytology (8)
- skin and subcut masses
- lymphadenopathy
- intrathoracic and intra-abdominal masses
- body cavity effusions
- urine sediment
- traumatic catheterization (bladder neoplasia)
- prostatic washes, bronchoalveolar lavage
- bone marrow samples
what are the basics to collecting a good cytology sample (4)
- collection of good quality sample (non-aspiration, aspiration)
- prep of a good quality smear
- correct sample staining for in house analysis
- support of experienced and well trained clinical pathologist for external analysis
what are the benefits of non-aspiration sample (5)
- minimal cell disruption (tumour cells may be fragile)
- reduces hemodilution
- excellent for lymph node aspirates
- effective for many skin tumours (mast cell, lipoma)
- may not yield a cellular sample (mesenchymal cells)
how is an aspirate sample attained
use needle with syringe attached
suction can be continuous or intermittent
avoid needle exiting the tumour
often used if non-aspiration technique doesnt yield sample
can be ultrasound guided
what are the reasons for poor quality samples (5)
- poor technique
- intrinsic nature of the lesion being sampled (fibrous, vascular, cystic, necrotic)
- hemodilution
- dirty slides
- ultrasound gel contamination
what are potential complications of obtaining a sample (4)
- intro of infection
- hemorrhage
- pneumothorax
- tumour seeding
how do you prepare a cytology smear (7)
- fill syringe with air and attach, detach from needle first if aspiration method
- expel sample briskly onto slide
- prepare smear
- air dry quickly
- label carefully
- stain and examine in house
- send air dried, unstained smears to external lab
what are the stains used
modified romanowsky stain (diff quik rapid stain)
3 solutions
methancol (fixative)
solution I (eosinophilic dye)
solution II (basophilic dye)
what is the diagnostic approach to a cytology sample

what should you note on the first look
scan slide at low power (10x)
what is the cellularity?
how are the cells distributed?
are they inflammatory cells or tissue cells?
what is the background? (red cells)
what cells can indicate neutrophilic inflammation
neutrophilic inflammation (suppurative, acute)
degenerative change may be seen
bacteria may be seen (septic) ex. cat bite abscess, surgical site infection
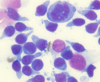
what is shown here

neutrophilic inflammation
bacteria seen
what cells would be present in a pyogranulomatous inflammation and where would this be seen
macrophages and neutrophils
ex. foreign body reactions, fungal infections, chronic injury
what cells would be present in a granulomatous inflammation and where would this be seen
macrophages and lymphocytes
chronic inflammation, specific infections (mycobacteria)
what is an eosinophilic inflammation
allergic/hypersensitivity reactions
parasitism
eosinophilic granuloma
neoplasia: mast cell tumour, some lymphomas
what is an lymphoplasmacytic inflammation
allergic/immune reactions
chronic inflammation
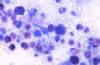
what inflammation type is shown here

eosinophilic
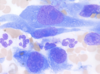
what inflammation is shown here

granulomatous inflammation
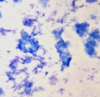
what inflammation is shown here

pyogranulomatous inflammation
what types of cells can be present in neoplasia (3)
- round cells
- epithelial cells
- mesenchymal cells
what is the cellularity of round cells
high
what is the cellularity of the epithelial cells
high
what is the cellularity of samples of mesenchymal cells
low to high
what is the cell distribution of round cells
evenly distributed
what is the cell distribution of epithelial cells
clusters or rafts
what is the cell distribution of mesenchymal cells
discrete cells
what are the cell size/shape of round cells
round, distinct borders
what are the cell size/shape of epithelial cells
round to cuboidal
cell to cell borders
what are the cell size/shape of mesenchymal cells
spindle shaped
wispy cytoplasmic tails
what other features are commonly seen in round cells
distinctive morphology
what other features are commonly seen in epithelial cells
possible acini
what other features are commonly seen in mesenchymal cells
production of matrix
what are criterias of malignancy (7)
- pleomorphism
- increased nuclear:cytoplasmic (N:C) ratio
- immature (coarse) chromatin pattern
- prominent and/or multiple nucleoli
- multinucleation
- nuclear moulding
- increased and/or abnormal mitotic figures
what are pleomorphism changes seen in malignancy (4)
- cell shape
- cell size (anisocytosis)
- nuclear size (anisokaryosis)
- nucleolar size (anisonucleoliosis)
what origin is frequenlty seen in round cell tumours
hematopoietic orgin
what is the shape of the cytoplasm in round cell tumours
round shape with distinct cytoplasmic border and round to indented nucleus
what cell type is seen here

