UW6 Flashcards
(63 cards)
Question

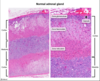
The adrenal gland is made up of an outer cortex (divided into 3 zones) and an inner medulla:
- The zona glomerulosa is the outermost zone of the cortex and is composed of cells arranged in rounded or arched clusters (glomus is Latin for ball) that secrete mineralocorticoid hormones (primarily aldosterone).
- The zona fasciculata is the middle zone and contains foamy-appearing cells in columns (fascis is Latin for bundle or stack) that secrete glucocorticoid hormones (primarily cortisol).
- The zona reticularis is the inner zone of the cortex and contains cells in anastomosing cords (rete is Latin for net) that secrete androgens.
The adrenal medulla is sharply demarcated from the cortex and is composed of chromaffin cells with a deeply basophilic cytoplasm.
Chromaffin cells are modified neuroendocrine cells derived from the neural crest. They are stimulated by acetylcholine released by sympathetic preganglionic neurons and secrete catecholamines (80% epinephrine, 20% norepinephrine) directly into the bloodstream to amplify sympathetic nervous system activity.

Zona Glomerulosa location and function
The zona glomerulosa is the outermost zone of the cortex and is composed of cells arranged in rounded or arched clusters (glomus is Latin for ball) that secrete mineralocorticoid hormones (primarily aldosterone).

Zona Fasiculata location and function
The zona fasciculata is the middle zone and contains foamy-appearing cells in columns (fascis is Latin for bundle or stack) that secrete glucocorticoid hormones (primarily cortisol).
Zona Reticularis location and function
The zona reticularis is the inner zone of the cortex and contains cells in anastomosing cords (rete is Latin for net) that secrete androgens.

Identify


Adrenal medulla location and function
The adrenal medulla is sharply demarcated from the cortex and is composed of chromaffin cells with a deeply basophilic cytoplasm.
Chromaffin cells are modified neuroendocrine cells derived from the neural crest. They are stimulated by acetylcholine released by sympathetic preganglionic neurons and secrete catecholamines (80% epinephrine, 20% norepinephrine) directly into the bloodstream to amplify sympathetic nervous system activity.

Question

This infant likely had Potter sequence, which is characterized by pulmonary hypoplasia, flat facies, and lower limb deformity (eg, club foot). Potter sequence is caused by a urinary tract anomaly that leads to decreased fetal urine output. It is classically associated with bilateral renal agenesis but can occur secondary to other etiologies, including posterior urethral valves or fetal exposure to ACE inhibitors.
Because fetal urine is the main component of amniotic fluid, decreased fetal urine output can lead to low or absent amniotic fluid levels (ie, severe oligohydramnios). Inadequate amniotic fluid levels allow for increased external compression of the fetal face (flat facies) and extremities (eg, club foot). In addition, the umbilical cord is often compressed such that fetal heart rate abnormalities (eg, recurrent decelerations) are common during labor.
Amniotic fluid also provides the fluid and growth factors needed for fetal lung development. Therefore, neonates with Potter sequence have pulmonary hypoplasia due to the lack of normal alveolar distension by aspirated amniotic fluid. Both lungs are affected, and respiratory failure (ie, hypoxia) is the most common cause of death in affected infants.

Fetal exposure to ACE inhibitors and ARBs

Causes of bilateral renal agenesis
potter sequence
Posterior urethral valves
ACE inhibitor or ARBs exposure
Question

