Anatomy - Thorax / Asthma Flashcards
What is the purpose of costal cartilage?
Provides resilience and stability
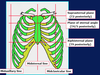
What are these parts called?


What are these lines called?

What are the properties of intercostal muscles?
In intercostal space
3 layers - external, internal, innermost
Respiration importance
Help keep intercostal space rigid
Where is pleura found and what are the 2 types?
Each lung is enclosed in serous pleural sac
2 continuous membranes - visceral (surface) and parietal (inner surface – lines pulmonary cavities)
What are these parts called?


What is a health problem related to the thorax?
Thoracic outlet syndrome - where important arteries and nerves are compressed
What are the 2 thoracic apertures and their function?

What number are these atypical ribs?


What are these parts called?


What is the purpose of the scalene tubercule on rib 1?
Where scalene anterior muscle attaches
Where does the pectoralis major attach to?
Clavicular head which attaches to clavicle
Sternocostal head which attaches to sternum + upper 6 costal cartilages
Fibres which converge on intertubercular groove or humerus
What is the function of the pectoralis major?
- Adductor and medial rotator of arm at shoulder joint
- Can act also as flexor (when arm extended) and as extensor (when arm flexed)
- If pectoral girdle is ‘fixed’, it can act also as an accessory muscle of respiration
Which nerves innervate the pectoralis major?
Medial and lateral pectoral nerves (C5-8 and T1)
Where does the pectoralis minor attach to?
Coracoid process of scapula, ribs 3-5 near cartilage
What is the function of the pectoralis minor?
Depressor of scapula (and, hence, shoulder) and protractor of scapula
If pectoral girdle is ‘fixed’, it can act also as an accessory muscle of respiration
Which nerve innervates the pectoralis minor?
Medial pectoral nerve (C8 and T1)
What are these parts called?


What is the mediastinum?
Central part of thoracic cavity, between pleural cavities
What are the boundaries of th mediastinum?
Sternum (anterior)
Thoracic vertebral column (posteriorly)
Thoracic inlet and root of the neck (superiorly)
Diaphragm (inferiorly)
What are these parts called?


What are the contents superior mediastinum?
- Thymus (lymphoid organ; large between birth and puberty but involutes in adult, especially after disease);
- Great veins (SVC, brachiocephalic vv);
- Phrenic nerves;
- Arch of aorta and branches;
- Origins of internal thoracic arteries;
- Pulmonary aa and vv;
- Vagus nn;
- Recurrent laryngeal branches;
- Trachea (lower half) and bifurcation into main bronchi (T4/5 in expiration); Oesophagus;
- Thoracic duct
What are the divisions are the mediastinum?
Superior and inferior –> behind manubrium sterni and behind body and xiphoid process of sternum
What are these parts called?


What are the contents of the inferior mediastinum?
- Divided into anterior, middle and posterior regions:
- Anterior: Internal thoracic aa and vv (and anterior intercostal branches); thymus (possibly); sternopericardial ligaments
- Middle: Heart and pericardium (serous and fibrous); phrenic nn and pericardiophrenic aa and vv; IVC (diaphragm to right atrium)
- Posterior: Descending aorta (and branches); azygos vv (and tributaries); oesophagus; thoracic duct; sympathetic trunks (and branches)
What are these parts called?


What are these parts called?


What is the purpose of trachea cartilage?
Keeps airways open
What are these parts called?


What are these parts called?


What happens during breathing?
- At rest, diaphragm relaxed
- Muscles of respiration contract to expand thoracic cavity - mainly diaphragm
- This increases thoracic volume / decreases intra-thoracic pressure
- Air drawn into lungs from outside (where pressure greater)
- Air passes into terminal bronchioles / alveoli to oxygenate blood
- Diaphragm relaxes, lungs recoil, thoracic volume decreases, intrathoracic pressure increases and air expelled
What are the properties of the diaphragm?
The most important muscle in respiration
Dome-shaped muscular partition
Separates the thorax and abdomen
Innervated by phrenic nerve – C3-5
Anteriorly attaches into the xiphoid process and costal margin
Laterally attaches to ribs 6-12
Posteriorly attached to T12 vertebra
What does a superior view of diaphragm look like?

What are the properties of intercostal muscles?
- Assist in inspiration and expiration
- Have obliquely angled fibres from rib to rib
- The contraction of External and Internal fibres raises each rib toward the rib above, to raise the rib cage
- Innermost and Internal depresses each rib to the rib below, to lower the rib cage
What are A, B and C?

A = external intercostal muscle
B = internal intercostal muscle (interosseus part)
C = internal intercostal muscle (interchondral part)
What are these parts called?


What are the directions of movement of the sternum and ribs?
Sternum = pump handle movement
Ribs = bucket handle movement