round cell tumour
what are the round cell tumour types
LYMPH
L- lymphoma
Y- transmissible venereal tumour (TVT)
M- mast cell tumour
P- plasma cell tumour
H- histiocytic tumour
what tumour type would this be

round cell tumour
lymphoma
what cell tumour type is this

round cell tumour
lymphoma
what cell tumour type is this
round cell tumour
lypmhoma
what tumour type is this

round cell tumour
lymphoma
what cell tumour type is seen here

round cell tumour
mast cell tumour
granulation
nucleus is difficult to see because there is purple staining granules within the cytoplasm
high #s of eosinophils because mast cell tumours release cytokines
what cell tumour type is this
round cell tumour
mast cell tumour
what tumour type is this

round cell tumour
mast cell tumour
why do you need to be careful when staining mast cell tumours with diff quik
granules are not always picked up

what tumour type is seen here

round cell
plasma cell tumour
very round nucleus that sits to one side of the cell, dark blue cytoplasm with clearing beside the nucleus
bi nucleation is seen more freq
what tumour type is seen here

round cell tumour
plasma cell tumour
what tumour type is seen here

round cell tumour
plasma cell tumour
what tumour type is seen here

round cell tumour
histiocytoma
marcophage lineage, lots of cytoplasm that is pale in colour
common in young animals
what tumour type is seen here

round cell tumour
histiocytoma
what tumour type is seen here

round cell tumour
histiocytoma
how do cells exfoliate in mesenchymal tumours
poorly
exfoliate as non-cohesive aggregates and/or individual discrete cells
what are the shapes of mesenchymal cells
spindle to oval shaped with wispy cytoplasmic tails
what cell tumour type is this

mesenchymal cells
what can mesenchymal cells produce
matrix (pink)
what is usually required to classify mesenchymal cells
histopathology
aspiration generally required
what benign mesenchymal tumour types (5)
- fibroplasia
- inflammation: granulation tissue
- lipoma
- fibroma
what tumour type is seen here

benign mesenchymal tumour
lipoma
what tumour type is seen here

benign mesenchymal tumour
lipoma
what are malignant mesenchymal tumour types
sarcomas (hemangiosarcoma, leiomyosarcoma, liposarcoma)
melanoma
soft tissue sarcoma
what tumour type is this

malignant mesenchymal
sarcoma
what tumour type is this

malignant mesenchymal
sarcoma
what tumour type is seen here
malignant mesenchymal
sarcoma
what tumour type is seen here

malignant mesenchymal
sarcoma
where can epithelial cell tumours originate from
skin, resp tract, GI tract, urogenital tract, tumours of glands and organs
how do epithelial tumours exfoliate
in cohesive clumps in rafts
how are epithelial arranged
intracellular adhesions seen as tight line
what are the shapes of epithelial cell tumours
polygonal, ovoid, round, angular, cuboid, columnar
what tumour type is seen here

epithelial tumours
what are benign epithelial tumours (4)
- follicular or epidermal inclusion cysts
- basal cell tumours
- sebaceous adenoma
- epithelioma
what are malignant epithelial tumours
carcinomas
what cell tumour type is this
epithelial tumour
what tumour type is seen here

epithelial tumour
sebaceous adenoma
what tumour type is seen here

epithelial tumour
what arrangements can carcinomas be in
acinar, palisading, honeycomb, papillary etc
what tumour type is seen here

epithelial cell
carcinomas
what tumour type is seen here

malignant epithelial cell tumour
carcinoma
what tumour type is this

malignant epithelial cell tumour
carcinoma
what tumour type is this

malignant epithelial cell tumour
carcinoma
what tumour type is seen

malignant epithelial cell tumour
carcinoma
what tumour cell type is this

malignant epithelial cell tumour
carcinoma
what tumour type is this

malignant epithelial cell tumour
carcinoma
what tumour type is this

malignant epithelial cell tumour
carcinoma
what is the cellularity of naked nuclei tumours
highly cellular
how are naked nuclei tumours arranged
loosely adherent cell arrangement
occasional clusters
what are the features of cell borders of naked nuclei tumours
indistinct cell borders
what are the features of the nuclei in naked nuclei tumours
many free nuclei
nuclei round to indented
minimal anisokaryosis
what are the origins of naked nuclei tumours
endocrine/neuroendocrine
anal sac adenocarcinoma
insulinoma
thyroid tumours
what cell tumour type is this

naked nuclei tumour
what cell tumour is this
naked nuclei tumour
what tumour cell type is this

naked nuclei tumour


