Vascular Anatomy Flashcards
What is the aorta?
Largest artery in the body
Receives cardiac output form the left ventricle
Distributes blood via the systemic circulation
What are the sub-divisions of the aorta?
Ascending
Arch
Descending (thoracic)
Abdominal

Where does the aorta terminate?
Terminates at L4 (vertebral level) where it divides (bifurcates) into two terminal branches:
Right and Left Common iliac arteries
What are the 5 general classes of blood vessels?
Arteries – arterioles – capillaries – venules – veins
What is the difference between arteries, capillaries and veins?
ARTERIES
Away from heart
Relatively thick muscular wall
Resilient
Arterioles
Oxygenated blood (mostly)
VEINS
Body –> heart
Thin walls
Valves (due to low pressure)
Venules – collect blood from capillary bed
Venous plexuses
Deoxygenated blood (mostly)
CAPILLARIES
Connect arterioles to venules
1 cell thick walls
Important exchange site between blood and surrounding interstitial fluid
What are the key features of arteries?
Elastic and contractile
Responds to changes in blood pressure
Under autonomic control: vasoconstriction and vasodilation
Classification:
Elastic
Muscular
Resistance
What is the importance of elastic arteries?
Aorta and branches – distinguished by greater elasticity
Helps to smooth out fluctuations in BP
Systole: elastic laminae are stretched, reducing BP
Diastole: elastic rebound helps to maintain arterial pressure
What are the layers of the artery?
Tunica intima (TI) may grow with age (arteriorscleorosis)
Tunica media (TM) thickest layer
•Smooth muscle cells
•Elastin
Tunica adventitia (TA) thin connective tissue •Collagen prevents elastic arteries from stretching beyond physiological limits
Vasa vasorum (vv) ‘vessels of the vessels’

What’s the difference between muscular and resistance arteries?
MUSCULAR
Majority of arteries
Less elastic tissue; smooth muscle predominates in TM
TI smaller and TA larger than in elastic arteries
RESISTANCE
Small diameter arteries and arterioles
TM still relatively muscular
TA thinner and TI may disappear
Greatest change in BP between arterioles and capillaries
What are capillaries and what types are there?
Connect arterioles to venules – exchange of nutrients and waste between blood and tissue cells, + interstitial fluid
Single-layered, flattened endothelial cells
Fenestrated: bigger gaps between endothelial cells

What are the differences between arteries and veins?
ARTERIES
Carry blood away from the heart
Thicker wall/diameter ratio
Maintains circular profile
Resistant to higher pressure
No valves
VEINS
Carry blood to the heart (with the exception of portal systems connecting two capillary beds)
Thinner wall/diameter ratio (especially tunica media)
Often collapsed
Valves
Where does the aorta ascend and what arteries does it give off?
Ascending within pericardial sac from the aortic orifice
Gives off the right and left coronary arteries
Where does the aortic arch lie and where does it terminate?
Arch lies behind sternum, in front of the trachea
Arches upwards and backwards
Becomes continuous with descending aorta at level of sternal angle
End at vertebral level T4
What arteries does the aortic branch into? (in order)
Brachiocephalic trunk (divides into right subclavian and right common carotid
Left common carotid
Left subclavian

What do the branches of the aortic arch branch into?
Brachiocephalic trunk = right subclavian artery and right common carotid artery
Left common carotid = internal/external carotid arteries
Left subclavian = vertebral artery

What provides the blood supply to the head and neck?
Majority from carotid and vertebral arteries
Right common carotid: frrom Brachiocephalic trunk
Left common carotid: directly from aortic arch
Both ascend up the neck and bifurcate into internal and external carotid (L and R) at C4
At what point do the left and right common carotid arteries bifurcate?
Both ascend up the neck and bifurcate into internal and external carotid (L and R) at C4

What do the external and internal carotid arteries each supply?
EXTERNAL CAROTID: artery supplies the areas of the head and neck external to the cranium
The artery ends within the parotid gland by dividing into the superficial temporal artery and the maxillary artery
INTERNAL CAROTID: enters the skull and via the carotid canal and supplies the brain, eyes and forehead
How do vertebral arteries enter the brain?
Vertebral arteries arise from the subclavian arteries and enter the cranium via the foramen magnum to eventually supply the brain
Label the arteries of the trunk


At what point do the common iliac arteries arise?
At L4 where aorta bifurcates into left and right common iliac arteries
What 3 key structures pass through the diaphragm and at what levels?

IVF T8: inferior vena cava, comes directly through tendon
Aorta- behind diaphragm at T12
(if it was through musuclar part of diaphragm, would compress the blood vessel)
Oesophagus: T10

Label the arteries


How is the blood supply delivered to the upper limbs?
The arterial supply to the upper limb is delivered via five main vessels (proximal to distal):
Subclavian
Axillary
Brachial
Radial
Ulnar
What is the pathway of the upper limb arteries?
Subclavian is a branch (either indirectly or directly) of the aortic arch
Becomes Axillary artery –> Passes deep to the Pectoralis minor muscle of the chest wall –> Forms anastomoses around the neck of the humerus
Continues as the Brachial artery –> Main blood supply to arm –> Descends down the arm into the cubital fossa and bifurcates into the radial and ulnar arteries of the forearm
Radial and Ulnar arteries anastomose around the hand – ‘Palmar arches’

What is the femoral triangle?
Femoral triangle: a wedge-shaped depression formed by muscles in the upper thigh at the junction between the anterior abdominal wall and the lower limb
The femoral nerve, artery, and vein and lymphatics pass between the abdomen and lower limb under the inguinal ligament (lower border of the oblique abdominal muscles) and in the femoral triangle

Identify the structures labelled as 1, 2 and 3.