What are the properties of the different types of pleura and lungs?
Pleura = Serous membrane divided into parietal and visceral layers; surround the lungs; contain the pleural cavities; separated by serous fluid
Parietal pleura = Outer; lines thoracic cavity
Visceral pleura = Inner; covers lung following lung fissures
Lungs = Go above 1st rib; covered by suprapleural membrane.
What causes thoracic cavity and lungs to expand?
Surface tension between 2 pleura layers
What are the properties of babies breathing?
- Babies can only breathe via abdominal breathing
- Newborn ribs more horizontal so cant use pump/bucket handle movements
- Intercostals weak
- Abdominal breathing is done by contracting the diaphragm
- As the diaphragm is located horizontally between the thoracic and abdominal cavities, air enters the lungs and the thoracic cavity expands
- Reliance on the diaphragm for breathing means there is a high risk for respiratory failure if the diaphragm is not able to contract
What are the properties of children’s breathing?
- Nasal breathers until 4 – 6 wks
- Short neck & shorter, narrow airways – more susceptible to airway obstruction / respiratory distress
- Tongue is larger in proportion to the mouth - more likely to obstruct airway if child unconscious
- Smaller lung capacity and underdeveloped chest muscles
- Have a higher respiratory rate – newborns ~60 breaths/min, early teens ~20-30 breaths/min
What is a health problem related to breathing?
Harrison’s suculus - defect from rapid breathing causing rib deformation in children
What is the costodiaphragmatic recess?
Where fluid will accumulate in the lungs (look for this abnormality in X-rays)

What does the use of accessory muscles during rest indicate?
Respiratory distress as lungs cannot provide enough oxygen to the body
What is neonatal respiratory distress syndrome?
- Affects premature babies, if they are born before their lungs are fully developed and capable of working properly
- The more premature the baby, the more likely it is that s/he will have respiratory distress syndrome
- Approx. half of all babies born before 28 weeks of pregnancy will develop NRDS
- Leading cause of death in newborns (accounts for 20% of deaths)
What is acute respiratory distress syndrome (ARDS)?
- Fluid / proteins leak from the blood vessels into the alveoli (air sacs)
- Lungs become stiff and so don’t work normally
- Breathing becomes difficult
- Mainly affects people over 75
- Approx 1 in 6,000 people per year affected in England
- Common causes are an infection in the lungs e.g pneumonia
- Lung clots or injury (e.g from a car crash), could also trigger the condition
What are the symptoms of respiratory distress?
Blue extremities
Rapid and shallow breathing
Rapid heart rate
What are the properties of asthma?
Common - ~ 5.4million people in UK receive treatment
An inflammatory disease of the airways of the lungs; persists long-term
- Muscles around the walls of
the airways tighten - so airways
become narrower
- The lining of the airways
becomes inflamed
Variable symptoms - shortness of breath, wheezing, tightness of chest, coughing
What are these parts called?


What is pneumothorax and the 2 types?
- Perforation of parietal pleura = air in pleural cavity
- Tension and non-tension pneumothorax
What is non-tension pneumothorax?
Hole so air in and out, no build-up
Less severe

What is tension pneumothorax?
Air breathed in cannot escape, so remains and builds with each breath
Flap of tissue covers opening
Heart is pushed over - leads to arrythmia

What happens during emphysema?
- COPD
- Over-inflated alveoli so ineffective gas exchange

How is asthma characterised?
Reversible decreases in FEV1:FVC (first expiratory volume in first second and total amount of air expelled)
How is asthma diagnosed?
Variations in PEF which improve with B2 agonist use
What are the properties of COPD?
- Chronic bronchitis and emphysema
- Chronic bronchitis = + airway mucus, airway obstruction and intercurrent infections
- Emphysema = alveoli destruction
- +90% related to smoking
- FEV1 reduced
- Little PEF (peak expiratory flow) variation
What is bronchial calibre control?
Parasympathetic + sympathetic
Sympathetic = circulating adrenaline acting on B2 adrenoceptors on bronchial smooth muscle, causing relaxation
What effect does parasympathetic system have on airways?
- A.Ch. acts on muscarinic M3–receptors:
- Bronchoconstriction
- Increase mucus
What effect does sympathetic system have on airways?
- Circulating adrenaline acting on beta2-adrenoceptors on bronchial smooth muscle to cause relaxation.
- Plus sympathetic fibres releasing NA, acting at adrenoceptors on parasympathetic ganglia to inhibit transmission.
- Beta2-adrenoceptors also on mucus glands to inhibit secretion.
What activates sympathetic nerve?
Irritants, such as dust
Leads to bronchoconstriction
What are the properties of asthma attacks?
Genetic predisposition, provoked by:
Allergens
Cold air
Viral infections
Smoking
Exercise
May be characterised by Early (Immediate) phase followed by Late phase
What do lung function test graphs look like before and after b2 agonist use for someone with asthma?
Decrease in FEV1, reversed by B2 agonist

What are the 3 spasmogens?
- Histamine
- Prostaglandin D2
- Leukotrienes (C4 and D4)
What are 2 chemotaxins and what do they do?
Leukotriene B4, PAF (platelet activating factor)
Lead to late phase
Attract leukocytes (+ eosinophils and mononuclear cells)
Leads to inflammation and airway hyperactivity
What are the 2 pharmacological therapy basis for asthma?
Bronchodilators - reverse bronchospasm in early phase and offer rapid relief
Prevention - prevent attacks, are anti-inflammatory
What are the properties of B2 adrenoceptor agonists?
- Increase FEV1
- Salbutamol
- Increase cAMP on smooth muscle B2-adrenoceptors
- Reduce parasympathetic activity
- By inhalation
- Prolonged use can lead to receptor down-regulation
- Long acting beta agonists (LABA) given for long-term control (i.e. salmeterol)
What is an example of a xathine and its properties?
i.e. theophylline
Bronchodilators, not as good as beta adrenoceptor agonists
Oral or IV in emergency (aminophylline)
Adenosine receptor antagonist
Phosphodiesterase inhibitors

