13 Cardiac Arrhythmias Flashcards
What is a cardiac arrhythmia?
- Disturbance in cardiac cycle where either:
- Pacemaker (SAN) functions incorrectly or
- Abnormal contraction/conduction in the heart
= insufficient to maintain cardiac output
Give some possible symptoms of cardiac arrythmias.
How is an arrythmia diagnosed?
- Palpitations
- Feeling dizzy
- Fainting
- Short of breath
Diagnosed:
ECG
How can bradycardic cardiac arrythmias be caused? (2)
-
Conduction block in (may be due to ischaemia) :
- AV node
- Bundle of His
- Bundle branches
-
Sinus bradycardia
- SAN- slower depolarisation
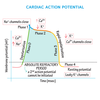
The following diagram shows a normal cardiac myocyte action potential. Describe what happens in phases 0-4 (in terms of ions).


Explain the action potential of the SAN in terms of the ions involved.

How can tachycardic cardiac arrythmias be caused? (4)
-
Ectopic pacemaker activity - eg following ischaemia or mitral stenosis
- Supraventricular
- Ventricular
-
After depolarisations - long QT/scarring
- Abnormal depolarisation of cardiac myocytes
- Early (phase2/3)
- Later (phase 4)
- Abnormal depolarisation of cardiac myocytes
-
Re-entry loops-eg due to ischaemia
- Impulse blocked- travels in retrograde way- re-excites area- another AP in quick succession
-
Wolff-parkinson white syndrome
- Abnormal electrical conduction in heart- impulses travel down bundle of Kent –> faster HR
- (Tachycardia can be caused a fibrillations)

Give some causes of atrial/ventricular fibrillations.
-
Ectopic focal points firing electrical impulses
- Tachycardia and irregular impulses
- High blood pressure
-
Mitral valve disease
- Stenosis- dilation and damage to atria
- Regurgitation- irritation of atria
- Ischaemia
What is the most common arrhythmia? Why should a person with this type of arrhythmia be given anticoagulants?
Atrial fibrillation
- Increased chance of clot formation- give anticoagulants
- Causes: breathlessness and poor perfusion- prevents 10% of blood entering ventricles
What are the 4 classes of anti-arrhythmic drugs?
(Anti-arrhythmics work to reduce abnormal impulse generation or slow conduction through tissue)
- Sodium blockers
- Beta blockers
- Potassium blockers
- Calcium channel blocker (CCBs)
How do sodium blockers work to treat arrhythmias? (class 1)

- Slow depolarisation= RHYTHM CONTROLLING
- Decrease slope in phase 0
- Doesn’t affect SAN Na as uses HCN channels

How do beta blockers work to treat arrhythmias? (class 2)
(DON’T give to asthmatics)
- SAN- decrease slope of funny current = RATE CONTROLLING
- (by blocking sympathetic nervous system)
Give 2 examples of class 2 antiarrhythmics.
Beta blockers
- Propanolol
- Bisoprolol
How do potassium blockers work to treat arrhythmias? (class 3)

Increase refractory period- RHYTHM CONTROLLING
- Prevents early depolarisations
- No potassium can leave
- Prolongs phase 3/plateau
Give an example of a class 3 antiarrhythmic (potassium blocker) and give its potential side effects.
Amiodarone (wide spectrum- effective for most arrhythmias)
Can act on: sodium channels, potassium channels, calcium channels, &as non competitive beta blocker
Side effects:
Gets deposited everywhere
- Pulmonary fibrosis
- Hepatic injury
- Increase LDL cholesterol
- Thyroid disease
- Photosensitivity
How do calcium channel blockers work to treat arrhythmias? (class 4)
Prevent calcium influx- slows heart rate - RATE CONTROLLING
Prolongs phase 2

Give 2 examples of calcium channel blockers used to treat arrhythmias.
- Diltiazem
- Verapamil
Give an example of a Class IA antiarrhythmic.
- How is it administered?
- What types of arrhythmias might it be used for?
- What are some of its side effects?
Quinidine
- Oral/IV
- Atrial fibrillation, atrial flutter, tachycardia, Brugada syndrome (irregular beats in ventricles)
- Side effects: hypotension, pro-arrhythmic
Give an example of a Class IB antiarrhythmic.
- How is it administered?
- What types of arrhythmias might it be used for?
- What are some of its side effects?
Lidocaine
- IV
- Ventricular tachycardia due to ischaemic heart disease
- Abdominal upset
Give an example of a Class IC antiarrhythmic.
- How is it administered?
- What types of arrhythmias might it be used for?
- Who is it contraindicated for?
- What does it need to be used with?
Flecainide
- Oral/IV
- Used for:
- Supraventricular fibrillation
- Wolff-Parkinson-White syndrome
- Contraindicated: ischaemic heart disease
- Use with AVN blocker- can increase ventricular response
What anti-arrhythmic would you prescribe for a patient with ectopic beats?
Beta blockers
How would you go about managing a patient with atrial fibrillation/flutter pharmacologically?
- First= rate controlling drugs (+digoxin to enhance vagal activity)
- Beta blocker
- Calcium channel blocker
- Second= rhythm controlling drugs for Cardioversion (restore normal sinus rhythm)
- Sodium blockers
- Potassium blockers
- Consider anticoagulants
- Aspririn
- Heparin
- Warfarin
If ACUTE- electrical/pharmacological cardioversion to restore sinus rhythm first
(digoxin= increases force of contraction)
What might we give to patients with tachycardic arrhythmias?
- Lidocaine is ischaemic heart disease (IB)
- Quinidine (IC)
- Beta blockers
- Calcium channel blockers
What drug do we give to patients with Wolff-parkinson-White syndrome?
Flecainide (Class IC- sodium blocker)
How does Ivabradine work as an anti-arrhythmic?
What are its specific indications?
Give a side effect of Ivabradine.
Who should Ivabradine NOT be given to?
- Blocks If (funny current)
- Slows sinus node
- Reduce HR in:
- Sinus tachycardia
- HF and angina
- Side effect: flashing lights
- AVOID in pregnancy = teratogenic

Ivabradine is an iF blocker. It slows the heart rate through its affect in the iF current. What is it particularly useful in treating?
- Heart failure
- Managing angina


