Global and Humanitarian Mental Health Flashcards
What is Global Mental Health?
The discipline concerned with addressing this public health crisis, both in low income countries, and in higher income countries of the treatment gap between those who require mental health care and those who do not receive it.
What is the Global Mental Health Treatment Gap?
The “treatment gap” (TG) for mental disorders refers to the difference that exists between the number of people who need care and those who receive care.
The concept is strongly promoted by the World Health Organization and widely used in the context of low- and middle-income countries.
What is the Global Burden of Mental Illness
•Globally, rapid economic, demographic, and epidemiological transitions mean a growth in populations that are living longer, but with greater morbidity and disability.10
Mental disorders are a major driver of the growth of overall morbidity and disability globally
The global burden of mental illness accounts for 32·4% of years lived with disability (YLDs) and 13·0% of disability-adjusted life-years (DALYs)
mental illness is a distant first in global burden of disease in terms of YLDs, and level with cardiovascular and circulatory diseases in terms of DALYs.
The unacceptable apathy of governments and funders of global health must be overcome to mitigate the human, social, and economic costs of mental illness.”
What is the Mental Health Atlas Project 2011?
Mental Health Atlas Project maps mental health resources in the world.
The 2011 version represents the latest global picture of resources available for mental health.
These data are needed at the country level to assess the current situation and to assist in developing plans and at the regional and global levels to develop an aggregate picture of the available mental health resources and the overall needs.
The data was collected in 2011 based on the available data.
How many people work in mental health?
In 2014, 45% of the world’s population lived in a country where there was less than one psychiatrist to serve 100 000 people.
gGlobally, there were 7.7 nurses working in mental health per 100 000 population (WHO; Global Health Observatory Data)
Why are people with mental illness ignored ?
Lack of governmental policy to supress burden of mental illness
Consequently people with mental illness are largely neglected
Pervasive stigma and discrimination
• contributes, at least in part, to the imbalance between the global burden of disease attributable to mental disorders, and the attention these conditions receive.
Stigma, embodied in discriminatory social structures, policy, and legislation, produces a disparity between services geared to physical health and mental health, with lower availability, accessibility, and quality of services for the latter.9
Why is there an underestimation of the global burden of mental illness?
under-estimation to identify five main causes:
- overlap between psychiatric and neurological disorders
- the grouping of suicide and self-harm as a separate category
- conflation of all chronic pain syndromes with musculoskeletal disorders
- exclusion of personality disorders from disease burden calculations
- and inadequate consideration of the contribution of severe mental illness to mortality from associated causes
What is the mental health atlas 2011?
•Mental Health Atlas Project maps mental health resources in the world. The 2011 version represents the latest global picture of resources available for mental health.
These data are needed at the country level to assess the current situation and to assist in developing plans and at the regional and global levels to develop an aggregate picture of the available mental health resources and the overall needs.
The data was collected in 2011 based on the available data.
What is the availability of mental healthcare in afghanistan?
Mental health outpatient facilities= 21
Day treatment facilities- 1
Psychiatric beds= 244
Mental hospital=1
Number reserved for children= 0
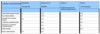
What is the accessibility of mental healthcare in Afhanistan?

Sierra Leone: Availability of mental health care =
Almost all not applicable (including mental health outpatient facilities, say treatment facilities, psychiatric beds in general hospitals
Community residential facilities
Beds in community residential facilities,
Only one mental health hospital
200 beds in that mental health hospital
Sierra leone: Accessibility to mental health care
Only 1 mental hospital.
Approx 1.7 per 100 000 admissions to that mental hospital
No access to mental healthcare for under 18s
What is the right approach to global mental health?
- Global movement for mental health has brought renewed attention to the neglect of people with mental health
- The maltreatment of the mentally ill in many low-income countries is widely reported within psychiatric hospitals, informal healing centres, and family homes
- Could discourage people from seeking mental healthcare
- International agencies have called for the development of legislation and policy to address these abuses
- However these exemplify a ‘top down’ approach to promoting human rights which historically has had a limited impact on those living with mental illness
What are the factors affecting mental health in disasters?
- Disasters have significant impacts on individual lives and society
- Coping with the aftermath of a disaster requires strong mental health and resiliance resources
- Disasters create challenges for mental health
- Effects of disasters can be long lasting + include indirect consequences of the disasterous event
- Working with affected populations in diverse settings and extreme conditions
How would you address mental health in disaster?
•Addressing mental health needs is a disaster in itself (during a disaster)
•Poor disaster management leaves people vulnerable to the after effects of disaster
- There are acute and long term consequences of a natural disaster
- Biggest problems are depression (stress conditions) and anxiety in a refugee camp (this happened in Sudan)
- People take pictures to memorialise incidents (deaths of family members)
- Hardly ever used medication in Haiti earthquake
- Being in contact with family helps (connecting people)
- Religion helps
How would ‘rape’ affect people living in a disaster setting? How would this link into mental health?
