Valvular and Congenital Heart Disease - Nichols and Newman Flashcards
What are the two forms of cardiac adaptation to valvular disease? How is this different in acute scenarios?
-
Concentric hypertrophy: pressure overload = STENOSIS (+ HTN)
1. INC thickness (thich walls), but normal volume -> LV hypertrophy -
Eccentric hypertrophy: volume overload = REGURGITATION
1. INC dilation of chamber (more volume + thin walls) -> INC output (Starling) -
Acute: no time to adapt, so pt presents severely ill
1. Murmur heard, but no concentric or eccentric hypertrophy - INC pressure change with DEC structural changes in acute OR DEC pressure change with INC structural changes in chronic
Mitral valve stenosis
- Rheumatic fever
- INC pressure behind mitral (stenosed) valve: concentric hypertrophy + dilation of LA (THROMBI), pulmonary HTN (atherosclerosis), concentric hypertrophy of RV
- Presentation: shortness of breath, alveolar fluid w/fibrinous material, hemoptysis (if chronic), right heart failure, afib (stroke), dysphagia (atrium compresses back on esophagus)
- Murmur: diastolic

Mitral valve regurgitation
-
Mitral valve prolapse, LV dilation (left sided heart failure dilates mitral valve ring), rheumatic fever
1. Prolapse: leaflets replaced by myxomatous (spongy) tissue; eccentric hypertrophy (dilation) of LA - Presentation: can be asymptomatic with murmur, sudden rise in atrial pressure, INC preload (from atrium) + DEC afterload (from venting) = INC stroke volume
- Acute = no change in RA volume, INC pulmonary capillary wedge pressure (lg pressure buildup)
- Murmur: pansystolic

What are the epi, patho and sign of mitral valve prolapse?

- Epi: most common valvular disease (about 2% of US population); primary or secondary
- Pathogenesis: primary form a genetic defect in connective tissue; secondary form injury
- Gross: redundant, billowing, ballooning, hooding, floppy leaflets, +/- elongated chordae tendineae (that can rupture)
- Microscopic: sometimes degeneration of and attenuation of outer zona fibrosa, and expanded myxomatous inner zona spongiosa (often normal)
- Sign: mid-systolic click
What are 1, 2, and 3?

- Normal mitral valve
1. Zona atrialis (sometimes also called zona fibrosa)
2. Zona spongiosa
3. Zona fibrosa
What do you see?

Expanded, myxomatous zona spongiosa (e.g., in mitral valve prolapse)
What are the epi and patho of Libman-Sacks endocarditis?

- Epi: lupus
- Gross: small-medium verrucous, berry-like or flat vegetations, commonly on multiple valves (on either or both sides)
- Microscopic: necrotic debris, fibrinoid material, degenerating leukocytes, fibroblasts, and hematoxylin bodies
- Clinically important fact: rarely embolizes
How is endocarditis related to valve pressure?
- Incidence of infection, marantic endocarditis, and rheumatic disease on a valve correlate with resting pressure on the closed valve:
1. Mitral: 116 mm Hg
2. Aortic: 72 mm Hg
3. Tricuspid: 24 mm Hg
4. Pulmonic: 5 mm Hg
Why is it really important to “catch” infective endocarditis?
100% fatal if undiagnosed/untreated, but only 20% fatal if diagnosed/treated appropriately (IV AB’s, sx)
What is the pathogenesis of infective endocarditis (4)?
- Most commonly of the valves, w/vegetations -> friable masses of infecting organisms and blood clot
1. Valvular endo injury
2. Platelet + fibrin deposition
3. Microbial seeding
4. Microbial multiplication - NOTE: valves may be “grossly normal,” but steps 1 and 2 precede 3 and 4
What valves, etiologic agents, and portals of entry are generally involved in infective endocarditis?
- Valves: mitral > mitral + aortic = aortic > tricuspid (only 1% pulmonic)
- Etiologic agents: staph aureus (acute) and strep viridans (sub-acute; followed by enterococcus)
What do you see? Why is this important?

