Spirochetes Flashcards
Spirochetes

3 Genera of Spirochetes Pathogenic for Humans
•Treponema
- Syphilis
- Non-venereal or endemic treponematosis
• Leptospira
- Leptospirosis
•Borrelia
- Lyme disease
- Relapsing fever
T. pallidum subsp pallidum
- cause of syphilis
- slender (0.2 µM), only seen using special stains
• dark-field, immunofluorescence, Warthin-Starry
- Few PAMPs, evades host immunity
- Microaerophilic with slow (30 hr) doubling time
- Minimal exogenous DNA
- Not routinely able to be cultured
Other pathogenic treponemes
- 99% related to T. pallidum subsp pallidum
- Not transmitted venereally
- Include
- T. pallidum subsp pretenue (yaws)
- T. pallidum subsp endemicum (bejel)
- T. carateum (pinta)
- Some free-living treponemes are associated with periodontal disease
Syphilis Transmission
• Acquired by sexual contact
- able to penetrate moist mucous membranes
- uncircumcised glans penis; labia, introitus and cervix of women; anal canal; oral mucosa
- may also infect abraded keratinized tissue
- Transplacental transmission
- soon after maternal infection, crosses the maternalfetal circulation to infect the fetus in utero
• Transmission only occurs during the primary & secondary stages
- when the number of organisms is high
Syphilis Epidemiology
- Syphilis remains a significant public health problem.
- While there was a decrease after the introduction of penicillin, there was an increase during the AIDS epidemic in the early 1990’s.
- After another decline, there has been a recent resurgence since 2000, particularly among men who have sex with men (MSM) and among people using drugs. In the latter case, transmission occurs as part of selling sex for drugs.
Syphilis Pathogenesis
- Entry is aided by at least one adhesin that binds to fibronectin and elements of the extracellular matrix.
- In the submucosa, it multiplies slowly and induces minimal tissue reaction. This is probably due to the relative paucity of antigens in the outer membrane.
- The organisms spread from the primary site to the bloodstream and to distant tissues rapidly.
- The immune response is not complete and the organism persists at low levels. Moreover, there is no long lasting immunity and reinfection may occur.
- T. pallidum can infect almost any organ of the body, including the central nervous system (CNS).
- The basic pathologic finding is an endothelial proliferation causing an endarteritis that results in capillary obstruction.
-This accounts for the necrotic ulceration of the primary lesion and subsequent destruction at other sites.
•Although the primary lesion heals spontaneously, the bacteria are already disseminated to other organs by way of local lymph nodes and the bloodstream.
Syphilis Immunity
- The host response in syphilis is imperfect.
- T lymphocytes infiltrate the site of infection within 3 days and are followed by macrophages. The number of treponemes decreases markedly thereafter, likely due to phagocytosis.
- However, some organisms evade phagocytosis and persist.
- The presence of activated lymphocytes and macrophages at the site of the infection may account for the increased risk for HIV-1 infection in those with a primary lesion.
- While antibodies are produced during infection, these are not sufficient to clear infection but are critical tools for diagnosis (see below).
- In the end, a state of latency occurs with organisms persisting and not triggering an inflammatory response, due to their relative lack of surface proteins. At this point, the immune response is not sustained and persons can be reinfected.
Primary Syphilis
- The primary lesion, called the chancre, appears as a single, painless papule at the site of inoculation. It rapidly ulcerates with a hard edge.
- There is often regional arlymphadenopathy that is firm and painless. It usually persists for 4-6 weeks before healing spontaneously.
- This stage often missed in women and in cases of anal exposure

Secondary Syphilis
- Occurs a few weeks or months after primary disease (with some occasional overlap)
- Mild, symmetrical non-pruritic rash that is present on the palms and soles
- Low-grade fever
- Diffuse lymphadenopathy
- Alopecia
- Mucous patches
- Condyloma lata
- Hepatitis

