Tuberculosis and drug resistant TB: A global health prospective Flashcards
What is TB?
TB is the 13th leading cause of death worldwide
since 2007 - leading cause of death from a single infectious agent
(before COVID-19)
ranking above HIV/AIDS and malaria
WHO declared TB a global health emergency in 2003
Define TB and the causal agent
a contagious, debilitating (consuming) bacterial disease
spread by airborne droplets from an infected person
Caused by a bacterium
(Mycobacterium tuberculosis)
slow growing, difficult to kill due to its
Lipid rich waxy outer cell wall coat
- Hard to treat by standard antibiotics
- coughing speaking sneezing, you can infect someone with TB
- Generation time of 24hrs
Left untreated, one person with tuberculosis
will infect 10-15 people (R0). Governments try to keep R under 1
R value of TB is between 15 and 20
Controversial because it takes years to find out whether someone has the disease or not
Describe the infectious dose, incubation and Colonization
Mycobacterium tuberculosis has an incredibly low infectious dose of less than 10 microorganisms.
These bacteria have a long incubation period of two to twelve weeks with a range from 2 weeks to decades
This bacteria, having the ability to be latent or cause disease, is what causes this range.
Mycobacterium tuberculosis that infects the lungs is inhaled by the host and engulfed by the macrophages of the alveoli.
These bacteria can now lay dormant or begin to reproduce inside the macrophages, which triggers the infection to occur.
What are the percentages of pulmonary and extrapulmonary TB?
- M.tuberculosis can infect many parts of the body
- 85% pulmonary TB
- 15% extra-pulmonary TB
- Like interstitial fluid
In HIV infected patients, only 30% of cases are pulmonary TB.
If someone is HIV ++, then they have a higher rate of non pulmonary TB
Where are the places that TB could infect?
Spread of infection by haematogenous spread (spread
Via blood)
Pleural disease
Lymph nodes – scrofula
Pericardial
Skeletal –Potts disease
Genitourinary
Gut
Peritoneal
Miliary
Meningeal
What are the characteristics of a pulmonary TB infection on an x-ray?
Multiple cavities
Circular holes-> due to necrotic tissue caused by bacteria
Thickening of lymph nodes
TB maybe located in one particular section, instead of multiple
What is miliary TB?
Miliary tuberculosis is a potentially fatal form of the disseminated disease due to the hematogenous spread of tubercle bacilli to the lungs, and other organs. It results in the formation of millet seed-sized (1 to 2 mm) tuberculous foci.
Comes up differently under chest xray
Normal TB= encapsulated]
Milliary= disseminated
Acute miliary TB is seen under 40 years of age. Most of the patients present with constitutional symptoms or can have signs and symptoms related to one organ owing to the systemic nature of the disease. Evening rise of temperature and night sweats of 1-2 weeks duration are classically described, although a patient can have early morning fever spikes.
What is Potts Disease?
Pott disease, also known as tuberculous spondylitis, is a classic presentation of extrapulmonary tuberculosis (TB).
It is associated with significant morbidity and can lead to severe functional impairment
Pott disease, or tuberculosis of the spine, has recently shown a significant resurgence in developed nations secondary to global migration. Concurrent with this phenomenon, multidrug-resistant bacterial strains of tuberculosis have been increasing in developing nations over the past decades.
What is a Scrofula?
Scrofula is a condition in which the bacteria that causes tuberculosis causes symptoms outside the lungs.
This usually takes the form of inflamed and irritated lymph nodes in the neck.
Doctors also call scrofula “cervical tuberculous lymphadenitis”: Cervical refers to the neck.
Describe the mechanism of m.tuberculosis,
including
exposure, to latency, to reactivation to active disease
About 30% of people are infected in the presence of TB aerosol
Of that 30%, only 5% go on to progress to active TB Everyone else goes into latency (no disease but they areTB infected)
Of these latent infections, you can diagnose via Mantoux test(hyperactivity of TB antigens) or blood test
Positive test= hypersensitivity to TB antigens
If you have latent Tb, you have a 10% lifetime risk of reactivation to active TB
Always a reservoir of infection
We don’t know is whether latent TB is driven by immunological protection
However immunosuppression increases the chances of reactivation to activation of TB by 5% by year
The spread of TB is mainly driven by pulmonary Tb
It is very difficult to spread spinal TB
What is latent TB?
Latent tuberculosis infection (LTBI) is defined as a state of persistent immune response to stimulation by
Mycobacterium tuberculosis antigens without evidence of clinically manifested active tuberculosis (TB) disease. Individuals with LTBI represent a reservoir for active TB cases
How many people are infected with latent TB?