- Central venous catheterization
- Portal of entry of bugs in infective endocarditis
What do you see? Why is this important?

- Mouth with gingivitis, brushing teeth, chewing, dental procedures -> all portals of entry for bugs in infective endocarditis
What is the gross pathology of infective endocarditis?

-
Vegetations: large (up to 3cm), friable, single or multiple, tan, grey, or red brown
1. Usually on line of valve closure (atrial side of AV valves, and ventricular side of semilunar valves) - The larger a vegetation, the more likely it is infective
- Destructive, and may cause: perforation of valve, adjacent abscess, fibrotic scarring, or calcification
- Infected (septic) emboli from endocarditis commonly go to kidney, heart, spleen, brain
What are the microscopic pathology and common symptoms/signs of infective endocarditis?
-
Microscopic pathology:
1. Fibrin, platelets, masses of organisms, +/- necrosis, +/- neutrophils
2. Later: +/- lymphos, macros, fibroblasts, fibrosis - Symptoms: fever, chills, weakness, dyspnea
- Signs: fever, heart murmur, splenomegaly, petechiae
What do you see?

- Osler nodes in fingers: tender to the touch
- Sign of infective endocarditis
What do you see?

- Splinter hemorrhage under fingernail (aka, subungual splinter hemorrhages)
- Sign for infective endocarditis, but not specific -> much more commonly due to trauma
What do you see?

- Janeway lesions: hemorrhages on palms or soles (5%)
- Sign of infective endocarditis
What do you see?

- Roth spots: retinal hemorrhages due to infective endocarditis
What are the common lab findings and complications associated with infective endocarditis?
- Lab findings: high ESR, anemia, proteinuria (may also have Rheumatoid factor or hematuria)
- Complications: heart failure, septic emboli (to kidneys, heart, spleen, brain)
What tests/procedures are helpful in diagnosing infective endocarditis? Which of these is essential?

- Transthoracic echocardiography: 60% sensitivity for vegetations
1. Transesophageal echocardiography: >90% sensitive for vegetations
2. Absence of vegetations on echo does not exclude endocarditis dx - Murmur + echo + vegetations does NOT = dx -> need BLOOD CULTURES (essential for making specific dx to guide AB therapy)
1. Continuous low-grade bacteremia characteristic of infective endocarditis: 3 sites cultures, 30-60min apart before starting AB’s
2. Alert lab endocarditis suspected b/c some bac that cause endocarditis fastidious, or slow-growing, or both, so lab will use special culture media, and hold the cultures longer
What are the pluses and minuses of surgical valve replacement?

- Can be life-saving, esp. w/acute disease
- Immediate relief w/chronic disease, but replaces one chronic disease w/another -> mechanical valves require lifelong anti-coagulation
- Bioprostheses deteriorate, with structural failure in up to 50% by 10 years, accelerating after that
- Complications include: leak, thrombosis, embolism, bleeding, and endocarditis
- Critical to make sure patients understand these risks/complications from the outset
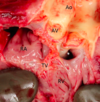
What do you see?

- Infective endocarditis: remember, fever + heart murmur = infective endocarditis (until proven otherwise)
- Mitral valve identifiable by chordae tendineae going to both leaflets (not aortic valve)
- Very large, extensive vegetations involving about 80% of leaflets (bigger the vegetations, the more likely they are infective)
- NOT mitral valve prolapse b/c many cases have valves that are microscopically normal; it is just too big. Even those with myxomatous change tend to have a normal surface -> inner zona spongiosa expanded, while outer zona fibrosa may be thinned, but is otherwise normal
- Size and extent of these very large, very extensive vegetations goes against marantic endocarditis
What is a probe-patent foramen ovale (often shortened to foramen ovale)?

- About 20% of ppl have membranous flap of tissue over foramen ovale that can be opened by pushing a probe on it
- Normally, higher pressures on left side of heart keep flap in place, maintaining separateness of left and right heart circulations
1. If pressures on right side ever rise to level higher than left, can act like probe and push open foraman ovale b/t right and left atria, letting deoxygenated blood skip passing through lungs