Breast Flashcards
Where might a congenital supernumerary nipple occur?
along milk lines
Difference between screening mammogram and Diagnostic mammogram
- Screening= asymptomatic patient
- Diagnostic= if pt c/o lump, etc (or if screening mammo is abnl)
What is a BI-RADS score used for
Used to score findings found on diagnostic mammorgram-
helps to determine if findings are normal/benign/concerning and helps determine next steps (When to follow-up or if you shoudl refer to surgeon)
Why is it important to correlate an abnormal mammogram with a prior study?
This could tell you if the finding has been present and stable for many years and therefore does not require further work-up
What is the initial diagnostic study for a young, low-risk woman with suspected fibroadenoma
Ultrasound
Fibroadenoma:
- MC young or old?
- MC in which race?
- solitary mass or numerous?
young
black
solitary mass
CPx of what?
- Round/ovoid
- rubbery
- movable
- non-tender
Fibroadenoma
How do you dx Fibroadenoma?
Core needle biopsy
What is definitive tx for Fibroadenoma
excision
What is the name of a large fibroadenoma that grows rapidly? Why is this concerning

Phyllodes tumor
Can be malignant
How do you treat a Phyllodes Tumor
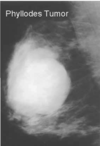
Excision required
What condition?
- MC 30-50y/o
- Increased risk with alcohol use
Cyst/fibrocystic changes
Fibrocystic breast disease is dependent on what hormone
estrogen dependent
Which condition?
- Painful
- Single or multiple
- Bilateral
- Rapid changes in size and appearance
- Nodular breast tissue
- Mobile
Fibrocystic breast disease
(breast cysts are usually single but can have the same characteristics as fibrocystic breast disease)
How do you diagnose Cyst/Fibrocystic changes of the breast?
- mammogram/ultrasound
- Fine needle aspiration
How do you treat Cyst/Fibrocystic changes of the breast?
- Breast support
- Rx: Danazol (only if severe)- was not on slide
Use of evening primrose oil, low fat diet, avoiding caffeine and vit E does NOT have great evidence
Cyst/Fibrocystic changes will subside with what
Menopause
Are cysts or fibroadenomas usually tender?
Cysts
(fibroadenomas are usually nontender)
MC age to have a fibroadenoma? Cysts?
- Fibroadenoma_- 15-25y/o_ (usu. puberty and young adulthood)
- Cysts- 30-50y/o (regresses after menopause except w/ estrogen therapy)
What is the MC female cancer and the 2nd MCC of cancer death in women in the US ?
Breast cancer
Risk factors of what?
- Female
- White race
- Postmenopausal obesity
- High estrogen levels
- BRCA1/BRCA2 genes
- Personal/FHx ovarian, peritoneal or breast cancer
- Radiotherapy to chest b/w age 10-30
Breast Cancer
What are the 5 protective factors for breast cancer
- Breastfeeding
- Higher parity
- Physical activity
- Oophorectomy < 35y/o
- ASA use
What is the risk calculator used for breast cancer in average risk women
Gail model
What are the USPSTF breast cancer screening guidelines for average risk women
50-74y/o, every 2 years






