UWSA1-2 Flashcards
(264 cards)
A 67-year-old man comes to the emergency department due to progressive weakness and numbness in his feet over the past month. The patient has had difficulty maintaining balance when walking and reports generally feeling weak. He has a history of alcohol use disorder and has been hospitalized for alcohol intoxication. Neurologic examination shows decreased tactile and vibratory sensation in the feet and ankles bilaterally. Gait is unsteady, and muscle strength is mildly decreased in both lower extremities. Lower extremity deep tendon reflexes are hyperactive, and Babinski sign is present bilaterally. Which of the following is the most likely cause of this patient’s current neurologic symptoms?
Cobalamin Deficiency
Subacute Combined Degeneration pathophysiology
The constellation of progressive neurologic symptoms and upper motor neuron signs (eg, hyperreflexia, Babinski sign) is suspicious for subacute combined degeneration. This myelopathy affects both ascending and descending pathways in the spinal cord and is associated with vitamin B12 (cobalamin) deficiency.
Vitamin B12 is a water-soluble vitamin found in animal-derived foods. Although liver stores are generally sufficient for several years, vitamin B12 deficiency can develop over time in patients with consistently poor intake (eg, strict vegan diet) or poor absorption (eg, pernicious anemia, chronic alcohol use).
Vitamin B12 is essential for DNA synthesis and repair, as well as myelin generation and maintenance (via methylation of neuronal lipids/proteins). Therefore, deficiency usually manifests with hematologic (eg, megaloblastic anemia) and/or neurologic abnormalities. Axonal damage within the spinal cord and peripheral nervous system is associated with motor and sensory deficits:
Dorsal columns: diminished tactile/vibratory sensation and proprioception (Romberg sign)
Lateral corticospinal tracts: muscle weakness, hyperreflexia, Babinski reflex, spastic paresis
Spinocerebellar tracts: diminished proprioception, sensory ataxia
Peripheral nervous system: paresthesia
For most patients, neurologic recovery following vitamin B12 supplementation is slow and variable.
Subacute Combined Degeneration S&S
- The constellation of progressive neurologic symptoms and upper motor neuron signs (eg, hyperreflexia, Babinski sign) is suspicious for subacute combined degeneration. This myelopathy affects both ascending and descending pathways in the spinal cord and is associated with vitamin B12 (cobalamin) deficiency.
- Vitamin B12 is essential for DNA synthesis and repair, as well as myelin generation and maintenance (via methylation of neuronal lipids/proteins).
- deficiency usually manifests with hematologic (eg, megaloblastic anemia) and/or neurologic abnormalities.
- Axonal damage within the spinal cord and peripheral nervous system is associated with motor and sensory deficits:
- Dorsal columns: diminished tactile/vibratory sensation and proprioception (Romberg sign)
- Lateral corticospinal tracts: muscle weakness, hyperreflexia, Babinski reflex, spastic paresis
- Spinocerebellar tracts: diminished proprioception, sensory ataxia
- Peripheral nervous system: paresthesia
Subacute Combined Degeneration Tx
For most patients, neurologic recovery following vitamin B12 supplementation is slow and variable.
Amyotropic Lateral Sclerosis vs Subacute Combined Degeneration
Amyotrophic lateral sclerosis is a neurodegenerative disorder that affects both upper and lower motor neurons and often presents with asymmetric limb weakness and incoordination. However, sensory pathways are rarely affected, and loss of tactile/vibratory sensation would be unexpected in Subacute Combined Degeneration.
Cerebellar Degeneration vs Subacute Combined Degeneration
Cerebellar degeneration in patients with extensive alcohol use is caused by damage to Purkinje cells in the cerebellar cortex and can lead to gait impairment (incoordination similar to that seen in alcohol intoxication). However, tactile/vibratory sensation loss and upper motor neuron signs (eg, hyperreflexia, Babinski reflex) would not be expected.
Subacute Combined Degeneration vs Thaimine Deficiency
Thiamine deficiency can cause peripheral neuropathy leading to gait impairment; thiamine deficiency can also cause Wernicke encephalopathy (ie, ataxia, confusion, oculomotor dysfunction).
However, SCD neurologic symptoms include upper motor neuron signs (eg, hyperreflexia, Babinski reflex), which are not seen with thiamine deficiency.
Vitamin B12 role in Subacute combined Degeneration
Vitamin B12 (cobalamin) deficiency can cause subacute combined degeneration of the spinal cord due to impaired myelination in the dorsal columns (causing diminished tactile/vibratory sensation and proprioception) and lateral corticospinal tracts (causing hyperreflexia, Babinski reflex, spastic paresis).
Myasthenia gravis Pathophysiology
- Autoantibodies against acetylcholine receptors at motor endplate
- Thymus involved in autoimmunity:
- Thymic hyperplasia
- Thymoma
myasthenia gravis (MG), an autoimmune disease that affects acetylcholine receptors (AChRs) in the postsynaptic membrane of the neuromuscular junction. Thymic abnormalities are extremely common in patients with MG and include thymic hyperplasia or thymomas. The thymus is thought to be the site of autoimmunization in MG and contains muscle-like cells that express AChRs. Abnormal antigen-presenting cells within the thymus process AChRs, allowing for priming of helper T cells and recruitment of B cells to form AChR antibodies. This leads to a decrease in the number of functional AChRs with resultant fatigable musculoskeletal weakness.
Myasthenia Gravis S&S
- Fluctuating & fatigable proximal muscle weakness; worse later in the day
- Ocular (eg, diplopia, ptosis)
- Bulbar (eg, dysphagia, dysarthria)
- Respiratory muscles (eg, myasthenic crisis)
intermittent diplopia, bulbar muscle weakness (eg, fatigue with chewing), and ptosis on examination likely has myasthenia gravis (MG)
Edrophonium test
A Tensilon test is a diagnostic test used to evaluate Myasthenia Gravis, which is a neuromuscular condition characterized by auto anti motor endplate acethylcholine receptor antibodies muscle weakness. The test involves an injection of Tensilon (edrophonium), after which your muscle strength is evaluated to determine whether your weakness is caused by myasthenia gravis or not.
Tensilon reverses the symptoms of myasthenia gravis. It works by preventing your acetylcholine from breaking down. It inhibits the enzyme that normally breaks down acetylcholine, acetylcholinesterase, allowing your acetylcholine to bind to the existing receptors as much as possible.
Improved weakness is a positive test for myasthenia gravis
Ice pack test
A test to check for Myasthenia Gravis
An ice pack is applied to the ptotic lid for 2 minutes, and ptosis is measured with a ruler before and after cooling. A rise of 2 mm is a positive result indicating Myasthenia Gravis
Myasthenia Gravis Tx
- Acetylcholinesterase inhibitors (eg, pyridostigmine)
- Thymectomy
Myasthenia Gravis Serology
anit acetylcholine receptor antibodies (AChRs) in the postsynaptic membrane of the neuromuscular junction