1/3 world’s population infected
BCG TB vaccine is largely ineffective for adult pulmonary disease
Preventive drug treatment possible but not practical
Antibiotics don’t work on latent TB
Not wise to provide antibiotics to the world due to Antibiotic resistance, Cost production and possible
Reactivation many years later
What are risk factors for reactivation of latent TB?
- reactivation occurring only when the immunity of the host is compromised.
- Malnutrition
- Poverty
- Immunosuppression
- Old age
- People become
partially
immunosupressed - Poor health
- HIV
Poverty, immunosuppression and malnutrition are liked with TB
What is the diagnosis of Pulmonary TB?
Blood:
Interferon (IFN)-gamma blood test.
- T-cell response to Mtb proteins
Interferon-γ release assays (IGRAs) depend on this immune reaction involving T helper cells to detect latent TB through quantification. Fresh blood samples are mixed with antigens and controls to test to determine if an individual has indeed contracted an infection.
Mantoux test
Chest X-ray: CT scanning
Sputum/ culture
GeneXpert–PCR
Bronchoscopy
Biopsy
How to significance of diagnosing TB via sputum?
Sputum: Cough or induced
- Smear/ culture
Sputum smear microscopy remains the most common way to diagnose pulmonary TB. Depending on the report and method used, smear microscopy can accurately detect TB in 20% to 80% (using fluorescence microscopy methods) of TB cases.
Limitations:
can only be used to diagnose TB when sputum has sufficient bacillary load, and it cannot detect drug resistance.
Thus, HIV-associated TB often goes undetected because people living with HIV (PLHIV), especially those with severe immunosuppression, generally have very low numbers of bacilli.
What is the significance of GeneXpert?
- Xpert is more sensitive than sputum smear microscopy in detecting TB, and it has similar accuracy as culture.5-6
- Moreover, its ability to detect smear-negative TB provides a significant advantage, especially for PLHIV.
- , its ability to detect RIF-resistant TB in less than 2 hours significantly improves the likelihood of timely treatment initiation. (Conventional culture and drug-susceptibility testing [DST] are still required to complete the drug-resistance profile and to monitor treatment.)
Limitations of GeneXpert?
Xpert does cost more than smear microscopy; it requires a machine that currently costs US$17,000 and cartridges that cost US$9.98 for each test, in addition to human resource and other running costs.
It also has operational limitations, such as the need for a sustained power supply.
However, Xpert is intended to be used at facilities close to the patient to reduce the time to diagnosis and TB treatment initiation.
What is the Mantoux test? What are the principles of the The Mantoux tuberculin skin test (TST) ?
The Mantoux tuberculin skin test (TST) is one method of determining whether a person is infected with Mycobacterium tuberculosis. Reliable administration and reading of the TST requires standardization of procedures, training, supervision, and practice.
Inject with PPD (or purified protein derivative)
Strong response= more likely that you are progressing towards more active disease
More antigen around
However, reactivity does not mean disease. It just means exposure.
What are the principles of the Mantoux test?
The reaction to intracutaneously injected tuberculin is the classic example of a delayed (cellular) hypersensitivity reaction.
T-cells sensitized by prior infection are recruited to the skin site where they release lymphokines.
These lymphokines induce induration through local vasodilatation, oedema, fibrin deposition, and recruitment of other inflammatory cells to the area.
Features of the reaction include (1) its delayed course, reaching a peak more than 24 h after injection of the antigen; (2) its indurated character; and (3) its occasional vesiculation and necrosis.
What is the BCG Vaccine?
This is an attenuated vaccine
Attenuated M.bovis Bacillus Calmette-Guerin
The most Heavily used vaccine in medical history
Until the COVID vacciens
Given Usually to infants or in early childhood
Protects against disseminated primary infection
Ineffective against reactivation adult TB
Poor data to show that BCG shows any effect on adults
Describe the graph showing TB prevention in terms of the USAGE of the BCG vaccine.
In North America (Particularly in USA & Canada) AND Italy, the BCG vaccine is used for specific groups
For most of the old world (barring western europe), South America (barring Ecuador), Microasia, Greenland and Mexico, the BCG is a vaccination that is utilised for all.
For Western Europe (like the UK, France, Spain,) and Oceania (Australia, New Zealand) etc… the BCG vaccine used to be used for ALL children.
Describe the graph showing TB prevention in terms of the coverage of the BCG vaccine.
