Week 6 Flashcards
(171 cards)
What are the three clinically important lipids?
- Triglycerides- most common form of stored energy in mammals, derived from either dietary sources or endogenous hepatic production
- Cholesterol- the main sterol in animal tissues
- Fatty acids- these are relatively simple and important components of other lipids
What are sterols?
also known as steroid alcohols, are a subgroup of the steroids and an important class of organic molecules. They occur naturally in plants, animals, and fungi, with the most familiar type of animal sterol being cholesterol.
Why are cholesterol and triglycerides transported as macromolecular complexes? What are they called?
Because lipids are insoluble in water, they cannot be transported in aqueous solutions such as blood plasma. The macromolecular complexes are called lipoproteins.
What is the structure of a lipoprotein?
Spherical structures consisting of a lipid core (triglycerides and/or cholesterol esters) and an amphophilic outer layer of phospholipids, free cholesterol and proteins.

How are free fatty acids transported?
Bound to albumin
Why is hydrolysis?
The cleavage of chemical bonds by the addition of water. For example, carbohydrate is broken into its component sugar molecules by hydrolysis, e.g. sucrose being broken down into glucose and fructose
What are chylomicrons? What is the process by which they form? Where do they go??
* Following digestion, hydrolysis products (mainly fatty acids and monoglycerides) are converted to triglycerides in the intestinal mucosa cells–> then combined with phospholipids, cholesterol, and apolipoprotein to form CHYLOMICRONS. Chylomicrons are transported to the LIVER (and other tissues)

Endogenously produced triglycerides and cholesterol are transported from what organ, in what form?
Endogenously produced triglycerides and cholesterol are transported from the liver as very low density lipoproteins (VLDL) and cholesterol transported also as LDL.
What causes triglycerides to be released?
The activity of lipoprotein lipase, an enzyme located on the endothelium in many different tissues, for uptake as free fatty acids into e.g. fat or muscle
What facilitates the uptake of triglycerides from chylomicrons into the liver?
Hepatic lipase on the endothelium of the liver sinusoids
What causes the release of fatty acids? And where do they go? How are they transported?
Fatty acids are released from stored triglycerides in fat cells by the action of hormone sensitive lipase, under sensitive regulation by hormones.
The fatty acid are transported to the LIVER as non-esterified fatty acids (NEFA) bound to albumin

What is the funtion of insulin?
* Promotes the esterification (storage) of glycerol and free fatty acids into triglycerides within adipose tissues.
* Insulin also increases the activity of lipoprotein lipase located on the endothelium of capillaries of extrahepatic tissues, promoting the movement of fatty acids into adipose tissue

Thyroid tumours in dogs vs. cats
Dogs = carcinoma, poor prognosis
Cats= benign, good prognosis
What are Heinz bodies?
Oxidatively damaged Haemoglobin

Heinz bodies- could indicate hyperthyroidism
What changes will we see on haemogram (CBC) for hyperthyroidism?

What changes will we see for serum biochemistry related to liver enzymes in hyperthyroidism?

What changes (not related to liver enzymes) will we see in serum biochemistry with hyperthyroidism?

What is the initial test of choice for hyperthyroidism?
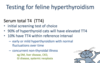
What are the options if the TT4 is within reference interval but hyperthyroidism is still suspected based on clinical signs and base-line testing?

Why is T4?
Thyroxine
Total T4 vs. Free T4
* TT4 bound to protein
* T4= free T4= < 1%
What is important to remember with cats and hyperthyroidism and renal function?

Hypothyroidism occurence in dogs and cats