What are examples of muscarinic m-receptor antagonists and their properties?
i.e. ipratropium / tiotropium
Block parasympathetic bronchoconstriction
Inhalation = prevents antimuscarinic side effects
Little value in asthma, used for COPD
What are examples and properties of anti-inflammatory agents?
Preventative
Corticosteroids - i.e. beclomethasone (inhalation) or prednisolone (oral)
Anti-inflammatory = by activation of intracellular receptors, leading to altered gene transcription, less cytokine production, and production of lipocortin/ Annexin A1 (a protein)
What is the function of lipocortin (annexin A1)?
Inhibits prostaglandin and leukotriene synthesis
What are the properties of steroid treatment in asthma?
- Given with B2-agonists
- Reduce receptor down-regulation
- Side effects - throat infections, hoarseness (inhalation) and adrenal suppression (oral)

What is an example and the function of leukotriene receptor antagonists?
i.e. montelukast
+ role as add on therapy
Preventative and bronchodilator
Antagonise actions of leukotrienes
What are the properties of omalizumab?
Role in difficult to treat asthma
Directed against free IgE but not bound IgE
Prevents IgE from binding to immune cells which lead to allergen-induced mediator release in allergenic asthma
What is stepped care and the clinical pharmacology?
Follow guidelines - if salbutamol is used +2 times per week, step up
Spacer devices (patients with – technique and reduce steroid impaction)
Bronchodilator before steroid
Rinse mouth after steroid

What is lung compliance and the properties it in regards to the lungs?
Lung compliance = stretchiness
High pressure = stiffer lung = low compliance
Base of lung = + compliant than apex for better ventilation
Compliance = ensued by elastic recoil
Decreased lung compliance = pulmonary fibrosis, alveolar oedema e.g.
Increased lung compliance = normal ageing lung
Healthy lung = + lung compliance, - alveolar surface tension due to surfactant
What are the 3 lung function tests?
Test mechanical condition of lungs (pulmonary fibrosis)
Test airway resistance (asthma)
Test diffusion across alveolar membrane (pulmonary fibrosis)
What does a spirometer graph tell us?

TV = tidal volume - volume of air entering and leaving the lung with each normal breath
VC = vital capacity - maximum amount of air expelled from the lungs after first filling the lungs to a maximum then expiring to a maximum (TV+IRV+ERV)
IRV = inspiratory reserve volume - extra volume of air inspired above the normal tidal volume with full force
ERV = expiratory reserve volume - extra volume of air expired by forceful expiration at the end of normal tidal expiration

What forced vital capacity (FVC), FEV1.0 and their ratio?
Total volume exhaled
Volume expired in the first second, usually >80% of FVC
FEV1.0 / FVC
What does the helium dilution test test and what are the equations?
Functional residual capacity tests
V1 = known initial volume of helium
C1 = known initial concentration of helium

What does the nitrogen washout test test and how does it work?
- Functional residual capacity
- Patient inspires 100% O2
- Expires into the spirometer system
- Procedure repeated until N2 in lungs is replaced with O2
- FRC calculated from exhaled N2 and estimated alveolar N2

What is restrictive deficit and what diseases does it occur in?
- Lung expansion is compromised - alterations in lung parenchyma, disease of the pleura or chest wall
- Lungs do not fill to capacity hence they are less full before expiration
- E.g. pulmonary fibrosis and scoliosis
- FVC is reduced, but the FEV1.0. is relatively normal
- The FEV1/FVC also remains relatively normal/increased
What is obstructive deficit and when does it occur?
- Characterised by airway obstruction
- If airways are narrowed, lungs can still fill to capacity
- Resistance is however increased on expiration
- E.g. asthma, chronic obstructive pulmonary disease (COPD)
- FEV1.0 will be reduced, but FVC will be relatively normal.
- A low FEV1.0/FVC will be recorded
What is the function of a vitalograph?
Measures ability to move air out of the lungs FVC and FEV1.0
What is the Miller’s prediction quadrant?

What is peak expiratory flow (PEF) recorded as and how does it work?

What do flow-volume loops look like and what type of defecit is the red and orange ones?
Red = restrictive deficit
Orange = obstructive deficit

How do measure PEF and what is gas transfer-diffusion conductance?
Peak flow meter
- Measures how easily CO crosses from alveolar air to blood
- The patient inhales a single breath of dilute carbon monoxide followed by a breath-hold of 10 seconds
- The diffusion capacity is calculated from the lung volume and the percentage of CO in the alveoli at the beginning and the end of the 10s breath-hold
- Clinical relevance - e.g. in fibrosis of the lungs where gas diffusion is compromised

What is the pericardium divided into and what is its function?
Fibrous (outer)
Serous (inner)
Surround the heart
What are the properties of the fibrous pericardium?
- Tough and not distensible
- Attached to diaphragm by pericardiophrenic ligaments
- Blends into adventitia of great vessels
What are the properties of the serous pericardium?
- Comprises visceral layer (epicardium) and parietal layer (lining fibrous pericardium)
- Potential space between them (pericardial cavity)

What do the parietal and visceral pericardial layers line?
Parietal = lines inner surface of fibrous pericardium
Visceral = lines surface of the heart

What are the 4 surfaces of the heart?
Anterior or sternocostal: formed mostly of right (with bit of left) ventricle
Inferior or diaphragmatic: mostly L (with bit of R) ventricle
Posterior or base: mostly L (and bit of R) atrium and pulmonary vv
Pulmonary: mostly L ventricle, in cardiac notch of L lung
What are the 4 borders of the heart?