B.
Beta blockers are the preferred treatment for patients with chronic stable angina and hypertension. They relieve anginal symptoms by inhibiting sympathetic stimulation of the heart, reducing both heart rate and contractility. Because beta blockers reduce heart rate and blood pressure during rest and exercise, the onset of angina is avoided or delayed.
At low doses, atenolol is a selective β1 adrenergic antagonist. β1 receptors are found in cardiac tissue and on renal juxtaglomerular cells, but not in vascular smooth muscle. The β1 receptor is a G protein-coupled receptor (GPCR) associated with Gs, which increases intracellular cAMP levels. Blockade of the β1 receptor leads to decreased cAMP levels in cardiac and renal tissue without significantly affecting cAMP levels in vascular smooth muscle (Choices C and D).
GPCRs comprise a large family of 7 transmembrane domain receptors that activate intracellular second messenger systems. There are 2 principal second messenger systems involving GPCRs:
cAMP signaling pathway: The activated Gs α subunit activates the enzyme adenylyl cyclase, which catalyzes the conversion of ATP into cAMP. Elevated cAMP leads to the activation of protein kinase A. Conversely, the Gi α subunit inhibits adenylyl cyclase, thereby reducing cAMP levels.
Phosphatidylinositol signaling pathway: The activated Gq α subunit activates phospholipase C, which degrades membrane lipids into diacylglycerol (DAG) and inositol triphosphate (IP3). Protein kinase C is activated by DAG, and calcium is released from the sarcoplasmic reticulum under the influence of IP3.
(Choice A) Propranolol is a nonselective beta blocker that blocks both β1 and β2 adrenergic receptors. β2 receptors are found in vascular and bronchial smooth muscle. Blockade of β1and β2 receptors would therefore result in decreased cAMP levels in cardiac myocytes, renal juxtaglomerular cells, and vascular smooth muscle.
(Choice E) A medication such as diltiazem, a non-dihydropyridine calcium channel blocker, would not directly affect cAMP levels.
Educational objective:
β1 adrenergic receptors are found in cardiac tissue and on renal juxtaglomerular cells, but not in vascular smooth muscle. Selective blockade of the β1 receptor (eg, with atenolol) leads to decreased cAMP levels in cardiac and renal tissue without significantly affecting cAMP levels in vascular smooth muscle.
G-protein coupled receptors and their signal transducers:
α1
Gq
G-protein coupled receptors and their signal transducers:
α2
Gi
G protein–coupled receptors & their signal transducers:
β1
Gs
G protein–coupled receptors & their signal transducers:
β2
Gs
G protein–coupled receptors & their signal transducers
M1
Gq
G protein–coupled receptors & their signal transducers
M2
Gi
G protein–coupled receptors & their signal transducers
M3
Gq
G protein–coupled receptors & their signal transducers
D1
Gs
G protein–coupled receptors & their signal transducers
D2
Gi
G protein–coupled receptors cAMP pathway
cAMP signaling pathway: The activated Gs α subunit activates the enzyme adenylyl cyclase, which catalyzes the conversion of ATP into cAMP. Elevated cAMP leads to the activation of protein kinase A. Conversely, the Gi α subunit inhibits adenylyl cyclase, thereby reducing cAMP levels.
G protein–coupled receptors Phosphatidylinisotol signaling pathway
Phosphatidylinositol signaling pathway: The activated Gq α subunit activates phospholipase C, which degrades membrane lipids into diacylglycerol (DAG) and inositol triphosphate (IP3). Protein kinase C is activated by DAG, and calcium is released from the sarcoplasmic reticulum under the influence of IP
Question

E. Cryptococcyus Neoformans

Cryptococcus neoformans is a yeast that has an antiphagocytic polysaccharide capsule, a major virulence factor. The polysaccharide capsule appears as a clear, unstained zone with India ink and stains red with mucicarmine (as seen in this patient). Methenamine silver stain can identify the yeast forms, seen in tissue as round cells with narrow-based buds.
C neoformans usually affects immunocompromised patients (eg, kidney transplantation patients on chronic immunosuppression). It is a neurotropic fungus that is transmitted via the respiratory route and most commonly presents with subacute or chronic meningoencephalitis. Cryptococcal lung disease can occasionally cause pneumonia-like symptoms, including cough with scant sputum production, pleuritic chest pain, dyspnea, and hemoptysis. Chest x-ray findings are nonspecific (eg, infiltrates, nodules). Diagnosis is usually confirmed by identifying Cryptococcus in sputum, bronchoalveolar washings, or tissue samples.
(Choice A) Aspergillus fumigatus can cause pulmonary disease and invasive aspergillosis, most commonly in immunocompromised patients. However, microscopy typically shows septate hyphae.
(Choice B) Blastomyces dermatitidis can cause both lung disease and disseminated mycosis. Its microscopic appearance in tissue is that of a round yeast with broad-based budding and a thick, doubly reflective wall.
(Choice C) Candida albicans most commonly causes oropharyngeal, mucocutaneous, and esophageal disease. It rarely causes pneumonia. Microscopy typically shows budding yeast with pseudo-hyphae.
(Choice D) Coccidioides immitis causes lung disease in immunocompetent individuals and disseminated mycosis in immunocompromised patients. In tissue samples, it appears as large, irregularly sized, thick-walled spherules that contain small, round endospores.
(Choice F) Histoplasma capsulatum is a dimorphic fungus that causes tuberculosis-like pulmonary disease. It can also cause disseminated mycosis in immunocompromised patients. It is found intracellularly in tissue (within macrophages), appearing as small, ovoid, and budding yeast cells.
(Choice G) Rhizopus species typically causes rhino-orbito-cerebral infection but can cause pulmonary disease, predominantly in immunocompromised patients. Histology typically shows broad hyphae with irregular branching and rare septations.
Educational objective:
Cryptococcus neoformans is the only pathogenic fungus that has a polysaccharide capsule. The capsule appears red on mucicarmine stain and as a clear unstained zone with India ink.
Aspergillus fumigatus causes and histology
Aspergillus fumigatus can cause pulmonary disease and invasive aspergillosis, most commonly in immunocompromised patients. However, microscopy typically shows septate hyphae.

Blastomyces dermatitidis causes and histology
Blastomyces dermatitidis can cause both lung disease and disseminated mycosis.
Its microscopic appearance in tissue is that of a round yeast with broad-based budding and a thick, doubly reflective wall.



















