- After disasters, there is gender based violence (rape)
- There may be problems when speaking to a male psychiatrist
- In Darfur (Sudan), some women commit suicide after rape
- After rape cases, they place women in safe places (if they go back to their families will they be at risk of being raped again?) and they distribute food, then they advise them to go to the hospital
- Must be very cautious and must use robust methods in diagnosing PTSD, especially among rape.
In an emergency, what is the priorites of which you need to address?
- a. Situational analysis
b. Shelter, food, safety, good information, provide healthcare (Basic needs) - Strengthen emergency response
- Strengthen community response (e.g. natural leaders (like chiefs), authority figures /traditional healers
- Focused non specialised support/ traditional healers (primary care). You train people in mental health. Using the MH GAP manual (an international document not a western document).
Must be mindful of maternal health (post partum depression). Indirect consequences of disaster e.g. displacement, poverty, oncoming gender based violence. If there is treatment of maternal diseases, then there is direct consequences in the health of children.
Basic care is at the bottom of the pyramid, more specialised care is at the top of the pyramid.
What are the effects of mental health treatment
on an individual
- In everywhere, there is a gap between mental health services and the need
- people are treated in primary care level rather than hospitals. It promotes human rights.
- People would rather be treated at their homes because when admitted in a mental health hospital, there is stigma.
- It stops people from having jobs, it stops people from getting married.
- In Turkmenistan, people get put on a register, which affects them for the rest of their life
What is the global burden of mental illness in LMICs?
More than 85% of the world’s population live in the 153 low- and middle-income countries (LMICs)
More than 80% of people who have mental disorders are residing in LMICs, with mental illness and substance abuse disorders presenting as an important cause of disease burden, accounting for 8.8% and 16.6% of the total burden of disease in low-income and lower-middle-income countries,
What are the key challenges facing mental health services in LMICs ?
- •Legislation and policy
- Finances and resources
- Organisation and planning
- Evidence based interventions and training
How is legislation and policy a key challenge in addressing mental health in LMICs?
- Many LMICs lack mental health policies and laws to direct their mental health programmes and services, which is of particular concern especially in Africa and South East Asia
- Family and user associations are present in LMICs but don’t have a strong influence in the development of policy( serious oversight considering that the majority with mental illness in LMICs are supported by family)
T•he mental health policy and the service guidance by the World Health Organization (WHO) describe the necessary steps to follow but does not detail how this can be contextually relevant to a particular culture
- the content of the existing policies have an impact. to what extent do the policies promote integration with the other sectors such as justice, social care, and development of services to ensure a more comprehensive (prevention, promotion, and treatment) and holistic approach to the delivery of mental health services are important
- Although it is important to have policies, it is equally important to ensure that the policies are relevant and beneficial to the local populations. Implementation of the policies should be adequately planned and change process communicated.
Similarly, the attitudes towards mental health among policymakers have a very important role in mental health policy development and funding allocations
How is finances and resources related to mental health treatment gap?
•Globally, the expenditure on mental health is less than US$2 per year per capita across all countries
Many LMICs, including 15 of 19 African countries, allocate less ess than 1% of their health budgets to addressing mental illness.
•Although it is clear that funding allocation to mental health services is inadequate, it would be helpful to have a benchmark of the ideal distribution of budget for general health and mental health for countries to have a guideline to work towards in each country.
How is organisation and planning related to the mental health treatment gap?
- Organisation and planning of mental health services needs focussed attention on the infrastructure and systems that allow easy and early access with referral systems, resources including health personnel, evidence-based treatment guidelines and availability of interventions, a mental health information system, links with other sectors, the extent to which mental health is integrated into health and mental health policies, national strategic plans, and district operating plans.
- Literature highlights the key organisational barriers to mental health care in LMICs being difficulties in access, the competing public health priorities, low investment in mental health services, a paucity of specialist human resources, and resistance to decentralisation
- The availability of geographically spread practical facilities influences access and outcomes in mental health.
Providing treatments in wide rural areas or where transport links are difficult especially when resources are concentrated in one central, usually urban base, is a difficult practical issue common in many developing countries.
It might be difficult, indeed impossible, for some clients to return to a health facility for interventions on a regular basis.
- Alternative strategies using information technology may need to be considered in these situations.
- Integrating mental healthcare with primary care= more accessible to rural communiities
- May not always work because of lack of mental healthcare training
- Training on how to give antipsychotic medications
How can evidence-based intervention & training be involved in the mental health treatment gap?