USA, Canada, Greenland, Western Europe and Australia have no data
For the majority of S. America, SSA, and Eurasia, , the coverage of the BCG vaccine is 90-100%.
Countries in central Africa, South Africa (the country) and Microasia, have a 50-89% coverage of the BCG vaccine.
Why does the BCG vaccine fail?
Protection ranges from 0-80% in different parts of the world
Maybe Environmental/genetic influences
Vaccination is given to infants but protection only lasts for about 15 years
- Strong protection against childhood TB
- little against the adult infectious form
- risk of disseminating infections
Boost with BCG does not work
-In young adults and teens
What was TB treatment like before the 1950s?
Before the ’50s:
The old way was taking people to the sanatorium (if you were rich)
There you got good clean air, good nutrition and lung exercise
However, there was a greater than 65% mortality rate.
Thus treatment DID NOT WORK
What is the 1943 to treat TB?
- Selman Waxman invented Streptomycin
You must inject everyday
TB rapidly became resistant to the 1 drug (bacilli became resistant)
10,000,000,000 bacteria mutating DNA
(unique waxy cell wall, therefore it doesn’t expose itself to innate immunity, therefore no septic shock. Therefore nobody dies after big exposure to TB )
After bacteria grows and divides it mutates, therefore easy resistance could occur
The bacteria randomly selects for the advantageous gene to resist streptomycin
What is the post-1973 way to treat TB?
ANTIBIOTICS!
4 drug combination trials
Standard short course= 6 months
There are 4 drugs: Isoniazid (H), Rifampicin (R) , Pyrazinamide (Z), Ethambutol (E)
Short standard course:
Intensive phase= RHZE for 2 months
Continuation phase= RH for 4 months
This is over 95% effective and prevented resistance
Some cases, the short course may last for longer. E.g. patients with cavities on the chest x ray and +ve sputum cultures at 2 months
should have treatment extended to 9 months if you have meningeal TB or bone TB.
Why did the 4 drug therapy of Izonaizid, Rifampicin, Pyrazinamide and ethambutol prevent resistance?
You need to give 3-4 antibiotics at the same time to overcome the statistical chance of selecting for a pre-existing mutant
The chance of selecting a mutant that is resistant to all 4 drugs is low
Combining 4 drugs overcame selecting for resistance
Why does TB therapy take 6 months?
As bacteria grows, they develop a persister phenotype: metabolic change where bacteria no longer are replicating, but are still metabolizing
All these antibiotics kill off actively replicating m.TB rather than persister (non-replicating) TB
M.tuberculosis drug tolerant persisters ?
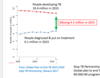
Describe the graph: Colony counts of M. tuberculosis in sputum during treatment with regimens containing isoniazid.
If you culture sputum during treatment, then you have to go on a longer treatment.
I: Actively replicating, rapidly killed by sterilising effect of isoniazid during days 1-4
II: slowly killed,
representing
drug tolerant
persister population
What is the purpose of Latent TB Infection (LTBI) Treatment Regimens? `
These are people with a positive mantoux test. They have been exposed to TB
Purpose : to prevent people with latent TB or exposed to TB from developing disease.
How do you choose between
Isoniazid or Rifampicin to give as a LTBI Treatment?
The Standard Regimen is Isoniazid (INH) daily for 9 months (min 6 months) .
You do this when someone has recently been exposed to the disease
Rifampicin (RIF) is given as the alternative if:
- Someone cannot tolerate INH (Izoniazid)
- Have been exposed to INH-resistant TB
RIF should be given daily for 4 months
RIF should not be used with certain combinations of anti-retroviral (ARV) therapy.
Rifampicin PLUS isoniazid daily for 3-4 months
Why should you give a single drug if you are beginning LTBI Treatment?
There is:
- low bacterial load, (you’ve only been recently exposed)
- low chance of pre-existing mutants
As latent TB must have persister organisms sitting contained by the immune system and untouched by antibiotics
Describe the Global Burden of TB
In 2020:
- *10 million new TB cases per year**
1. 3 million deaths- (plus 0.24 million HIV+ve along with TB)
1/3 of the world’s population is latently infected with TB
People with Multiple drug resistant (MDR-TB) is approx 400 000 people.
People with extensively drug resistant TB (XDR-TB) is approx. 6% of the MDR TB cases (really big threat)
Taken from the WHO TB report 2021
Can you describe the status of the TB epidemic (2018)
10 mill cases annually and has been stable over the years
Burden varies by country. It could be either 5-500 people per 100 000 people. This means that in some countries, there are low TB rates, and in others, there are high TB rates.
