Cystitis, Pyelonephritis and Interstitial Nephritis Flashcards
(57 cards)
Cystitis
- Inflammation of urinary bladder, most often due to bacterial infection. The upper urinary tract is usually not involved.
- Especially important as antecedent to pyelonephritis
Pyelonephritis
- Inflammation of upper urinary tract: renal pelvis, tubules, and interstitium, most frequently due to bacterial infection.
- Glomeruli are usually not involved.
Bacteriuria
- Bacteria in the urine.
- May be associated with clinical urinary tract Infection (UTI) or may be asymptomatic.
Interstitial Nephritis
•Inflammation of renal interstitium, and to a lesser degree the tubules, with no or minimal involvement of glomeruli.
Vesicouretral Reflex (VUR)
•Retrograde urine flow from bladder into uterus + kidney
Reflux Nephropathy
•Functional and pathologic changes in kidney resulting from VUR.
Cystitis - Symptoms
• Triad of symptoms:
– Frequency of urination
– Lower abdominal pain
– Dysuria
• Usually does not give rise to constitutional symptoms
– Occasionally: Fever, chills, malaise
Cystitis - Organisms
Causative organisms:
• Most common:
-E. coli >> Proteus, Klebsiella, Enterobacter
• Rare:
– M. tuberculosis
– Candida
– Viruses
– Chlamydia
– Schistosoma - parasite
*Important as a risk factor for squamous cell carcinoma
*Highest incidence in Africa, South America, Middle East, Egyp

Cystitis - Predisposing Factors
- Bladder calculi
- Urinary obstruction
- Diabetes mellitus
- Instrumentation
- Immune deficiency
- Cytotoxic drugs (cyclophosphamide)
– Hemorrhagic cystitis
• Radiation
Acute Cystitis - Pathological Findings (Gross)
• Gross
– Hyperemia (reddening) of mucosa
– Exudate
– If large amounts of hemorrhage = Hemorrhagic cystitis
– If large areas of ulceration = Ulcerative cystitis

Acute Cystitis - Pathological Findings (Microscopic)
• Microscopic
– Neutrophilic infiltrate, hemorrhage, ulceration of mucosa


Hemorrhagic Cystitis
Chronic Cystitis
• Persistence of infection
– Longer duration
• Pathologic findings:
– Chronic infiltrate, mostly lymphocytes, plasma cells
– Heaped up and reactive urothelium
– Fibrous thickening of muscularis propria
• Leads to decreased contractility

Chronic Cystitis - Special Histologic Forms
- Follicular cystitis
- Eosinophilic cystitis
- Interstitial cystitis
- Malacoplakia
- Polypoid cystitis
- Emphysematous cystitis
- Cystitis cystica
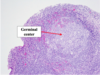
- Chronic Follicular Cystitis
- Aggregation of lymphocytes with lymphoid follicles

- Eosinophilic Cystitis
- Submucosal eosinophils, fibrosis and occasional giant cells
- Rarely part of a systemic allergic disorder
Interstitial Cystitis
- Most frequent in women
- Inflammation and fibrosis in all layers of the bladder wall, often with ulceration
– Can mimic gross appearance of carcinoma in situ (CIS)
- Highly incapacitating and difficult to treat
- Symptoms:
- Intermittent and severe suprapubic pain
- frequency
- urgency
- hematuria
- dysuria

- Malakoplakia - cystitis
- Unique form of chronic cystitis; caused by chronic E. coli infection
- Immunosuppressed patients (esp. transplant recipients)
- Similar inflammatory process can occur in kidney, colon, lungs, and prostate
- Pathologic features:
– Gross: Multiple yellowish plaques in mucosa and submucosa

- Malakoplakia - cystitis
- Microscopic Pathologic features:
- Large foamy macrophages, multinucleate giant cells, lymphocytes
- Michaelis-Gutmann bodies
– Round, concentric intracytoplasmic concretions within macrophages and between cells – Thought to represent defects in phagocytosis

Polypoid Cystitis
• Results from mucosal irritation
- Common in patients with indwelling bladder catheter
• Mucosal appearance:
- Broad polypoid projections due to submucosal edema
• Can be confused with urothelial carcinoma
Emphysematous Cystitis
•Inflammation associated with formation of air-filled spaces

Cystitis Cystica
- Nests of transitional epithelium gown downward into lamina propria; may have central cystic spaces
- Can be seen in normal bladders, but also in the setting of inflammation and metaplasia

Pyelonephritis
•Acute
-Most resolve
•Chronic
- Persistent/recurrent infections
- Due to abnormalities of the urinary tract
•Majority (>95%) are ascending infections from the bladder
– Hematogenous spread also occurs
• Most are bacterial infections:
– > 85% due to gram negative rods from the intestinal tract
– Most common: E.coli
– Others: Klebsiella species Proteus mirabilis Enterobacter species
– Less common: Staphylococci, Enterococcus
• Rare – Viral infections, mycobacteria, fungi
Pyelonephritis - Nosocomial Infections
- Indwelling bladder catheters, patients on multiple antibiotics
- Most are due to E.coli
- Other organisms: Pseudomonas, Serratia, Staphylococcus epidermis, Candida albicans