Acute Inflammation Flashcards
What is inflammation?
A well ordered vascular and cellular response of tissues to aggression.
• It is a defense mechanism to eliminate initial cause of injury and the consequences of that injury (i.e necrotic cells) and initiate repair
What are the two components of acute inflammation?
Vascular: Vascular component characterized by hyperemia, vasodilation and vascular leakage. This is to “dilute” the cause of injury.
Cellular: Cellular component is to heal/ repair the injury
What is a consequence of inflammation?
• Potential for substantial tissue damage. Sometimes the inflammation will cause a worse injury.
What is the purpose of inflammation?
- contain injury
- destroy/ dilute or wall off offending agents
- remove damaged or necrotic tissue (macrophages)
- prepare tissue for repair / healing
What are the beneficial aspects of inflammation? The harmful aspects of inflammation?
- Good: Diluting and/or inactivating biological
and chemical toxins. Killing or sequestering microbes,
foreign material, necrotic tissue, and neoplastic cells. Providing wound healing factors. Restricting movement for healing and repair
• Bad: Prolonged release of inflammatory mediators, excessive fibrosis, hypersensitivity and autoimmunity, chronic inflammation can lead to neoplastic transformation,
What are the 5 cardinal signs of inflammation?
◦ Heat and redness (Hyperemia and vasodilation)
◦ Swelling ( edema and emigration of leukocytes)
◦ Pain (chemical mediators)
◦ Loss of function ( can preserve tissue and allow for healing)
What are the vascular changes associated with acute inflammation?
- Vascular: Hyperemia, Vasodilation, Increased vascular permeability (edema)
- Cellular: - Emigration of leukocytes (predominantly neutrophils) and delivery at the site of injury, to kill and/or neutralize the inciting stimulus
What orchestrates cellular and vascular changes of acute inflammation?
• Cellular and vascular changes are orchestrated by chemical mediators (many of them)
What is the clinical definitions of inflammation? Pathologic definitions? What is seen in subacute inflammation?
Clinical definition
• Acute: Hours to days
• Chronic: weeks to months to years
Pathologic definition
• Acute: edema, fibrin, neutrophils
• Chronic: macrophages, lymphocytes, plasma
cells, few neutrophils, fibrosis
Subacute: Lymphocytes and Plasma cells.
What is the general process of acute inflammation?
- Bacteria and other pathogens enter wound
- Macrophages “senses” bacteria through their receptors and phagocytize
- Chemical mediators secretion by activated
macrophages and mast cells 4. Hyperemia, vasodilation and increase vascular permeability - Leakage of fluid (edema) and neutrophils
- Neutrophils phagocyte and/or secrete
granules that kill and degrade pathogens - Macrophages secrete cytokines that attract leukocytes to the site and activate cells involved in tissue repair
- Inflammatory response continues until the foreign material is eliminated and the
wound is repaired
What are the causes of acute inflammation?
• Infections (bacteria, viruses, parasites)
• Trauma
• Physical agents (heat, cold)
• Toxins
• Tissue necrosis (of any origin; products of degenerate or
neoplastic processes)
• Foreign bodies (grass awn, sutures)
• Immunological reactions
What are the primary vascular and cellular responses during acute inflammation?
- Mast cell will sense injury and will secrete cytokines that will increase vascular permeability, endothelial cell contraction, chemotaxis of neutrophils.
- Diapedesis of erythrocytes can also occur - mild hemorrhage.
What occurs during the fluidic phase of acute inflammation? What is the purpose?
1) Increase blood flow (hyperemia) and vasodilation (mediated by Histamine, NO, PGD2, Bradykinin, LTB4) 2)↑Vascular permeability (mediated by Histamine, Bradykinin, C5a, C3a, PGE2, Leukotrienes, PAF, IL-1, TNF)
- Leads to leakage of fluid, plasma proteins and leukocytes (neutrophils) to the tissue
- Exudate
- Purpose: Dilute, isolate (surround), and trap (contain) the injurious agent and damag
What is transudate? What is exudate?
• Transudate - accumulation of fluid- clear, watery, translucent, low protein/ plasma cells.
◦ Think of mechanism of edema, increased hydrostatic (CHF), decreased osmotic (parasitism, PLN, PLE, Liver failure), lymphatic obstruction (tumors)
• Exudate: inflammation, accumulation of opaque, thick fluid. A lot of plasma proteins, neutrophils, macrophages, inflammatory cells, ect. Mechanism is increased vascular permeability.
◦ Fibrin also present due to decreased vascular permeability
What mediates increased vascular permeability?
• Mediated by vasoactive amines (histamine, bradykinin), C5a and C3a, prostaglandins, leukotrienes, PAF, IL-1 and TNF
What are the mechanisms of increased vascular permeability?
1) Retraction of endothelial cells
2) Direct endothelial cell injury 3) Leukocyte-mediated vascular injury
4) Increased transcytosis
What occurs during retraction of endothelial cells?
• Mediated by vasoactive amines
• most common
• Gap formed between endothelial cells to allow fluid and plasma cells to leak out.
- Mediated by vasoactive amines
(histamine, bradykinin, serotonin), NO,
IL-1 and TNF
What occurs during direct endothelial cell injury?
• can cause necrosis, and detachment of cell from underlying basement membrane
• activation of platelets, clotting and complement cascades
• Thermal injury, chemotherapeutic drugs, radiation, bacterial cytotoxins, viral and protozoal infections
◦ Protozoa can cause vasculitis, ect
What occurs during leukocyte mediated vascular injury?
- can cause necrosis, and detachment of cell from underlying basement membrane
- Neutrophils/ other leukocytes attach to endothelial cells and release ROS and proteolytic enzymes ( from lysosomes)
• usually associated with bacteria, or viruses that affect neutrophils.
- Ricckketsia is one example. RMSF
What is the end result of increased vascular permeability? What is fibrin?
- end results are fibrin, strands of fibrin.
- Fibrinous pleuritis.
- Fibrin is chemoattractant to neutrophils
- If inflammation does not resolve or if it is exacerbated by chemical mediators (pro- inflammatory cytokines), there will be accumulation of neutrophils
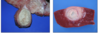
What is seen in this image?

Fibrin : Fibrinous pleuritis
What is seen in this image?

Fibrinosuppurative pleuritis
**Fluidic and cellular phase occur together
What is the purpose of cellular phase of acute inflammation? What is the result?
• Purpose of cellular phase: Deliver leukocytes into the exudate so they can kill and/or inactivate the stimulus
Results in:
- Exudation
- Cellular activation
• Microbial killing ( by phagocytosis, or release of proteolytic degradative enzymes)
• Extent/ intensity of this process causes varying degrees of injury to adjoining normal tissue.
- Clear necrotic cells and debris
What are the steps of the leukocyte adhesion cascade? What is it mediated by?
1) Margination
2) Rolling
3) Activation and Stable Adhesion
4) Transendothelial cell migration
Mediated by adhesion molecules and cytokines/chemokines (histamine, TNF, IL-1):
- Selectins (Rolling)
- Integrins + VCAM and ICAM (Activation and Stable Adhesion)
- PECAM and JAM (Transendothelial cell migration)