Thymoma

Lambert-Eaton myasthenic syndrome (LEMS) Pathophysiology
an autoimmune disorder of the neuromuscular junction caused by antibodies against voltage-gated calcium channels on the presynaptic membrane.
Lambert-Eaton Myasthenic syndrome Vs Myasthenia Gravis
LEMS resembles MG, but the weakness lessens rather than worsens with repeated stimulation and the limbs are typically affected more than the bulbar muscles.
Pituitary Adenoma common Presentation
Pituitary adenomas most often present with bitemporal hemianopsia (compression of the optic chiasm), headache (mass effect), and diplopia (oculomotor nerve compression). Hormone abnormalities (eg, hyperprolactinemia, Cushing disease, acromegaly) can also be seen.
Myasthenia Gravis Brief Description
Myasthenia gravis is an autoimmune disease that affects the postsynaptic acetylcholine receptors of the neuromuscular junction and presents with fatigable musculoskeletal weakness (particularly eye and bulbar musculature). Thymic abnormalities (hyperplasia, thymomas) are extremely common in patients with myasthenia gravis; patients often improve with thymectomy.
Retinoblastoma white reflex

Retinoblastoma Pathopgenesis
- The retinoblastoma (RB1) gene, a tumor suppressor gene that, when defective, predisposes to retinoblastoma.
- One copy of the RB1 gene is found on each chromosome 13.
- Both copies of the RB1 gene must be lost for tumorigenesis to occur. This concept reflects the Knudson “2-hit” hypothesis of tumorigenesis.
- Patients with sporadic retinoblastoma develop 2 spontaneous somatic mutations in a single retinal cell, resulting in a unilateral tumor.
- In contrast, patients with hereditary retinoblastoma are born with a germline defect in one of their RB1 genes. As a result, all their cells have the first “hit” required for tumor formation. An additional somatic mutation (eg, a loss of heterozygosity) early in life provides the second “hit” for malignant transformation.
- Patients with hereditary retinoblastoma are at increased risk for bilateral and multifocal retinoblastoma. They are also at risk for development of other primary malignancies, such as osteosarcoma, later in life.
Xeroderma Pigmentosum pathophys
- Defective DNA repair occurs in xeroderma pigmentosum, a heritable disease resulting from defective nucleotide excision repair that predisposes to early skin cancer of all forms
Partial Hydatidiform moles karyotype
Partial hydatidiform moles result from triploidy
(69XXX,
69XXY,
or
69 XYY)
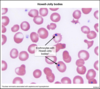
What is this?
Joint aspirate

Septoc Arthritis