- Psychotherapeutic interventions are not included in mainstream treatments in many LMICs. This can be attributed to 2 main reasons: lack of resources and inadequate training. Moreover, in some countries, the religion and political landscape have a role to play too
- Despite the strong evidence for its effectiveness, cognitive behaviour therapy (CBT) remains underutilised in clinical settings internationally due to the limited availability of comprehensive training programmes and qualified CBT mental health professional
- In addition, as currently delivered, CBT has been criticised as being West-centric and not in tune with different cultural beliefs
- Although cultural relevance is essential and practice needs to be adapted to fit a variety of cultural backgrounds, this carries its challenges and should follow evidence-based methodology.32 Cost-effectiveness of adapted interventions will need to be evaluated in LMICs. Such adaptation of therapies requires specialised training and research which tends to suffer in economic downturns.
What are opportunities for mental healthcare delivery in LMICs?
•Globalisation and advances in media and communication across the world have resulted in increased awareness and a better understanding of mental health issues by the public in all countries
Despite these developments and increased awareness, in many LMICs and especially in the rural areas, culturally explained attributions to illness determine pathways into care, and often these do not lead to mental health professionals.
Many people with mental illnesses prefer to see a faith healer or religious leader. Although this can present delays in accessing appropriate mental health care, knowledge of local cultural beliefs can suggest different ways of developing services
•Appropriate training in physical and mental health care at primary and secondary care level can help identify mental health problems early, even when they manifest as physical complaints. Also, resources need to be utilised to conduct quality research in different countries to fine-tune the understanding of psychopathology and the effectiveness of various interventions for that particular country
Family support systems and the larger community can be open and accepting of individuals with mental illness in most LMICs. A growing body of evidence through randomised trials now demonstrates that affordable and clinically effective interventions can be provided by the lay health workers in community–a process termed task shifting
How is depression involved in mental health in disasters
•They go to:
- families
- Traditional healers/native doctors/witch doctors
- Religion
•
•Sometimes if you treat depression, then you can alleviate physical conditions
How would you approach GBV and structural violence in disasters?
- Exploitation
- The best thing to do is to promote women in the workforce
- Humanising individuals that have been dehumanised
- This is because some women are not allowed to go an receive healthcare without a male
- Many healthcare workers are male, so women are not allowed to see them alone (either domestic abuse or males think they are protecting women from other males (community issues).
- Structural violence: If a man is seen to take a woman to a male doctor, then the community will shun them.
- Semantics (try to leave normative judgements at the door)
What are the long term effects of disasters on mental health?
Individuals affected by disasters have worse long-term mental health outcomes compared to the non-affected or to the pre-disaster period (war and armed conflicts except terrorism were excluded
What is PTSD?
- Post disaster psychiatric disorder.
- Disaster exposure essential for assessing diagnosis of PTSD: cannot occur without exposure to disaster trauma.
- American Psychiatric Association:
- ‘the person experienced, witnessed, or was confronted with an event or events that involved actual or threatened death or serious injury, or a threat to the physical integrity of self or others’
- and…
- ‘the person’s response involved intense fear, helplessness, or horror’
*
How would you understand PTSD?
- Diagnosed following recurrent episodes of symptoms that commence from 1 month after the disaster
- Delayed onset PTSD (DSM-IV-TR) “onset of symptoms is at least 6 months after the stressor”
- Disasters create both temporary and long lasting mental health problems
How would you determine the risk of developing PTSD from people who have preexisting mental illness?
•Among those with preexisting PTSD, the odds of screening positive for any new mental illness were 11.9 times greater; among those with schizophrenia, 9.1 times greater; and among those with affective disorders, 4.4 times greater.
Persons with preexisting mental illnesses, particularly PTSD, should be considered a high-risk group for poor outcomes after a disaster
How would you work with victims of disasters
You need to know the normal reactions & extreme emotional circumstances as a psychiatric disorder
Account for cross-cultural factors influencing presentation of symptoms
How would you determine cultural sensitivities when treating PTSD?
contradictory, incompatible and divergent attitudes, thoughts, and feelings can develop in response to situations, objects, and other people, and are considered a normal component of cognitive processing
•Diagnosing PTSD has significant moral and societal bearings on local cultures
Disaster mental health needs require spiritually, culturally, and historically sensitive trauma interventions
•Significant impact of stigma of mental illness
How would mental health care present itself in humanitarian crises?
- Mental health needs during humanitarian crises are at risk of being overlooked
- Acute stress reactions (like grief and stress)
- Common mental disorders triggered by the crisis (need to distinguish from emotional distress)
- Pre-existing chronic psychiatric disorders
- Acute health risks, social problems, like substance abuse
Summary
- Mental health in a global context, responding to disasters, is increasing in importance for health care and humanitarian professionals
- There is a need to understand culture to deconstruct critiques such as essential treatment, which can constitute interventions that may be harmful for the individual