Superior: from L costal cartilage 2 to R costal cartilage 3
Right: convex to R; from R cc3 to R cc6; mainly R atrium with SVC and IVC
Inferior: lies on diaphragm central tendon; from R cc6 to L intercostal space 5; mainly R ventricle and part of L ventricle
Left: convex to L; from L ics5 and back to L cc2; mainly L ventricle and maybe some L atrium

What are the 4 valve positions and what are all valves?
All valves = retrosternal in position and close to the midline
Pulmonary = medial to L cc3
Aortic = medial to L ics3
Bicuspid or mitral = medial to L cc4
Tricuspid = medial to R ics4

What are the 4 valve sounds and their locations?
Pulmonary: L ics2 near sternal edge; ‘dup’ sound
Aortic: R ics2 near sternal edge; ‘dup’ sound
Bicuspid or Mitral: L ics5 at midclavicular line; ‘lub’ sound
Tricuspid: L ics5/6 near lower sternal edge; ‘lub’ sound
What are the properties of the parietal pleura?
- Lines thoracic cavity lateral to mediastinum
- Supplied by intercostal and phrenic nerve
- Is sensitive to pain
What are the properties of the visceral pleura?
- Covers lungs and follows lung fissures
- Supplied by autonomic nerve
What is a condition related to the pleura?
Inflammation of the pleura. The lung surfaces end up rough so the ‘pleural rub’ can be heard with a stethoscope. Leads to chest pain (usually sharp) when you take a breath or cough.
What are the 4 types of pleura and their properties?

Dark green = Mediastinal: flat, faces mediastinum and has impressions of mediastinal structures; contains the hilum and pulmonary ligament
Light green = Diaphragmatic: concave and faces domes of diaphragm
Red = Costal: convex and faces ribs
Blue = Cervical: extends into neck, 2-3 cm above medial third of clavicle, as apex, dome or cupola
What are pleural reflections?
The abrupt lines along which the pleura change direction (reflect) from one wall of the pleura cavity to another
Occur where the costal pleura becomes continuous with the mediastinal pleura anteriorly and posteriorly, and with the diaphragmatic pleura inferiorly
What are the properties of the visceral pleural reflections?
Reflections closest at plane of sternal angle (rib 2);
Parallel down to rib 4; L indented (cardiac notch) butR continues to cc 6;
Cross rib 8 at midaxillary line;
Cross rib 10 at lateral borderof erector spinae m

What are the properties of the parietal pleural reflections?
Again, asymmetry and close behind sternal angle (rib 2);
Parallel down to rib 4;
L indented (cardiac notch) but R continues to cc 6;
Rib 8 at midclavicular line;
Rib 10 at midaxillary line;
Rib 12 at lateral border of erector spinae m
What are the properties of the right lung?
- Has 3 lobes (superior, middle and inferior) separated by the oblique and horizontal fissures;
- Oblique fissure from T2 vertebra posteriorly to rib 6 anteriorly;
- Horizontal fissure from rib 4 to oblique fissure;
- Superior and middle lobes mainly anterior;
- Inferior lobe mainly posterior

What are the properties of the left lung?
- Has 2 lobes (superior and inferior) separated by the
oblique fissures;
- Oblique fissure from T2 vertebra posteriorly to rib 6 anteriorly;
- Superior lobe mainly anterior and has lingula;
- Inferior lobe mainly posterior

What is the main property of each bronchopulmonary segment?
Have own nerve, vein and artery supply
What are the properties of the bronchi divisions?
- Trachea divides into right and left
- Right is wider and more vertical than left
- Each bronchus divides into secondary bronchi (supplying lobes)
- Secondary divide into tertiary bronchi (supplying segments)
- Right lung has 3 lobes and 10 segments
- Left lung has 2 lobes and 9/10 segments

Why are the anatomical, functional and surgical units of the lungs required to be known?

- X-ray interpretation
- Surgical resection in disease (segment resection is preferred to lobe resection)
- Draining fluids (fluids tend to accumulate in apical and posterior segments of inferior lobe)
What are the great vessels of the heart?


What are thedifferent parts of the aorta?

Descending aorta = divided into thoracic and abdominal aorta
What is the function of the azygous vein?

Drainage of posterior thoracic wall
What are these CT scans showing?

1 = left is right and right is left side of heart
2 = arch of the aorta
3 = ascending aorta and descending aorta
What are the 3 respiratory system compartments?
Conduction zone - conditioning of inhaled air
Respiratory zone - site of gas exchange
Musculo-elastic ventilation apparatus - drives ventilation
What is the main property of airway division?
Divides in successions of bifurcations
How is turbulence created in the nasal cavity?
Created by turbinate bones in nasal cavity which form narrow passageways
What is the function of the large venous plexus in submucosa?
Enhance temperature adjustment and moisturising
What is the function of vibrissae?
Prevent large particles entering nose as large hairs at nasal cavity entry
What is the function of mucus?
Traps small particles and covers lining all the way to terminal bronchioles
What are these parts called?


What are these parts called?


What are these parts called?
What happens during infection?

Venous plexus swell during infeciton, blocking airway

What are these parts called?


