Urinaty Sytem Flashcards
In what structures do the kidneys lie?
Where does it originate from?
What does it contain?
Lie in dense fibrous capsule called renal fascia
It derives from the transversalis fascia
It contains fat (for protection) but also is continuous anteriorly and contains major blood vessels (IVC and Aorta)

At which spinal levels can the kidneys normally be found?
Hilum of the kidney at around L1 (for both)
Start at around T11/T12( left) or T12 (right)
–> Because of right kidney often lower
To which structure does the kidney relate superiorly?
The kidney relates superiorly to the diaphragm
What are the important anatomical structures the kidneys relate to posteriorly?
Which nerves run posteriorly to the kidney?
Diaphragm, transverse abdominis+ posterior abdominal muscles
–> all separated from the kidney by the transversalis fascia
Nerves:
- 11 intercostal nerve
- subcostal nerve
- Iliohypogastric nerve and Ilioinguinal nerve

Which structures doe the right kidney relate to anteriorly?
It lies behind the Hepatic flexure
The hilus of the kidney lies behind the 2nd part of the duodenum (curvature)

Which structures doe the left kidney relate to anteriorly?
It relates to different structures:
- Pancreas
- Stomach
- Spleen
- Splenic flexure (left upper curve of colon)

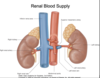
Summarise renal blood supply from the aorta and drainage into the IVC. Include the length of the vessels for the right and left kidney, and arrangement of blood vessels.
- Kidneys get directly supplied by short branches of the aorta (20-25% of resting CO)
- Drain into the IVC
Relations:
The aorta lies left and posterior to the IVC resulting in different blood vessel length:
Right kidney:
- long artery, shorter vein
Left Kidney:
- short artery, longer vein
How is the relation between the superior mesenteric artery and the left renal vein?
The left renal vein passes anteriorly over the aorta but is overlapped by the superior mesenteric artery originating superior to left renal vein

How are the blood vessels and the ureter /pelvis of kidney arranged in the hilum of the kidney?
From anterior to posterior
- Vein
- Artery
- The pelvis of Kidney (also inferior)

Summarise the structure of the kidney
Has a Cortex (outer part)
- granular appearance because of random organisation
And a Medulla
- Straited appearance because of radial arrangement of tubules and micro-vessels
The Medulla occurs in Lubules (Multi-lobular kidney in humans)
- Each medulla part of lobule is called Pyramid
- Each lobule has own calyx and renal papilla

What is the Calyx in the kidney?
Chambers of the kidney through which urine passes

What is the renal papilla?
It is the junction of the site where urine from medullary pyramids enters the calyx

Which route do the ureters take to get from the kideny to the bladder?
- Run vertically down posterior abdominal wall in the vertical plane of the tips of the transverse processes of the lumbar vertebrae
- Cross aorta at bifurcation of the common iliac arteries and the pelvic brim anterior to the sacroiliac joint
- Descend anteromediallyto enter bladder at the level of the ischialspine

How are the ureters supplied with blood?
Basically from every major vessel they cross:
- renal artery
- gonadic artery
- common iliac artery
- internal iliac artery
- some branches directly from the aorta
–> If only one blood supply gets blocked, nothing functions anymore
How is urine transported down the ureters?
By peristaltic contraction of SM
Where do the sphincters of the ureters sit?
What is their relevance?
3 sites of ureteric constriction:
- pelviuretericjunction
- where ureter crosses pelvic brim
- where ureter traverses bladder wall
–> often sites where renal stones get trapped and cause pain
Which epithelium lines the ureters and the bladder?
Specialised transitional endothelium/ urothelium
- very tight junctions ! –> impermeable to water
- Look stratified when relaxed but arent!
- When stretched: show simple epithelium

Where does the bladder sit?
In the pelvis, below the peritoneum
But when filled:
Can reach into the abdominal cavity, pushes peritoneum away to also allow a direct catheter

What is the shape of the bladder?
•Triangular pyramid with apex pointing anteriorly and base posteriorly
Superior surface expands when bladder filled

What is the trigone in the bladder?
Triangular stretched part of the bladder between the entrance of the ureters and exit of the urethra
–> most bladder cancers occur in this region

By which structure is the bladder being held in place in males and females?
Females:
Pubovesical ligament around the urethra
Males:
Puboprostatic ligament around the prostate

What is the difference between the two sphincters of the bladder?
Where do they sit in males and females?
1. Internal/ Sphincter vesicae
- Smooth muscle –> involuntary control via reflex opening in response to wall tension
- At the neck of the bladder
- Relaxed by PNS, contracts by SNS innervation
2. External/ Sphincter urethrae
- Striated muscle –> voluntary control can be learned
- In perineum (Perineal membrane)
–> In Females: right below internal sphincter, in males below the prostate gland

What is the difference between the male and the female urethra?
The male urethra is way longer and has almost two right angles within
Femal is short and straight
Also, parts have different names

How is the lymph drainage of the urinary system organised?
Lymph basically follows arterial supply












