Latent Syphilis
- This occurs in patients who have a positive syphilis serology without any clinical manifestations who have not received prior appropriate antimicrobial therapy.
- It has been arbitrarily divided into early latent syphilis, occurring within one year of infection, and late latent syphilis, where infection has occurred one or more years previously.
- Some clinicians insist on a lumbar puncture to rule out meningitis prior to making this diagnosis, but this is not routinely done.
Tertiary Syphilis
- Currently uncommon
- Cardiovascular
- 10-40 years after initial infection
- endarteritis obliterans of vaso vasorum of large vessels
- aortic regurgitation with saccular aneurysm of ascending aorta
- calcification of the aneurysmal wall
• Late benign syphilis (gumma)
- granulomatous
- indolent, painless masses, sometimes ulcerated
- skin, skeletal system most common
• Late neurosyphilis
Neurosyphilis
•Syphilitic involvement of the central nervous system is now recognized as occurring very soon after infection. It is divided into an asymptomatic and a symptomatic stage
Asymptomatic neurosyphilis
•Asymptomatic neurosyphilis occurs in patients without attributable symptoms but who have an abnormal CSF profile. This may include a nucleated cell pleocytosis, an elevated protein level, and/or a positive non-specific treponemal test, such as the VDRL. There is some debate, but most experts recommend treating asymptomatic neurosyphilis.
Symptomatic neurosyphilis
•Symptomatic neurosyphilis is divided into three types.
- Meningeal syphilis usually presents within one year of infection. Headache, cranial nerve abnormalities, and seizures are common. Uveitis (ocular syphilis) and deafness (otic syphilis) may be seen.
- Meningovascular syphilis is due to an inflammatory vasculitis and occurs later after infection. Stroke involving the middle cerebral artery is the most common manifestation.
- Parenchymatous neurosyphilis is due to late tissue damage and is rarely seen now. General paresis is a cluster of abnormalities including changes in personality, often with delusions of persecution or grandeur, defective judgment, and hyperreflexia.
- The Argyll-Robertson pupil, where pupillary restriction occurs from accommodation but not from light, is a manifestation.
- Tabes dorsalis is due to demyelination of the posterior columns, dorsal roots, and dorsal root ganglia, resulting in a loss of sensation and proprioception. The patient presents with a wide-based gait, joint degeneration (Charcot’s joints), and ulcers of the feet and shins.
Congenital syphilis
- Currently uncommon
- All pregnant women should be tested for syphilis
- if risk high, retested during third trimester
- if positive, treat mother
• Manifestations
- Early (~2-10 weeks)
- infectious
- similar to secondary syphilis in adults
- Late (>2 years)
- non-infectious, subclinical in 60%
- interstitial keratitis
- 8th nerve deafness
- recurrent arthropathy
- Hutchinson’s teeth, mulberry molars, saddle nose, saber shins

Diagnosis of Syphilis - Microscopy and NAATs

Diagnosis of Syphilis - Serology

Syphilis Treatment
•penicillin!
Jarisch-Herxheimer reaction
• Systemic reaction after therapy
- most common with 2° syphilis
- Fever, chills, tachycardia, hypotension 6-8 hr after treatment and lasts ~24 hr - presumed cytokine storm from released lipoproteins of dead treponemes
- Ameliorated with NSAIDs, corticosteroids
- Occurs with treatment of other spirochete infections - e.g. relapsing fever, Lyme disease
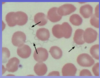
Leptospira genus
- Gram -
- spiral
- aerobic
- The genus Leptospira currently has 23 named species
- previously only L. interrogans recognized as pathogenic
- thin, tightly wound, with hooked ends
Leptospirosis
• Zoonotic infection
- chronic renal infection in rodent reservoirs
• In humans, occurs most commonly in tropics & subtropics
- subsistence farmers
- urban homeless
- camping, water sports
- animal handlers
- Direct or indirect contact with infected urine - soil or water
- Results in humans in a high-grade leptospiral bacillemia
- human TL4 does not recognize leptospiral LPS
- lack of innate immune response
- results in “cytokine storm
Leptospirosis Life Cycle

Leptospirosis Clinical Presentation
- Ranges from mild to life-threatening
- Typically, biphasic
- Incubation stage: 2–20 days
- Acute presentation stage: ~ 1 week
- sudden fever, chills, headache
• associated with leptospiral bacillemia
- muscle pain
- conjunctival suffusion
- multiple organ involvement
• Weil’s syndrome
- jaundice
- hemorrhage
- renal dysfunction
- Convalescent or Immune stage: ~2–3 weeks
- Chronic stage (?): months–years