What are the properties of the trachea?
- Kept open by horse-shoe shaped cartilage
- Has seromucous glands in submucosa
- Smooth muscle completes rings, formed partially of cartilage

What are the properties of the respiratory epithelium?
- Pseudostratified, ciliated and varying in thickness
- Has mucus producing goblet cells
- Mucus is transported towards pharynx by cilia (mucociliary clearance)
What are the properties of a bronchus?
- Has cartilage in its wall of varying size
- Lumen bordered by respiratory epithelium
- Ring of smooth muscle located between epithelium and cartilage
- May have submucosal glands

What are the properties of a bronchioli?
- Derived from bifurcations downstream of bronchi
- No cartilage in wall
- Fewer goblet cells in epithelium
- Incomplete smooth muscle ring surrounds
- No submucosal glands

What are the properties of the smaller bronchiole?
- Epithelium becomes cuboidal
- Ciliated and non-ciliated club cells
- Club cells have protective role
- Club cells generate serous secretions
- Incomplete smooth muscle ring surrounds epithelium
- Higher ratio of muscle ring thickness to luminal diameter than bronchi
What is the function of terminal bronchioles?
Give rise to respiratory bronchioles that have cuboidal epithelial and alveoli built in walls

What do connective tissue of alveoli contain?
Numerous elastin fibres
What is the blood air barrier formed of?
Thin capillary endothelium and type 1 cell wall
Where do alveolar capillary networks get their blood supply from?
Pulmonary circulation
What are the properties of pulmonary arteries?
- Elastic arteries
- Comparatively thin walls
- Larger ones accompany bronchi and bronchioles
Where do bronchi get their blood circulation from?
From the aorta

What is the function of surfactant?
Reduces surface tension in alveoli

What are these parts?


Where are lymph vessels found and what is their function?
In septa next to vessels of pulmonary circulation
- Drain into series of major lymph nodes along trachea
- Network found in interstitial layer adjacent to pleura
What is Waldeyer’s ring?
What does airway mucus contain?
Tonsils - aggregates of lymph follicles
Immunoglobulins mainly IgA
What is the purpose of regulated immunological response?
What does exaggerated immunological response result in?
Protection
Tissue damage (hypersensitivity)

What are the different types of hypersensitivity?

What are the properties of mast cells?
- Generate inflammatory response
- Activated by 2+ type 1 allergens binding to receptors
- Mediators released
- Tissue damage
What are the steps of an allergic reaction?
What is the purpose of IL-4 and IL-13?
When does allergic sensitisation occur?
IL-4 and IL-13 = cause B cell to switch and produce IgE antibodies instead
At first exposure

What can Th2 cells promote?
Type 1 hypersensitivity

What happens during skin test with IgE and IgE + T cells?

What happens during actue and chronic repsonse to allergens?

What happens during the triggering mechanism?

What are examples of type 2 allergies and autoimmunities?
Allergies:
- Allergeric haemolytic anaemia
- Blood transfusion reactions
- Haemolytic disease of newborn
Autoimmunities:
- Autoimmune haemolytic anaemia
- Myasthenia gravis
- Grave’s disease
How does haemolytic disease of newborn arise?

What are exampkles of type 3 allergies and autoimmunities?
Allergies:
- Dermatitis herpetiformis
- Allergic alveolitis
Autoimmunities:
- Systemic lupus erythmatosus
- Rheumatoid arthritis
What are examples of type 4 allergies and autoimmunities?
Allergies:
- Contact dermatitis
- Acute graph rejection
Autoimmunities:
- Thyroiditis
- Addison’s disease
- Gastritis
- Type 1 diabetes mellitus
What is the process of immune complex transport and removal?

How does the respiratory diverticulum form?
Forms as a blind-ending outgrowth from ventral wall of foregut

What happens during trachea development?
- In 4th week
- Oesophagotracheal ridges fuse to form oesophagotracheal septum

What are the 2 layers of the laryngotracheal tube and their funciton?

What are the 4 stages of lung development?
- Pseudoglandular stage
- Canalicular period
- Terminal sac period
- Alveolar period
What happens during the first stage of lung development (pseudoglandular stage)?
Terminal bronchioles form
All major lung components formed at end of period, expect those for gas exchange (5-16 weeks)

What happens during the second stage of lung development (canalicular period)?
- Enlargement of lumens of bronchi and terminal bronchioles
- Tissues = vascularised
- 24 weeks = each terminal bronchiole has formed 2+ respiratory bronchioles
- First terminal sacs form at end of period at end of respiratory bronchioles
What happens during the third stage of lung development (terminal sac period)?
- terminal sacs form
- Flat and thin epithelial cells of terminal sacs (type 1 alveolar cells/ pneumocytes)
- Capillaries close to flat cells and bulge into primordial alveoli allowing gas exchange
- Secretory round e cells form (type 2 alveolar cells) between flat cells
What happens during the fourth stage of lung development (alveolar period)?
- surfactant production
- 5% of mature alveoli before birth
- size of primordial alveoli
- Thinner type 1 cells
- Capillaries = closer as they mature
- Postnatal + lung size due to + divisions to form respiratory bronchioles and continues primordial alveoli production
What happens during pleural cavity development?
Pericardioperitoneal canals are separated from pericardial cavity by pleuropericardial folds (5th week)
Cavities narrow and are 2 separate cavities surrounding the heart but are separate from the heart
The pericardioperitoneal canals (which form the pleural cavities) remain connected to the peritoneal (abdominal) cavity until closed by fusion of the pleuroperitoneal folds during formation of the diaphragm

What are the propertieds of type 1 and 2 alveolar epithelial cells?
Type 1 = thin, allowing efficient gas exchange
Type 2 = round, secretory formed from end of 6th month, produce surfactant