Identify these structures

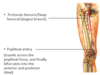
What is the popliteal fossa?
The popliteal fossa is a diamond-shaped depression located posterior to the knee joint.
Important nerves and vessels pass from the thigh to the leg by traversing through this fossa.
These include the two terminal branches of the sciatic nerve, the popliteal vessels and short saphenous vein.
Several muscles of the thigh and leg form the boundaries of the popliteal fossa.
They include the semimembranosus, semitendinosus, biceps femoris, gastrocnemius and popliteus muscles.
What structure do the two terminal branches of the sciatic nerve, the popliteal vessels and short saphenous vein traverse through?
Popliteal fossa
What are the arteries of the leg?
Popliteal
Posterior tibial
Anterior tibial
Dorsalis pedis

What are the veins of the lower limb divided into? What is the difference between them?
DEEP VEINS and SUPERFICIAL VEINS
Deep veins are located underneath the deep fascia of the lower limb, accompanying the major arteries.
Superficial veins are found in the subcutaneous tissue. They eventually drain into the deep veins.
What veins run in subcataneous tissue?
Superficial veins of the lower limb (great and small saphenous veins)
What are the two major superficial veins?
The Great Saphenous Vein = ascends up the medial side of the leg, passing anterior to the ankle, and posteriorly at the knee
The Small Saphenous Vein = moves up the posterior side of the leg, and empties into the popliteal vein in the popliteal fossa

When does the external iliac artery become the femoral artery?
When it passes under the inguinal ligament in the femoral triangle
Running medial to lateral what are the positions of the femoral nerve and blood vessels in the femoral triangle?
Medial: femoral vein
Middle: femoral artery
Lateral: femoral nerve
What is the importance of skeletal muscles in circulation?
Valves in the veins prevent backflow of blood
Contracting muscles compress veins, forcing blood towards the heart
Skeletal muscle that aids the heart in the circulation of blood
Increases venous return to heart

What are pulse points and where are they found?
Tactile, arterial palpation of the heartbeat peripheral pulse point
Compression of an artery against a bone
FOUND IN: Head and neck, Lower limb, Upper limb
Describe the anatomical position of the brachial artery pulse
The brachial pulse is in the midarm
The brachial artery lies on the medial side of the arm in the cleft between the biceps brachii and triceps brachii muscles.
This is the position where a blood pressure cuff is placed.
What is the anatomical position of the radial artery pulse?
The radial artery at its distal end of the forearm (i.e. before the wrist) lies on the anterior surface and is only covered by skin and fascia
This is a common place to measure the pulse rate of a patient as a means to assess heart rate, cardiac rhythm and pulse strength
The radial artery lies superficially in front of the distal end of the radius, between the tendons of the brachioradialis and flexor carpi radialis; it is here that clinician takes the radial pulse
How else can you take the radial pulse?
Can also take a radial pulse in the anatomical snuffbox where the radial artery crosses the lateral side of the wrist between the tendon of the extensor pollicis longus muscle and the tendons of the extensor pollicis brevis and abductor pollicis longus muscles.
What is the anatomical position of the ulnar pulse?
The ulnar pulse can be located in the distal forearm
The ulnar artery lies immediately under the lateral margin of the flexor carpi ulnaris tendon and proximal to the pisiform
What are 3 points of clinical significance of the femoral triangle?
The femoral artery is palpable as it passes over the femoral head and may be easily demonstrated using ultrasound.
If arterial or venous access is needed rapidly, a clinician can use the femoral approach to these vessels
Many radiological procedures involve catheterisation of the femoral artery or the femoral vein to obtain access to the contralateral lower limb, the ipsilateral lower limb, the vessels of the thorax and abdomen, and the cerebral vessels.

What is the clinical significance of the femoral triangle in relation to catheterisation?
Cardiologists also use the femoral artery to place catheters in vessels around the arch of the aorta and into the coronary arteries to perform coronary angiography and angioplasty.
Access to the femoral vein permits catheters to be maneuvered into the renal veins, the gonadal veins, the right atrium, and the right side of the heart, including the pulmonary artery and distal vessels of the pulmonary tree.
Access to the superior vena cava and the great veins of the neck is also possible.
Arteries are made up of 3 layers
- Intima: includes the endothelium a layer of cells which are continuous with the endocardium, a layer of loose connective tissue the internal elastic lamina.
- Media: Is mainly smooth muscle surrounded by varied numbers of collagenous, reticular and elastic fibers.
- Adventitia: A thin layer of connective tissue with some elastic fibers
What 3 layers make up the veins?
- Intima: Composed of endothelium with some connective tissue.
- Media: Is reduced in comparison to a similar sized artery and has only occasional smooth muscle cells.
- Adventitia: This makes up the majority of the vessel wall, with collagen, smooth muscle and some elastic fibers.
What are the different types of arteries?
Muscular
Elastic
Arterioles
Muscular arteries
Muscular arteries
The media contains little elastin, and is mainly composed of smooth muscle.
The adventitia is made up of collagenous and elastic fibers.
EVG stains them yellow
Elastic arteries
Elastic arteries
This is a section through the aorta. The most prominent layer is the media which is composed of concentric layers of elastic fibers separated by smooth muscle and collagen.
Elastic arteries receive blood directly from the heart and therefore are subject to high and varying blood pressures. The elastic tissue in the media provide recoil, helping to maintain and smooth out the pressure wave from the heart contracting.
EVG stains them black
Arterioles
Arterioles
The intima is reduced to the endothelium cells lying on a basement membrane on top of the internal elastic membrane.
In larger arterioles the media contains one or two layers of smooth muscle, as the arterioles get smaller this reduces to a discontinuous layer.


