17 Anaesthetics Flashcards
How are anaesthetics administered IV?
Administer to:
- achieve plasma concentration at which specific end point reached (eg loss of eyelash reflex)
How?:
- Initial induction bolus
- Infusion system to maintain unconcious state

What does the blood:gas partition mean in terms of anaesthetics? What does a low value mean?
Blood:Gas partition= describes solubility of a volatile anaesthetic in blood
Low value= fast induction and recovery of patient
What does the Oil:Gas partition describe in terms of anaesthetics?
Oil:Gas partition: solubility in fat- determines potency
Why is it that it can take patients a long time to wake up if they have a high oil:gas partition?
Higher Oil:Gas partition- greater ability of anaesthetic to travel through fat
Anaesthetic can accumulate in fat - takes longer for patient to wake up
Give 3 examples of local/regional anaesthetics which can be used.
- Lidocaine
- Bupivacaine
- Ropivacaine
Administering anaesthetics involves the use of polypharmacy. What are the 6 steps involved?
- Premedication
- Induction
- Analgesia (usually opioid)
- Muscle paralysis
- Facilitate intubation
- Maintenance
- Typically gaseous
- Reversal and provision for PONV

Volatile anaesthetic potency is described in terms of minimum alveolar concentration.
What is the minimum alveolar concentration? (with relation to anaesthetics)
[Alveolar] (at 1atm) at which 50% of subjects fail to move to surgical stimulus
At equilibrium [alveolar]=[spinal cord]
List some factors that increase MAC (anaesthetics). (4)
- Age
- Hyperthermia
- Pregnancy
- Alcoholism
Other anaesthetics and opioids decrease MAC. What substance is commonly added to other volatile anaesthetics to decrease the MAC (less of drug needed so less side effects) and why?
Nitric oxide added- venodilates

What stages do we use to describe the level at which anaesthetics are working? What are the different stages?

There are 3 types of targets which are targeted by anaesthetic drugs. What are these 3 targets?
- GABA receptors (most anaesthetics)
- NMDA Glutamate receptors
- Voltage Gated Sodium channels
How do anaesthetics that target GABA receptors work?
(modulate balance between Glutamate- excitatory and GABA- inhibitory)
- Cl- ions flow into cell
- Cell hyperpolarises
- Can’t produced AP
- Depressed neural activity
Depressed reticular system inc:
- Hippocampus- memory
- Brainstem- CVS and resp
- Spinal cord- analgesia
What compounds act on NMDA Glutamate receptors as anaesthetics?
Xenon (good neuroprotective anaesthetic)
N2O
Ketamine
(glutamate used to wake patients up)
How do voltage gated sodium channel blockers work as anaesthetics?
(usually local anaesthetics)
Local anaesthetics-charged once inside cell
Charged agents blocks voltage gated soidum channel
Channel blocked- Na can’t pass through
AP can’t be achieved

What are the 2 ways we can administer general anaesthetics?
- Inhalation (volatile)
- Intravenous
What is conscious sedation and how is it carried out?
Use of small amounts of anaesthetic or benzodiazapines to produce ‘sleepy’ state (maintain verbal contact but feel comfortable)
Give some examples of IV anaesthetics.
- Propofol
- Barbiturates
- Etomidate
- Ketamine
Anaesthesia is a combination or 4 effects on the body. What are these 4 effects?
- Analgesia
- Hyponosis (LOC)
- Depression of spinal reflexes
- Muscle relaxation
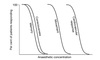
In what order are the following functions lost as anaesthetic concentration increases?
- Cardiovascular response
- Conciousness
- Movement
- Memory
Memory
Conciousness
Movement
CVS response
How do the loacl anaesthetics esters and amides differ in terms of length of action?
Esters= short acting
Amides= long acting