What are the properties of surfactant?
- Produced by type II alveolar epithelial cells
- Phospholipid-rich fluid
- Forms a monomolecular film over internal walls of the terminal sacs and mature alveoli
- Lowers surface tension at the air-alveolar interface
- Produced from the end of 6th month, though at low levels
What lung changes occur before birth?
- Amount of surfactant produced increases before birth, mostly in the last 2 weeks of gestation
- Breathing movements occur before birth to stimulate lung development and respiratory muscles.
- Amniotic fluid is aspirated
What lung changes occur at birth?
This fluid is removed from the lungs by:
1) Pressure on the thorax during delivery expelling fluid through mouth and nose
2) Absorbed into circulation via the pulmonary circulation
3) Absorbed into lymphatics
A thin coating of surfactant is left lining the alveolar cell membranes
Lungs = half filled with fluid
Still born lungs = full of fluid if firth breath not taken or full of air if first breath taken
What are the 4 embryonic components of the diaphragm?
- Transverse septum
- Pleuroperitoneal membranes
- Dorsal mesentery of oesophagus
- Muscular ingrowth from lateral body walls
What are the properties of the transverse septum?
- Mesodermal in origin
- Grows dorsally from ventrolateral body wall
- Forms early in development
- Forming liver embedded in tissue
- Caudal to pericardial cavity – partially separating it from peritoneal cavity
- Primordium of central tendon of diaphragm

What are the properties of the pleuroperitoneal membranes?
- Form from the lateral wall of pleural and peritoneal cavities
- First appear at the start of the 5th week
- Forms posterior and lateral parts of diaphragm, by fusing with the transverse septum and dorsal mesentery in the 7th week
What are the properties of the dorsal mesentery of the oesophagus?
- Will form the median region of the diaphragm
- Forms muscle bundles anterior to the aorta, the “Crura of the diaphragm”
- Derived from myoblasts that had previously migrated into the dorsal mesentery of oesophagus
What 3 things fuse to form the full diaphragm and complete abdominal - thorax separation?
Pleuroperitoneal membranes
Dorsal mesentery
Transverse septum

What is the purpose of muscle ingrowth during the 12th week?
Contributes muscle to peripheral region of diaphragm external to the region that is derived from the pleuroperitoneal membranes

What are defects and problems associated with lung development?
- Premature baby and respiratory distress syndrome
- Oesophageal artesia and tracheoesophageal fistula
- Congenital cysts of lungs
- Congenital diaphragmatic hernia
What happens during premature baby RDS?
- Insufficient surfactant in lungs
- High surface tension at air-blood interface
- Risk of alveoli collapsing during expiration
- RDS = 2% newborns
- Rapid labored breathing
What happens during oesophageal atresia and tracheoesophogeal fistula?
- Abnormal separation of oesophagus and trachea by oesophageal septum
- 1/3000 births
- in males
- Associated with CHD (fistula = abnormal opening / passage) (atresia = narrowing or withering away)

What happens during congenital cysts of the lungs?
- Abnormal terminal bronchi dilation
- At lung periphery usually
- Poor drainage
- Chronic lung infections
What happens during congenital diaphragmatic hernia?
- Hole in diaphragm, usually posterior lateral
- Abdominal contents become herniated and enter thorax
- Lung = hypoplastic
- Heart = under pressure
- Mediastinum pushed to right

What are the 5 main red cell physiologies?
- Erythropoiesis
- Haemoglobin structure
- Haemoglobin biochemistry
- O2 transport
- CO2 transport
How is erythropoiesis controlled and what is its funciton?
- Essential to maintain RBC level
- Controlled by ERYTHROPOIETIN - polypeptide hormone
- Released by peritubular cells in kidney - in response to hypoxia (low oxygen) e.g.
- Anaemia
- At altitude
- Chronic lung disease (e.g. COPD)
- Increases number of stem cells committed to erythropoiesis
- Recombinant erythropoietin (EPO) used clinically
- Treat anaemias associated with renal failure.
- Open to abuse by athletes?
What is a reticulocyte?
What happens during red cell maturation?
An immature RBC
- Immature RBC - nucleus extruded and taken up by bone marrow macrophages
- mRNA in RETICULOCYTE allows haemoglobin to still be synthesised
- The reticulocyte may enter blood stream - (0.5-2% of circulating RBCs)
- Retic count elevated when erythropoiesis is increased:
- bleeding
- haemolysis
What is the lifespan of RBCs and its properties?
- 120 days
- Measurement: incubate a sample of blood with 51Cr, which binds to Hb.
- Measure disappearance from blood + sites of RBC destruction detected by surface counting.
- Useful for haemolytic anaemias - increased disappearance + increased radioactivity at sites of destruction:
- Spleen in spherocytosis
- Liver in sickle cell anaemia
- Degradation of RBCs: Occurs in reticuloendothelial system (mononuclear-phagocyte system) of spleen, liver + bone marrow.
- Proteins degraded and recycled, iron retained in stores, porphyrin from haem converted to bilirubin in liver (+ bilirubin = jaundice).
What is the structure of haemoglobin?
- 2 components HAEM & GLOBIN
- Tetrameric: 4 globin chains, each made of polypeptide with a haem prosthetic group
- Haem: Ferrous iron, Fe2+ at the centre of a protoporphyrin complex
- The Globin chains linked by non-covalent bonds