The global average is 130 people per 100 000 having TB
1.3 million TB deaths (who are not HIV -ve), which was a 27% reduction from 1.7m in 2000
251,00 deaths in HIV+ve cases which is a 60% reduction from 600 000 since 2000
In all cases of TB, 8.2% are living with HIV (PLHIV)
What is the global distribution of TB?
Unequal global geographic distribution
SE Asia ( 44%)
Africa (24%)
W.Pacific (18%)
8 Countries account for 2/3rds –
India, china, Indonesia, Pakistan, Nigeria, Bangladesh
Gender bias:
Highest burden:
- Male incidence rates are higher
In Men over 15yrs =57% all cases
Women – 32%
Children 11%
Women may not be accessed to healthcare (Somalia, TB is a shameful disease).
Health systems are not notified. You don’t know the true figure
Data can be skewed by people’s behaviours towards HCSs
highest rates in southern africa
Describe the prevalence rates of TB coinfection
S. Africa – co-infection rates HIV + TB = >50%
Risk of developing TB in the 37 million PEOPLE LIVING W/ HIV (PLHIV)
x20 higher than rest of general public)
Old soviet states had little healthcare-> caused outbreak of TB
Some rates are declining due to population increase
In london (west london), some rates of TB are greater than in some parts of the world
What does SDG 3 says?
What does Target 3.3 say?
Ensure healthy lives and promote well being for all at all ages
By 2030, end the epidemics of AIDS, TB, malaria and neglected tropical diseases
and combat hepatitis, water-borne diseases and other communicable diseases
What are the SDG target milestones and the WHO’s End TB strategy?
SDG Target 3.3 – end TB by 2030
Milestones in 2020
35% reduction in TB deaths
20% reduction in TB rates
Targets – for 2030 vs 2015
- 90% reduction in TB deaths
- 80% reduction in TB incidence rate ( new cases/100K )
What are the political declarations in relation to TB in 2018?
Remember that we want to get to the point where no one experiences catastrophic health expenditure in relation to TB treatment. We want to get to the point where we receive TB healthcare. OOP expenditure for TB drugs should be mitigated.
- •treat 40 million in 5 year period 2018 – 2022
- •reach 30 million with TB preventive treatment for LTBI
- •mobilise $13billion for access to TB diagnostics, treatment and care
- •$2b annually for TB research
- THESE ARE MORE AMBITIOUS TARGETS
- Most of these WHO regions are NOT on track to meet milestones
What is the global plan to end TB (between 2016 and 2020)?
Reach at least 90% of all people with TB and place them in appropriate therpy first-time, second time and preventative therapy as required
Reach at least 90% of the key populationd most vulnerable and at risk.
Achieve at least 90% treatment success for all people diagnosed with TB through affordable treatment services, adherance to complete and correct treatment, and social support.

What are the 2020 targets for the reduction of TB incidence rate and TB deaths and the catestrophic costs?
*

What is the impact of COVID-19 on TB services, TB disease burden and progress towards targets?
- Number of new diagnoses has decreased from 7.1 million in 2019 to 5.8 million in 2020 (down by 18%)
- Decreased access to treatment has led to approx 100 000 increase in deaths
- Increase in the number of cases of HIV+ TB coinfection from about 210 000 to 215 000
- TB incidence rates are going to be seen in the next few years
- Treatment for MDRTB has decreased by 15%
- TB preventative treatment has decreased by 21%
- Global spending on TB has decreased diagnostics, treatment, prevention, services
What is the missing 4 million?
“four million people are “missing” and are either not diagnosed or treated or receive care that is of poor quality”
No high burden country achieved both treatment coverage and success
Greatest gap - in treatment coverage
Why was there an incerase in TB in Subsaharan Africa?
The observed increase in TB in sub-Saharan Africa may have resulted from several factors, including civil conflict leading to displacement, overcrowding, famine, and malnutrition. Together with economic decline, these factors have in many cases led to a breakdown in health infrastructure.
diagnose and treat all active cases of TB and close the gap with other regions
What does the UN millennium development goals suggest about TB elimination?
- Elimination target is 1 million per year by 2050
Need a 20% reduction/year by:
- Case Management - currently possible; big impact.
- Need application of technologies to improve control measures
- – diagnostics, treatment and new drugs, vaccines, new technologies
“Sustainable Development Goals (SDGs) target and End TB Strategy require the faster scale-up of existing tools and urgent research on new tools to fight TB”
What is the WHO TB initiative?
