Week 5 Flashcards
(144 cards)
What does the adrenal cortex synthesize?
Two classes of hormone corticosteroids (glucocorticoids and mineralocorticoids) & androgens
What are mineralocorticoids?
Electrolyte-balance regulating e.g. aldosterone which regulates K+ and Na+ levels in the distal tubules of the kidney, causing them to absorb more sodium and water from the urine… therefore more potassium is secreted in exchange
** stimulates H+ secretion in the collecting duct, regulating plasma bicarbonate and acid/base balance
* can also act on the CNS via the posterior pituitary gland to release ADH- conserves water by direct actions on renal tubular resorption
What do glucocorticoids do?
* essential for survival in a fasting animal
* cortisol is a glucocorticoid that affects carbohydrate and protein metabolism
* Protects glucose dependent tissues e.g. brain & heart
* Increases plasma glucose by enhancing mobilizaton of amino acids from proteins in many tissues
* Enhances the ability of the liver to convert these amino acids and glycerol into glucose by activating gluconeogenesis and to store glucose as glycogen
* In the periphery, glucocorticoids diminish glucose utilization and uptake, activate lipolysis, and increase protein breakdown
* Targets most body tissues, including CNS, bone, skin, liver, fat, and muscle
What is an example of an androgen precusor and function?
dehydroepiandrosterone (DHEA)- converted to testosterone and estradiol in peripheral tissues
What are the three zones of the adrenal cortex and each function?
- Zona glomerulosa- produces aldosterone
- Zona fasiculata- produces cortisol and androgens
- Zona reticularis- produces cortisol and androgens




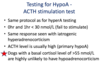
What regulates glucocorticoid secretion?
Regulated via hypothalamus- pituitary axis- CRH & ACTH
* CRH is released as a consequence of hypoglycaemia, stress, physical trauma, hypoxia, ADH, infection and diurnal secretion (dogs and cats episodic release)
** CRH binds cell surface receptors on corticotrophs and via G proteins and cAMP releases ACTH from the anterior pituitary
** Feedback inhibition– cortisol inhibits pituitary and hypothalamus. ACTH inhibits neuronal cells in the hypothalamus.

How are adrenocortical hormones transported and removed?
* Transported in the blood bound to globulin (trancortin) and albumin. 90% of glucocorticoids are bound to protein and have a relatively long half life ~60-90 minutes
* Inactivated by the liver, conjugated with sulphates and glucuronides- decreasing their ability to bind to blood proteins and makes them more water soluble- for excretion in the urine
What is the steroid mechanism of action?
* Cortisol and aldosterone bind to glucocorticoid receptor (GR) or mineral corticoid receptors (MR) in the cytoplasm that translocate to the nucleus and modulates transcription in multiple tissues after hormonal binding
What are metabolic actions of glucocorticoids?
* Defence against hypocalcaemia: raise blood glucose by increasing liver output of glucose
- decrease utilization of glucose by muscle and adipose tissue
- promotes gluconeogenesis (by inducing synthesis of enzymes)
- promotes proteolysis and inhibits protein synthesis to free up amino acids for gluconeogenesis
- liver synthesis of enzymes involved in the metabolism of amino acids- facilitating conversion to carbohydrates
- In muscle facilitating break down of muscle protein therefore providing amino acid substrate to the circulation and to the liver
* Mobilization of fat from subcutaneous adipose tissue
* Enhance release of glucagon from pancreas alpha cells
* Antagonizes the action of insulin on muscle and adipose tissue
* cortisol must be present for catecholamines to stimulate hormone sensitive lipase
Glucocorticoids and inflammation
* inhibit PGs and Leukotriene production (from endothelial cells, macrophages, mast cells, etc.)
* decrease release of pro-inflammatory cytokines (IL-1, IL-6, TNF-alpha)
* Reduces IL-2 production therefore inhibiting lymphocyte proliferation
* Reduced proliferation of fibroblast- therefore slow wound healing
What is Cushing’s Disease?
Hyperadrenocorticism
* Excess secretion of corticosteroids due to:
- pituitary tumour (85% of cases) over secreting ACTH- normally have two large adrenal glands
- Adrenal tumour
- excess administration of cortico-steroids (iatrogenic) (cortisone = cortisol, predinisone 4 x cortisol, dexamethasone 30 x cortisol)
What are the symptom’s of Cushing’s Disease?
* Bulging sagging (pot-bellied) belly
* muscle weakness, loss of muscle mass
* Hair loss and thinning of skin
* weak bones
* bruising
* polyphagia
* PU/PD
* poor wound healing
* Weight gain or redistribution of fat
* susceptibility to infections particularly bladder
* exercise intolerance
Why are about 10-20% of dogs with Cushing’s Disease also Diabetic?
* Glucocorticoids decrease utilization of glucose by muscle and adipose tissue and lower sensitivity of these tissues to insulin
What is Addison’s disease?
* Insufficiency of adrenocortical hormones
* Rare- autoimmune disease
* Signs: lethargy, weakness, dehydration, collapse
* Low plasma Na+, increased K+, increased BUN (blood urea nitrogen)
What does the adrenal medulla secrete? What is the medulla?
* catecholamines: adrenalin and noradrenalin (short half life 10-15 seconds- up to 90% of catecholamines removed from blood on single passage)
* medulla is a modified ganglion- a component of the sympathetic NS
What are the major stimuli of the adrenal medulla? How?
* hypoglycaemia, stress, and exercise
* Stimulation of nicotinic ACh receptors opens Ca2+ ion channels on chromaffin cells that produces a localized depolarization and entrance of Ca2+ resulting in exocytosis of adrenaline and noradrenaline
Where and from what are adrenalin and noradrenalin synthesized?
Chromaffin cells
* Tyrosine, dopa, dopamine, noradrenalin, adrenalin
What are the functions of adrenoceptors?
alpha- 1: increased vascular smooth muscle contraction, mydriasis (constricts radial muscle)
alpha-2: muscle relaxation, sedation, and analgesia (effects on CNS), hypertension, vasoconstriction of arteries to the heart
Beta 1: heart and kidney- increased force cardiac contraction and heart rate, renin release
Beta 2: bronchodilation by relaxation of smooth muscles in bronchi, uterine muscle relaxation, liver- glucose metabolism, smooth muscle relaxation
Beta 3: enhanced lipolysis
Metabolic actions of adrenalin

Where do large emobli tend to become trapped in the brain? Why are venous occlusions uncommon in the brain?
* Leptomeningeal vessels (where they divide into perpendicular branches)
*at the grey-white matter junction
* venous occlusions are rare because verebral veins are abundant and have many anastamoses
What is diploe?
Spongy bone present between two layers of compact bone in the parietal, occipital, and temporal bones of the skull– one of the ways the skull can absorb considerable shock forces (cranial sutures help too and the internal bony ridges of the skull)
What are the factors that influence the consequences of skull trauma?
Physical rigidity of bone (age, nutrition, presence of metabolic disease), mass, velocity, and direction of the applied force, the ability of the impacted tissues to move in response to the applied force