3 Pharmacokinetics Flashcards
What is pharmacokinetics?
Pharmacokinetics is the study of the movement of a drug into and out of the body
“What the body does to the drug”
What is pharmacodynamics?
Pharmacodynamics is the study of drug effect and mechanisms of action
“What the drug does to the body”
What is pharmacogenetics?
Pharmacogenetics is the effect of genetic variability on the pharmaco- kinetics/dynamics of a drug on an individual
What are the two forms of drug administration?
- Enteral – delivery into internal environment of body (GI tract)
- Paraenteral – delivery via all other routes that are not the GI
What are the 9 different types of drug administration into the body?
- Oral
- Intravenous
- Intramuscular
- Transdermal
- Inhalation
- Subcutaneous
- Sublingual
- Intrathecal
- Rectal
Briefly, identify and describe the four main processes involved in drug therapy?
- Pharmaceutical process – “Is the drug getting into the patient?”
- Pharmacokinetic process – “Is the drug getting to its site of action?”
- Pharamcodynamic process – “Is the drug producing its required pharmacological effect?”
- Therapeutic process – “Is the pharmacological effect being translated into a therapeutic effect?”
What are the four processes involved in pharmacokinetics?
- Drug in:
I. Absorption
II. Distribution
- Drug out:
I. Metabolism
II. Excretion

What is bioavailability?
Bioavailability is the fraction of a dose which finds its way into a body compartment (usually the circulation)
ie how much is absorbed
How does one calculate oral bioavailability?
Oral Bioavailability (F) = AUCoral / AUCIV
(AUC= area under curve)

What are the factors which affect bioavailability?
- Absorption
- drug formulation
- age
- food
- vomiting
- malabsorption
- First pass metabolism
What is first pass metabolism?
First pass metabolism is any metabolism occurring before the drug enters the systemic circulation (eg liver)
Identify three common locations where first pass metabolism occurs
- The Gut Lumen
- The Gut Wall
- The Liver
What are the two factors affecting drug distribution?
- Protein binding
- Volume of Distribution (Vd)

In three steps, explain how protein binding determines drug distribution
⇒ In systemic circulation, many drugs are bound to circulating proteins
⇒ Most drugs must be unbound to have a pharmacological effect
⇒ The free fraction of the drug can bind to cellular receptors, then gain access to cellular enzymes
Once in the systemic circulation, many drugs are bound to circulating proteins.
Provide four examples of this
- Albumin (acidic drugs)
- Globulins (hormones)
- Lipoproteins (basic drugs)
- Acid glycoproteins (basic drugs)
Changes in protein binding can occur, causing changes in drug distribution. However, these are only important if 3 criteria are met.
What are these criteria?
- High protein binding
- Low Vd
- Has a narrow therapeutic ratio
Identify four factors which affect protein binding
- Hypoalbuminaemia
- Pregnancy
- Renal failure
- Displacement by other drugs
What is volume of distribution?
Volume of distribution is a measure of how widely a drug is distributed in body tissues
If a drug is not bound to plasma proteins, it is available for distribution to the tissues of the body.
How can you calculate volume of distribution? (equation)
Volume of distribution (Vd) = Dose / [Drug]t0
Smaller Vd- drug confined to plasma and ECF
Larger Vd- drug distibuted throughout tissues
What are the end products of drug metabolism (usually)?
- After conjugation, water-soluble metabolites are formed
- Usually, they are pharmacologically inactive
What are the end products of drug metabolism (usually)?
Describe two circumstances where drug metabolism produces active metabolites
- After conjugation, water-soluble metabolites are formed
- Usually, they arepharmacologically inactive
- Pharmacologically inactive compound → pharmacologically active compound e.g. pro-drugs
- Pharmacologically active compound → other active compounds eg. codeine to morphine
Phase I metabolism involves oxidation and reduction reactions.
Which group of enzymes control these reactions? What do they do? Where are they found?
Cytochrome p450 family of enzymes
CYP450s are a super family of isoforms responsible for approximately 90% human drug metabolism through oxidative reactions
- They metabolise toxins such as carcinogens and pesticides
- Found mainly in liver (some gut and lung)
Explain how drugs can control the activity of Cytochrome P450 enzymes
Enzyme-inducing and enzyme-inhibiting drugs that alter the rate of metabolism of other drugs
Identify five other factors, apart from drugs, which influences the activity of cytochrome p450 enzymes
- Age
- Liver disease
- Hepatic blood flow
- Cigarette use
- Alcohol consumption
Identify 6 routes of drug elimination and state which one is the main one?
- Kidneys (main route)
- Lungs
- Breast milk
- Sweat
- Tears
- Genital secretions
Three processes (within kidneys) determine the renal excretion of drugs.
Identify these
- Glomerular Filtration
- Passive tubular reabsorption
- Active tubular secretion

What is clearance?
Clearance is the ability of body to excrete drug (mostly = GFR)
Describe the relationship of clearance with GFR and t1/2
- GFR is directly proportional to clearance
- t<strong>1/2</strong> is inversely proportional to clearance
i.e. a reduction in clearance (/ GFR) increases t1/2
Describe the features of 1st Order kinetics – linear
- Rate of elimination is proportional to drug level
- Constant fraction of drug eliminated in unit time
- t1/2 can be defined
Describe the features of Zero Order kinetics – non-linear
Rate of elimination is constant

How does one calculate the elimination rate constant (k)?
k = Cl / Vd
How does you calculate half life (t1/2)?
t<strong>1/2</strong> = ln2 / k
Most drugs exhibit zero order kinetics at high doses.
Why is this?
Because the receptors / enzymes become saturated

Zero order drugs are more likely to result in toxicity, hence, drug monitoring essential.
Why does this occur?
- Fixed rate of elimination per unit time
- “Small” dose changes may produce large increments in [plasma] which may lead to toxicity
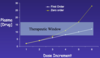
Provide 5 reasons (characteristics of the drugs) for drug monitoring
- Zero order kinetics
- Long half-life
- Narrow therapeutic window
- Greater risk of drug-drug interactions
- Known toxic effects e.g. bone marrow suppression
What is the steady state (CpSS) of the drug?
- Steady state (CpSS) refers to the situation where the overall intake of a drug is in dynamic equilibrium with its elimination
- Usually, 4-5 half lives are required to reach steady state

Loading doses are employed to reach CpSS more rapidly.
What are loading doses?
- A loading dose is an initial higher dose of a drug that is given at the start of a drug course before dropping down to a lower maintenance dose
- Useful for drugs that have a long systemic half-life (eliminated slowly)

How does one calculate loading doses?
Loading Dose = Vd x [Drug]target