The End Tuberculosis Strategy, set ambitious targets for 2020–2035, including 20% reduction in TB incidence and 35% reduction in the absolute number of TB deaths by 2020 and 90% reduction in TB incidence and 95% reduction in TB deaths by 2035, compared with 2015
What is MDR-TB?
Multidrug-resistant TB (MDR TB) is caused by an organism that is resistant to at least isoniazid and rifampin, the two most potent TB drugs. These drugs are used to treat all persons with TB disease.
Rifampicin is a sterilising drug and izoniazid (only works on actively replicating drugs)
Isonaisid is used as a top up if rifampicin doesn’t work
What is the treatment of TB disease?
- Treatment must contain multiple drugs to which organisms are susceptible
- Treatment with a single drug or adding a single drug to failing regimen can lead to the development of drug-resistant TB
- High bacterial load in TB (unique)
- Selection of pre-existing resistant mutants
Is MDR and XDR TB treatable?
- more difficult to treat both MDR and XDR TB
- MDR-TB treatment is difficult because the second-line TB drugs are mostly weak and toxic. Most of these drugs were developed decades ago but hardly ever used because of poor side effect profiles. Because of the weak sterilizing activity of the second-line TB drugs
- XDR TB is resistant to both isoniazid and rifampicin. The most resistant form of TB
- requires the use of “second line” or reserve drugs
- Empirical therapy (guessing)
- more costly ( $10 -50,000 VS $500)
- more toxic side effects
- up to two years
- Cure rates ~ 50% to 70%
What is the shorter MDR-TB regimen ?
One of the most important steps in designing an MDR-TB regimen is taking a detailed history of past TB treatment.
important in patients who have received multiple treatment courses with first- or second-line anti-TB drugs, as there may be omissions or errors in the written medical record.
As a general rule, any drug that has been used in a regimen that did not cure the patient should be considered unlikely to still be effective, even if a recent DST indicates that the patient’s strain is still susceptible.
For example, if the patient previously used ethambutol or pyrazinamide as part of a failed first-line regimen, neither of these drugs should be considered likely to be effective.
All DST results should be compared carefully with the clinical history; DST can be incorrect like any laboratory test. Only DST to first-line anti-TB drugs, injectables, and fluoroquinolones is considered reliable. Laboratory resistance to pyrazinamide, ethionamide, or PAS, combined with a history of use in a failing regimen, however, strongly suggests the drug is ineffective.
At least four second-line anti-TB drugs likely to be effective should be included in the MDR regimen.
How would you diagnose MDRTB?
- GeneXpert could give a diagnosis, however there is molecular DST which could diagnose faster
- There is no “gold standard” for the diagnosis of drug resistance. Molecular testing may detect mutations that confer low levels of resistance that are not detected by culture-based testing but are still clinically significant
- •Specifically, a positive molecular test for rifampicin resistance can be considered diagnostic for MDR-TB, because in most countries, greater than 90% of rifampicin-resistant strains are also resistant to isoniazid.
- A public health strategy of “universal DST,” meaning testing all patients with active TB disease for drug resistance at the start of therapy, is certainly feasible in the near future because of the increasing availability of molecular DST
- DST is cost effective for any country with greater than 1% MDR TB in new patients
- At the current time, however, DST is not widely available in many countries so patients with risk factors for MDR-TB are prioritized for testing
- Household contacts of MDR-TB patients should also be started empirically on treatment if any delay in DST is anticipated
Global MDR-TB
2019 –
- 465,000 cases +110,00 RR-TB
- 240,000 deaths (mostly in Asia) - death rate!!!
- Globally 3.3% of new incident TB are MDR-TB (drug resistant)
- In most cases of MDR-TB, 90% will be latent TB to be stored in the hosts body for 20 years, only to be reactivated.
- 18% of previously treated TB are MDRTB
- 47% of MDR-TB cases worldwide occur in
China, Russia Federation and India
- ~ 50% treatment success rate ?! Improving
- Oblasts and Republics of former Soviet Union –
- Highest proportion of new TB cases as MDRTB:
23. 8–28.3% - 61% of previously treated TB are MDRTB
WHAT is the global burden of XDR TB
- 6.2% of MDR-TB cases are XDR-TB - global average
- 8000 new cases reported in 2016
- Eight countries reported XDR-TB in >10% of MDR-TB
- six of these countries in Eastern Europe and Central Asia
- To date, 121 countries - at least one case of XDR-TB