What’s the difference between adult and fetal Hb?
Adult haemoglobin (Hb A) contains a2b2 subunits
Fetal Hb contains a2y2
What are the properties of iron?
- Iron - from diet:
- Ferrous iron (Fe2+)
- (Fe3+ reduced to Fe2+ by stomach acid) –ve effects of antacids, chelation by tetracycline
- Fe3+ produced by mucosal cells of duodenum. Binds to apoferritin to produce ferritin (stores)
- Release iron into blood to bind with transferrin (transport)
- Delivers iron to bone marrow (ferritin stores)
- Iron in Hb
- Iron recycled - very efficient (90%) from breakdown of RBCs in liver and spleen
- Iron uptake in guts increased when iron deficient: erythroid regulator from bone marrow & an iron stores regulator
How is oxygen transported?
- RBCs carry O2 from lungs to tissues and return CO2
- Ferrous (Fe2+) iron in haem binds O2
- 4 O2s per Hb
- Hb is an ALLOSTERIC PROTEIN: the binding of 1O2 enhances (by a conformational change) the binding of another O2 to another haem in same molecule etc.
- The 4th O2 binds some 300 x more readily than the 1st.
What does an oxygen dissociation curve look like and what is the comparison between maternal and fetal curve?
First O2 binding = + affinity for 2nd to bind = enhances 3rd binding = enhances 4th binding

What is the Bohr effect?
- Acidity enhances the release of O2 from Hb
- Increasing CO2 at constant pH also lowers Hb’s O2 affinity
- Therefore, O2 is more readily given up to metabolically active tissues (which produce H+ and CO2).

What is 2,3-diphosphoglycerate (DPG)?
- Present in RBCs at same molar conc as Hb
- Reduces O2 affinity of Hb - in its absence Hb would yield little O2 to tissues
- DPG binds to deoxyhaemoglobin to shift equilibrium. Reduces O2 binding
- Fetal Hb unable to bind DPG - hence higher O2 affinity
- DPG increased when arterial O2 reduced chronically (e.g. at altitude, severe COPD) so O2 more readily liberated to tissues
What is carboxyhaemoglobin?
- Is CO + haemoglobin
- Hb has a much greater affinity for carbon monoxide than oxygen - carboxyhaemoglobin
- CO-Hb does not readily dissociate
- Tissue becomes starved of O2
- CO - cigarette smoke so smokers have higher levels of CO-Hb - contributes towards vascular diseases due to smoking
What is methaemoglobinaemia?
- Iron in Ferric (Fe3+) not ferrous state
- Cannot carry O2
- Patient may be
- Cyanosed
- Symptoms of anoxia (dizziness, respiratory distress, tachycardia)
- Hereditary lack of glucose-6-phosphate dehydrogenase, which keeps Hb in reduced state
- May be caused by drugs - e.g. antimalarials, sulphonamides through oxidant stress
How is carbon dioxide transported?
- 10% dissolved
- 30% bound to Hb - combines to form carbaminohaemoglobin
- 60% as HCO3-
- CO2 + H2O –> HCO3- + H+
- catalysed by carbonic anhydrase in RBC
- Hb buffers H+
- HCO3- may leave cell, Cl- enters (Chloride shift) to maintain charge
What are the problems with NSAIDS?
Can provoke asthma by increasing leukotriene production
i.e. aspirin, ibuprofen
What are the properties of beta blocker use in asthma and COPD?
Asthma = contraindicated
COPD = used with caution
What are some causes of breathlessness?
- Respiratory –> asthma, COPD, pneumonia, lung cancer
- Cardiovascular –> heart failure, pulmonary oedema (accumulation of fluid on lungs), pulmonary embolism (blood clot on lungs), atrial fibrillation
- Other –> functional breathlessness (i.e. obesity), anaemia (full blood count required)
- Pneumothorax
- Iatrogenic (caused by medicines)
- Foreign bodies
- Panic attacks
What are the 3 steps of differential diagnosis?
- What is likely to be wrong
- What is unlikely to be wrong
- ‘Conformation bias’ (closed minded so only focus on a certain condition/s)
What history do you need to take when someone reports with breathlessness?
- Age
- Onset of symptoms
- Variability
- Smoking history
- Drug history
- Occupation
- Pets
- Associated symptoms
- Orthopnoea (breathlessness from changing posture – related to heart failure)
What are the 2 signs of respiratory disease and potential diagnoses?
- Digital clubbing
- Lung cancer
- Bronchiectasis
- Pulmonary fibrosis
- Cardiac eg Fallot’s tetralogy
- Cyanosis (bluish colour)
- Central:
- Reduced O2 saturation, tongue and lips
- Cardiac/resp with shunting of blood
- Peripheral:
- Hand and feet due to poor blood flow
- Central:
What do you look for during physical examination for breathlessness?
- Palpation and percussion
- Auscultation
- Wheeze: expiration, limitations of flow in asthma and COPD
- Crackles: opening of closed bronchiole
- Early Inspiratory associated with diffuse airflow limitation
- Late inspiratory associated with pulmonary oedema, fibrosis and bronchiectasis
- Pleural rub
- Inflammation of pleural surfaces
What are the 2 methods for measuring blood gases?
Arterial blood gas monitoring
Pulse oximetry (<92% = hypoxia symptom)
What do lung function graphs tell us and how do normal, asthma and COPD compare on the graph?
FEV1 = volume of air expelled in the first second
FVC = total volume of air expelled after 6 seconds

What diseases can chest X-rays show us?
Fluid
Tumours
TB
What is V/Q scanning and how does it work?
Ventilation / perfusion (bloodflow)
- Pulmonary 99mTc scintigraphy: under-perfused areas
- Technetium (99mTc) albumin macroaggregated
- Inhalation of Xenon-133 gas to detect under-ventilated areas
- Pulmonary embolism: striking perfusion/ventilation mismatch
What are the symptoms of chronic heart failure?
- Left ventricular failure
- Pulmonary oedema
- Dyspnoea [Breathlessness] – sensation of drowning. ‘Cardiac asthma’
- Cough
- Orthopnoea – breathless on lying which is relieved by sitting up. Nocturnal problem? (paroxysmal nocturnal dyspnoea)
- Inspiratory crepitations
What are the properties of pneumonia?
- An inflammation of the alveoli in the airways - usually due to infection
- Infection: bacterial or viral
- Aspiration e.g. vomit
- Fluid accumulates in the alveoli and impairs gaseous exchange
Which nerves are shown here?


Which nerves are shown here?


Which nerves are shown here?


What are each of these in the hilum of the right lung?


What are each of these in the hilum of the left lung?


What are each of these impressions from?


Where are the vomer, hyoid bone, palatine bone, conchae and turbinate bones located in the skull?

Where is the thyroid cartilage, circoid cartilage, tracheal cartilage and arytenoid cartilage?

What are the nasal branches of the maxillary artery?

What are these nerves?


What muscle is this?


What are each of these sinuses?


What is shown by this radiograph?

Hyoid bone
Air in pharynx and larynx
Soft palate
Nasopharynx
Oropharynx
What are the key features of this radiograph?

Maxillary sinus
Nasal septum
Frontal air sinus
Entrance to nasopharynx
What are hilar shadows on X-ray mainly made up of?
Pulmonary vessels
What are numbers 6, 7, 17, 20, 21, 22, 23?

6 = Oesophagus
7 = Trachea
17 = T5 vertebral body
20 = Arch of aorta
21 = Anterior mediastinum
22 = superior vena cava
23 = Arch of azygous vein
What are numbers 18, 22, 23, 24, 25, 27, 28, 29?

18 = T6 vertebral body
22 = Superior vena cava
23 = Arch of azygous vein
24 = Ascending aorta
25 = Descending aorta
27 = Pulmonary trunk
28 = Right pulmonary artery
29 = Left pulmonary artery
What does the upper respiratory tract consist of vaguely?
What is the function of the pharynx and the larynx?
Nose
Nasal cavity
Pharynx
Larynx
Pharynx = respiration and digestive passageway
Larynx = voice, maintains open airway and directs food and drink appropriately
What is the order of the respiratory tract bifurcations?
Trachea
Bronchi
Conductive bronchiole
Terminal bronchiole
Respiratory bronchiole
Alveoli
What are the 3 steps of respiration?
Pulmonary ventilation - Air into lungs
Pulmonary respiration - Air from gas exchange at alveoli
Tissue respiration - Air from capillary to tissue cell
What does Boyle’s law state?
Pressure = inversely proportionate to volume at a constant temperature
P ≈ 1 / V
What is the role of water vapour in respiration?
- Inspired air = saturated with water vapour
- Dilutes gases
- At 37 degrees, partial pressure = 6.3 KPa
- Moist air enables efficient gas exchange
How do you convert KPa into mmHg?
1 KPa = 7.50 mmHg
What does Dalton’s law of partial pressure state?
Pressure exerted by each gas = independent of other gases present
Total pressure = sum of all individual pressures
How do you work out pulmonary ventilation rate (PVR) and what are its units?
Respiration rate X Tidal volume
Units = L/min
During exercise can reach 120 L/min
What is dead space in the lungs?
How do you work out dead space ventilation rate?
What is alveolar ventilation rate (AVR) and how do you work it out?
Serial dead space = volume of conducting airways (0.15L typically)
Distributive dead space = part of lungs that aren’t airways and dont’ support gas exchange (i.e. dead alveoli) (0.02L typically)
Physiological dead space = serial + distributive dead space (0.17L typically)
Physiological dead space X respiration rate
Actual amount of air that reaches alveoli
AVR = PVR - dead space VR
When does dead space ventilation occur?
With rapid shallow breathing, reducing alveolar ventilation
What factors affect airway resistance?
- Airway smooth muscle tone —> During asthma attack, airways reduced in size causing obstructed airflow
- Gravity and posture —> + airway resistance when in supine (led down) position than upright position as even blood flow distribution
- Lung compliance —> increases with age due to loss in elastic recoil (emphysema = + lung compliance, pulmonary fibrosis = - lung compliance)
- Age
- Disease
How do you detect airway resistance?
Auscultation:
- High and turbulent airflow in bronchi produces breath sounds
- Laminar flow in small bronchioles produces no breath sounds
- Small airways = silent zones = hard to detect disease of small airways
What does low diffusion resistance depend on?
Respiratory membrane
Gas permeability
What are 2 respiratory membrane disorders?
Oedema fluid on interstitial space
Lung fibrosis
- Increased diffusion resistance
- Interferes with normal gas exchange
What are the 2 ways gas transfer is controlled and where are they found?
Neural regulation —> cerebral cortex (voluntary breathing), pons and medulla (involuntary breathing)
Chemical regulation —> central chemoreceptors (on medulla), peripheral chemoreceptors (in aortic arch and carotid arteries), ventilation-perfusion matching
What is perfusion?
When is ventilation-perfusion matching used?
Process where deoxygenated blood passes through lungs and becomes re-oxygenated
Detection of pulmonary embolism


